The 2015 National HIV Prevention Conference Presentation
Download NHPC 2015 presentation slideset: PDF version [PDF – 3 MB] | PowerPoint version [PPT – 6 MB]
Slide 1
High Impact Prevention: Science, Practice, and the Future of HIV
Jonathan Mermin, MD, MPH
National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention
Centers for Disease Control and Prevention
National HIV Prevention Conference
December 7, 2015
Slide 2
Why are we here when these are 100% effective?
Slide 3
Overview
- Science and practice of High Impact Prevention
- State of HIV epidemic including health equity
- High Impact Prevention 2.0
- Importance of monitoring and feedback
Slide 4
High Impact Prevention
Slide 5
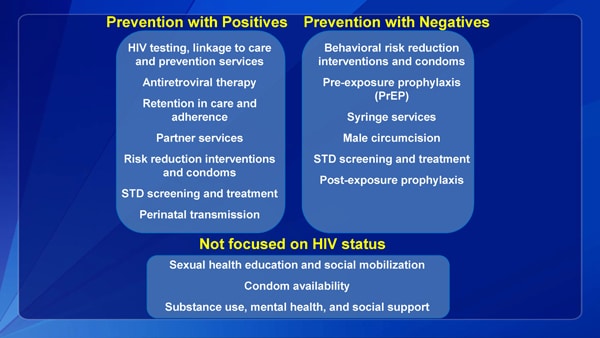
Prevention with Positives
HIV testing, linkage to care and prevention services
Antiretroviral therapy
Retention in care and adherence
Partner services
Risk reduction interventions and condoms
STD screening and treatment
Perinatal transmission
Prevention with Negatives
Behavioral risk reduction interventions and condoms
Pre-exposure prophylaxis (PrEP)
Syringe services
Male circumcision
STD screening and treatment
Post-exposure prophylaxis
Not focused on HIV status
Sexual health education and social mobilization
Condom availability
Substance use, mental health, and social support
Slide 6

High Impact Prevention
Slide 7
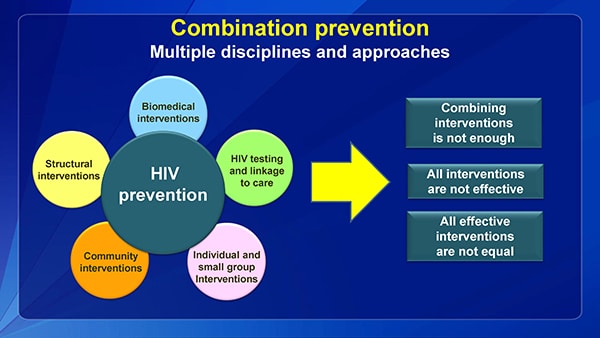
Combination prevention
- Multiple disciplines and approaches:
- Biomedical interventions
- HIV testing and linkage to care
- Individual and small group Interventions
- Community interventions
- Structural interventions
Slide 8
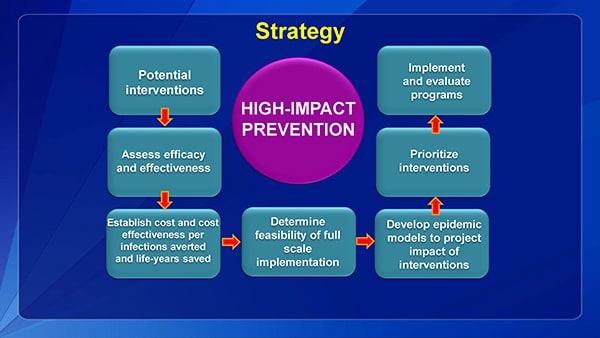
Strategy
Potential interventions
Assess efficacy and effectiveness
Establish cost and cost effectiveness per infections averted and life-years saved
Determine feasibility of full scale implementation
Develop epidemic models to project impact of interventions
Prioritize interventions
Implement and evaluate programs
Slide 9
High Impact Prevention
Slide 10
Implementation of High Impact Prevention
- Program shifts:
- Most activities focused on priority interventions
- Doubling of jurisdictions with integrated HIV prevention and care planning
- Increased activities with PLWHV and MSM, especially black MSM
- Funding for HE/RR reduced from 34% to 11%
- Focus on use of ACA and billing capacity
- About 50% of jurisdictions receive no state HIV prevention resources
Slide 11
Reducing disparities is good public health
- Care and Prevention in U.S. (CAPUS)
- Partnership with CDC, HHS offices, HRSA, SAMHSA
- $45M total funding over 3 years to 8 states
- Eligible states had highest HIV burden among African Americans and Latinos, high AIDS diagnosis rates
- Overcome social determinants that prevent people from reaching a suppressed viral load
- 25% of resources for CBOs
- YMSM and Transgender Persons of Color
- $11 million annually to 34 CBOs to improve care and prevention
- >3,000 new HIV diagnoses anticipated
Slide 12
Has it worked?
Slide 13
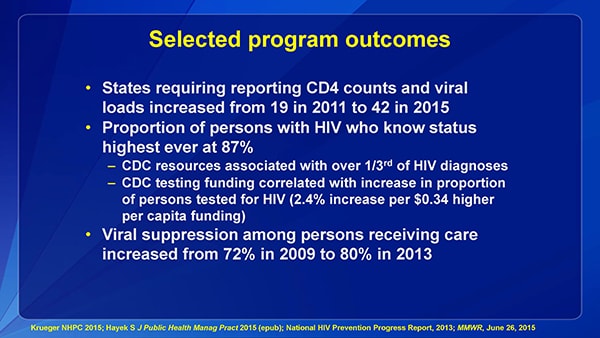
Selected program outcomes
- States requiring reporting CD4 counts and viral loads increased from 19 in 2011 to 42 in 2015
- Proportion of persons with HIV who know status highest ever at 87%
- CDC resources associated with over 1/3rd of HIV diagnoses
- CDC testing funding correlated with increase in proportion of persons tested for HIV (2.4% increase per $0.34 higher per capita funding)
- Viral suppression among persons receiving care increased from 72% in 2009 to 80% in 2013
Slide 14

Some indicators of success
- 2010-14, annual new HIV diagnoses decreased 9%
- 6% reduction in men; 21% in women
- 32% decrease in infections attributed to injection drug use
- 2% decrease in young black MSM, following 114% increase during prior 5 years
- Proportion of persons with HIV aware of status increased, so decreases not due to less testing
- 2010-2013, 9% less mortality–seen in all race/ethnic groups
- 2008-12, mortality among African Americans diagnosed with HIV decreased 28%
- Hispanic/Latinos have lowest mortality among PLWH
Slide 15
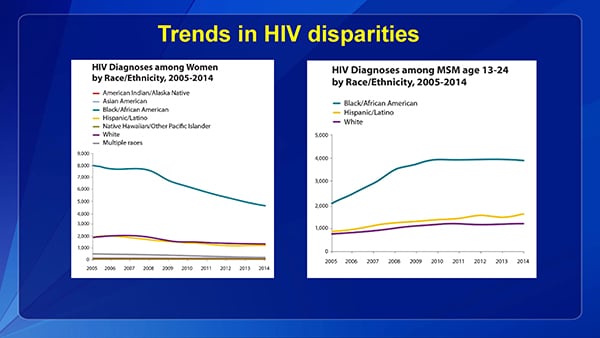
Trends in HIV disparities
Slide 16
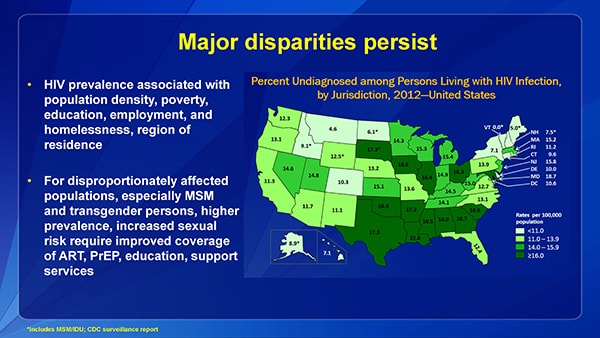
Major disparities persist
- HIV prevalence associated with population density, poverty, education, employment, and homelessness, region of residence
- For disproportionately affected populations, especially MSM and transgender persons, higher prevalence, increased sexual risk require improved coverage of ART, PrEP, education, support services
Slide 17
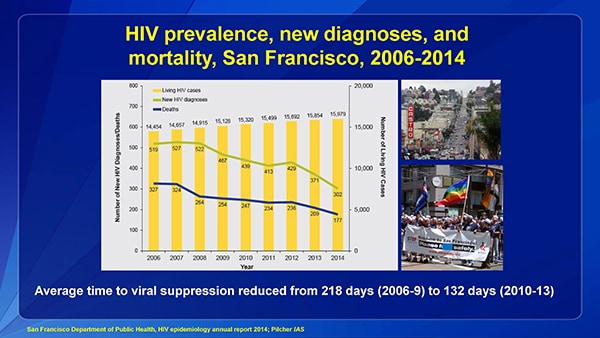
HIV prevalence, new diagnoses, and mortality, San Francisco, 2006-2014
Average time to viral suppression reduced from 218 days (2006-9) to 132 days (2010-13)
Slide 18
High Impact Prevention 2.0
Slide 19
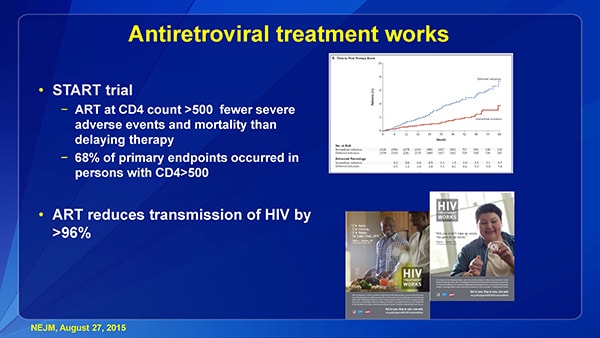
Antiretroviral treatment works
- START trial
- ART at CD4 count >500 fewer severe adverse events and mortality than delaying therapy
- 68% of primary endpoints occurred in persons with CD4>500
- ART reduces transmission of HIV by >96%
Slide 20
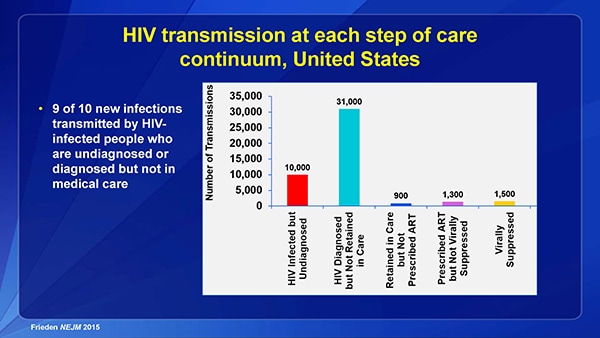
HIV transmission at each step of care continuum, United States
- 9 of 10 new infections transmitted by HIV-infected people who are undiagnosed or diagnosed but not in medical care
Slide 21
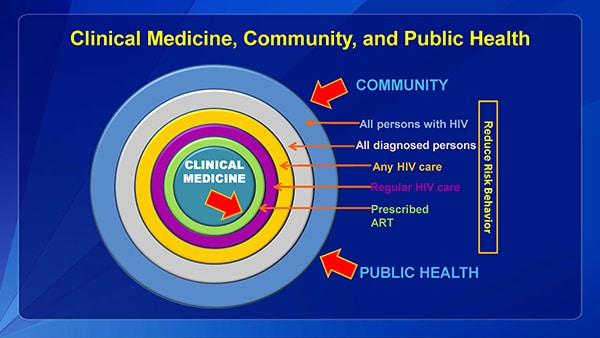
Clinical Medicine, Community, and Public Health
Slide 22
High Impact Prevention
Slide 23
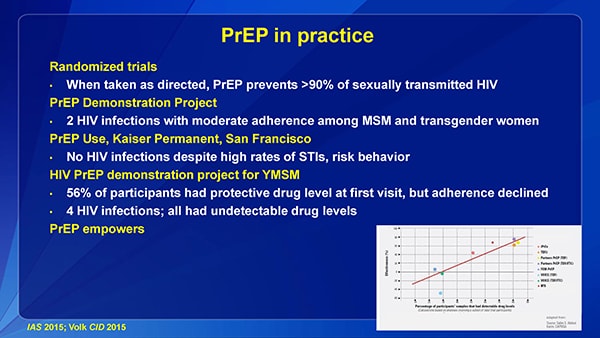
PrEP in practice
Randomized trials
- When taken as directed, PrEP prevents >90% of sexually transmitted HIV
PrEP Demonstration Project
- 2 HIV infections with moderate adherence among MSM and transgender women
PrEP Use, Kaiser Permanent, San Francisco
- No HIV infections despite high rates of STIs, risk behavior
HIV PrEP demonstration project for YMSM
- 56% of participants had protective drug level at first visit, but adherence declined
- 4 HIV infections; all had undetectable drug levels
PrEP empowers
Slide 24
Prevention as healthcare – Healthcare as prevention
- How do we make HIV prevention services, including PrEP, a normative part of healthcare?
- HIV testing as routine as cholesterol testing
- Risk reduction as common as nutrition counseling, foot care for people with diabetes
- Ensure reimbursement systems support routine HIV prevention services within clinics and by CBOs
Slide 25
New activities
- Community-based organization funding
- $216 million over 5 years; 137 organizations
- Highly affected jurisdictions and populations
- Support testing and continuum of care, empowering people to protect themselves, including PrEP
- State and local health department funding focused on MSM and transgender persons of color
- Improve continuum of care, PrEP, risk reduction
- Data to Care
Slide 26

Act Against AIDS new National Testing Campaign
Slide 27
What is the new generation of risk messaging?
- “Protection” is no longer restricted to condoms
- No studies have assessed effectiveness of risk reduction for HIV-negative persons incorporating ART by partner, PrEP, nPEP, male circumcision, and serosorting
- Few studies have assessed new approaches for persons with HIV and their partners
Slide 28
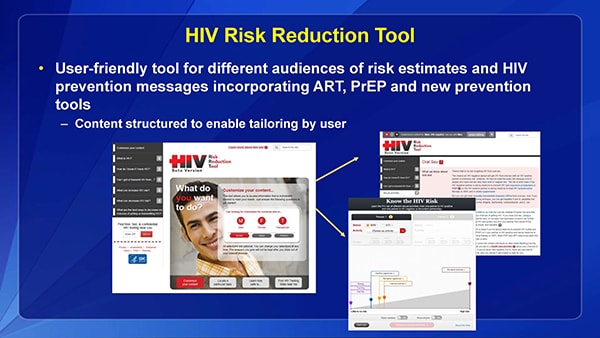
HIV Risk Reduction Tool
- User-friendly tool for different audiences of risk estimates and HIV prevention messages incorporating ART, PrEP and new prevention tools
- Content structured to enable tailoring by user
Slide 29
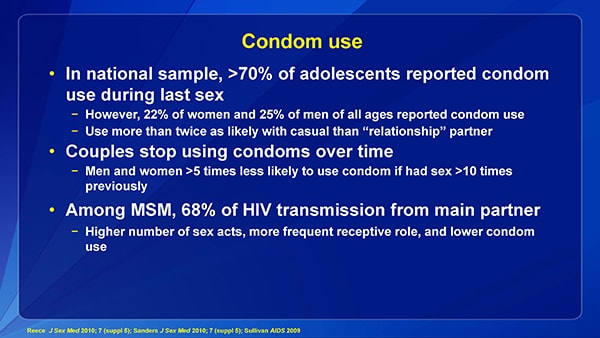
Condom use
- In national sample, >70% of adolescents reported condom use during last sex
- However, 22% of women and 25% of men of all ages reported condom use
- Use more than twice as likely with casual than “relationship” partner
- Couples stop using condoms over time
- Men and women >5 times less likely to use condom if had sex >10 times previously
- Among MSM, 68% of HIV transmission from main partner
- Higher number of sex acts, more frequent receptive role, and lower condom use
Slide 30
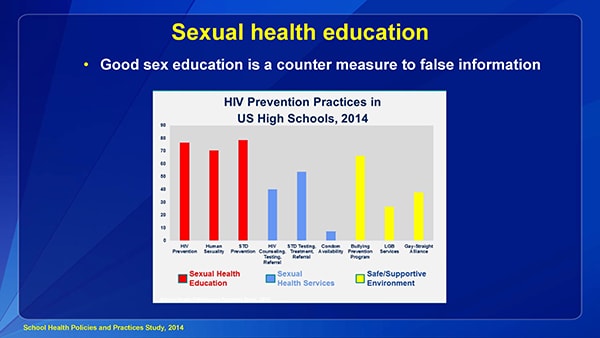
Sexual health education
- Good sex education is a counter measure to false information
High Impact Prevention
Slide 31
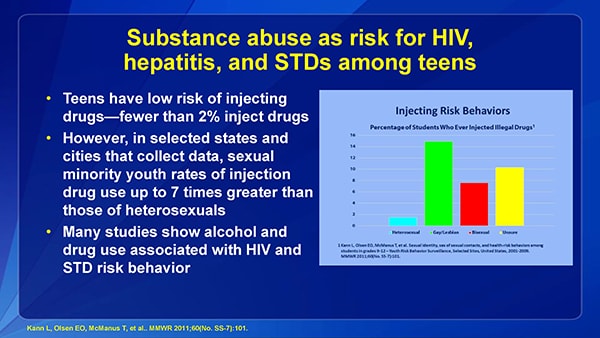
Substance abuse as risk for HIV, hepatitis, and STDs among teens
- Teens have low risk of injecting drugs—fewer than 2% inject drugs
- However, in selected states and cities that collect data, sexual minority youth rates of injection drug use up to 7 times greater than those of heterosexuals
- Many studies show alcohol and drug use associated with HIV and STD risk behavior
Slide 32
High Impact Program Coordination and Service Integration (HIP PCSI)
- Age-based screening for HIV and HCV using computerized clinical decision tools
- Annual STD screening of people with HIV
- STD diagnosis as potential indicator for PrEP, and provision of PrEP at STD clinics
- Integrated partner services
- HIV, HCV, and HBV screening and treatment at drug treatment centers
Slide 33
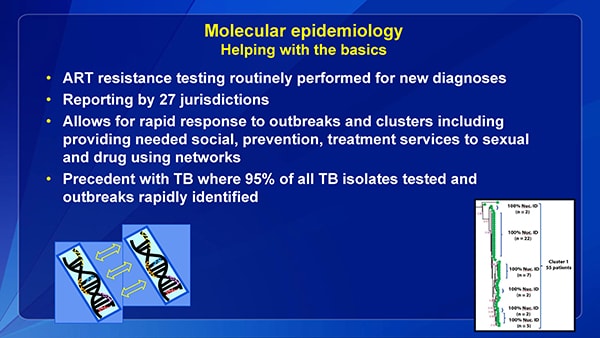
Molecular epidemiology Helping with the basics
- ART resistance testing routinely performed for new diagnoses
- Reporting by 27 jurisdictions
- Allows for rapid response to outbreaks and clusters including providing needed social, prevention, treatment services to sexual and drug using networks
- Precedent with TB where 95% of all TB isolates tested and outbreaks rapidly identified
Slide 34
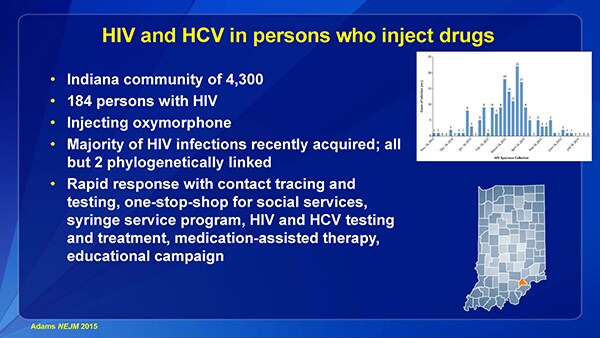
HIV and HCV in persons who inject drugs
- Indiana community of 4,300
- 184 persons with HIV
- Injecting oxymorphone
- Majority of HIV infections recently acquired; all but 2 phylogenetically linked
- Rapid response with contact tracing and testing, one-stop-shop for social services, syringe service program, HIV and HCV testing and treatment, medication-assisted therapy, educational campaign
Slide 35
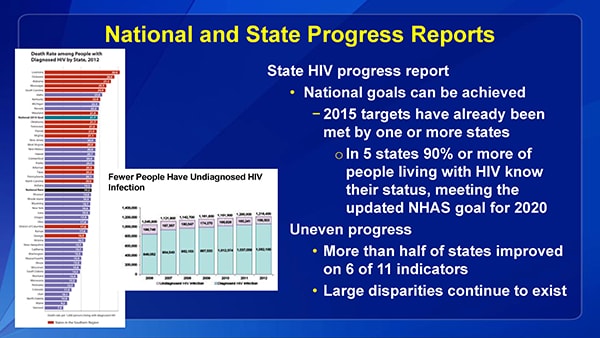
National and State Progress Reports
State HIV progress report
- National goals can be achieved
- 2015 targets have already been met by one or more states
- In 5 states 90% or more of people living with HIV know their status, meeting the updated NHAS goal for 2020
- 2015 targets have already been met by one or more states
Uneven progress
- More than half of states improved on 6 of 11 indicators
- Large disparities continue to exist
Slide 36
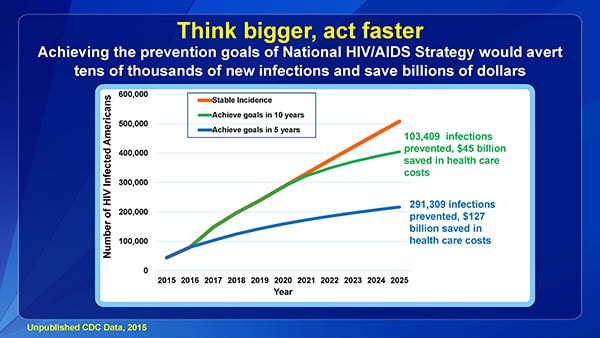
Think bigger, act faster
Achieving the prevention goals of National HIV/AIDS Strategy would avert tens of thousands of new infections and save billions of dollars
Slide 37
Conclusions
- We have turned the corner on HIV, but we are far from achieving success
- Prioritizing the tools and programs that will have the greatest impact is essential
- New science, creative education, sound policy, and innovative programs can make easier, more effective choices
- Future includes integration of treatment, PrEP, molecular epidemiology, and use of data to improve programs
- Think bigger, act faster
Slide 38
Acknowledgments
- Sara Bingham
- Rich Wolitski
- Eugene McCray
- Stephanie Sansom
- Irene Hall
- Janet Cleveland
- David Purcell
- Stephanie Zaza
- Nick DeLuca
- Dawn Smith
- Evin Jacobson
- Patty Dietz
- Norma Harris
- Alexa Oster
- John Brooks