Real Stories from People Living with Sickle Cell Disease: Lametra Scott
Lametra’s Story

In September 2012, Lametra Scott gave birth to a baby boy. She named him Rickey. Before his birth, Lametra had no idea that she carried the sickle cell trait (SCT). It wasn’t until one of her prenatal visits that her doctor told her that she and her son’s father both had SCT, and that their son would have a 25% (or 1 in 4) chance of having sickle cell disease (SCD). The doctor provided her the option to speak with a genetic counselor to determine possible next steps for her pregnancy. Because of her strong faith, Lametra chose to continue the pregnancy.
Getting the Diagnosis
When Rickey was born, his primary care doctor tested him for SCD and Lametra was comforted to learn that her son did not have the disease. She was told that he carried the trait for SCD just like his parents. She and her son’s father immediately breathed a sigh of relief. However, this comforting feeling did not last long, as the State of Tennessee Department of Health soon contacted her and requested that she take Rickey in for confirmatory testing. The health department worker explained to her that a repeat test was needed to confirm Rickey’s initial newborn screening test results, which indicated he had SCD. This was the first time Lametra was made aware of Rickey’s newborn screening results. The test was repeated, and the results showed that Ricky did in fact have SCD. As you can imagine, this news was a devastating blow to the family. “It was like I got the wind knocked out of me,” said Lametra.
Finding and Sharing Resources/Information About SCD
Online and community resources and information about SCD were somewhat limited when Lametra found out about her son’s diagnosis, but she did have access to knowledgeable providers who helped to educate her about the condition. Her hematologist (a blood disorders specialist), Dr. Michael DeBaun, and his nurse, Jeannie Byrd, were an incredible source of information, giving Lametra a handbook for new patients that was very helpful. There was also a sickle cell support organization in the city, but there was not an organization with an initiative that focused on SCD education. This is when Lametra decided to start Breaking The SSickle Cell Cycle Foundation—to increase SCT awareness and to fill the gap in education about SCD. She wanted to be a source of information and support for people who were going through the same things as she was and also help educate others about SCD. Today, Rickey is not shy about sharing his condition with others and even helps his mom educate people about SCD. “Most of the time, he is with me at community SCD awareness events. He helps me pass out SCD flyers. He explained his condition to his kindergarten teacher by saying his “blood cells are sticky and shaped like bananas, not like donuts. They stick together and make my legs hurt.”
Overcoming Challenges Associated with SCD
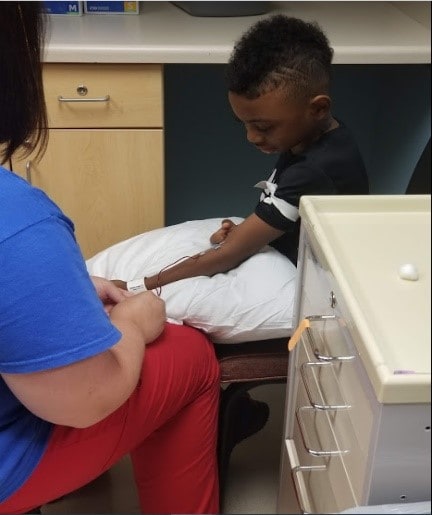
Rickey has experienced dactylitis (inflammation of finger/toe joint), leg/shin, ankle, and back) pain due to his SCD. At age 3, he also required a blood transfusion after developing acute chest syndrome, a common complication of, and leading cause of death for patients with, sickle cell disease.
Lametra has had to explain to Rickey why it is so important that he takes his medicines every day. Potty training was also a challenge according to Lametra. “Because of the need to drink more water to prevent SCD pain episodes, combined with the effects SCD has on the kidneys and their ability to concentrate urine, enuresis (bedwetting) can be a problem for children and teens with SCD. This symptom of SCD can be very discouraging, and weighs heavily on a child who is new to learning how to control bodily functions and trying very hard not to wet themselves.”

Lametra also noted that they have faced certain challenges at school. Whenever she takes Rickey to a new school or program or a friend’s house, she meets with each person (parents, teachers, social workers, nurses, principals, etc.) to discuss SCD. She helps them understand more about Rickey’s condition, informing them of his unique needs. For example, she may let them know that he may need to use the bathroom more frequently due to his increased fluid intake requirements and the effects SCD has on the kidneys. “I try to let him live the life a child wants to live, inclusive of any activities that he finds interest in; he just may have to make some adjustments and/or accommodations for SCD. For example, he needs to stay hydrated during gym class and summer camp and make sure that he does not over-exert himself. I have to make sure he understands his need to take breaks when he needs to and talk to the school staff to make sure they understand his needs too. In addition, they all have to know what to do if he does find himself in a situation where SCD pain is preventing him from participating in regular activities. Another activity in which Rickey can participate, as long as he takes a few extra precautions, is swimming. Rickey started swim lessons at 6 months old. I wanted to make sure he did not fear the water and learned to swim at an early age. I looked for programs and facilities that performed swim lessons in heated pools. I have him wear a wetsuit to help keep his body warm and protect against cold water, which could trigger a sickle cell pain episode. With proper planning and set parameters in place, he participates in regular activities just as other children. There are no limitations to what Rickey can do, but modifications may be needed.”
Tips for Others
When asked what tips she has for others with sickle cell disease, Lametra offered the following:
- Education is key. Educate yourself as much as you can. Don’t believe hearsay. Get reputable information first-hand on how to effectively manage SCD.
- Be an advocate for your own health. Be involved in healthcare decisions.
When asked what advice she has for parents of kids living with sickle cell disease, Lametra offered the following:
- Don’t be afraid to let your child be a child. What works for one, may not work for you. If something poses a problem, find alternatives and allow your child to choose among them. For example, my son wanted to play soccer, which is very aerobic. Instead, he does martial arts, which only requires short bursts of energy, as opposed to activities that require constant running up and down a field. He also plays baseball. Find activities your child can participate in safely and that decrease the chances of leading to a hospital visit. If your child wants to go out and play in the snow, bundle them up and let them go out for 5–10 minutes and then have them come back in again and get warm. With proper planning and modifications, your child can enjoy many of the same things other children do.
- Start the transition process earlier. From pediatric to adult SCD care, start the transition process earlier on before it’s actually time for the transition to occur. Transition is the process of your child moving from a pediatric care provider to an adult care provider. It is also the period when your child becomes more responsible for his or her own health and healthcare. Allow your child to speak during doctor visits. Assist your young adult child in setting up an appointment to meet with the adult care provider early on so that it’s not a cold handoff. This way, you and your child will know what’s expected and it will be easier on everyone.
Where Is She Now?

Dr. Lametra Scott is the Founder and Executive Director of the Breaking the Sickle Cell Cycle Foundation, Inc. She started the foundation in 2015 to provide community support and to educate her peers and providers. She is also a pharmacist with the State of Tennessee. As a guest lecturer, she teaches SCD best treatment practices to rising Doctor of Pharmacy students at the University of Tennessee College of Pharmacy, her alma mater, and Lipscomb University College of Pharmacy. In addition, she has been a guest speaker for Tennessee State University’s Respiratory Therapy Program and has spoken to future social workers at Columbia State Community College about the systematic healthcare disparities SCD patients experience when seeking care. She also works with churches and other organizations to conduct SCT testing.
CDC would like to thank Lametra and her son, Rickey for sharing their story.