Intercountry (International) Adoption Tuberculosis FAQs
As a parent adopting a child from a country outside of the United States, screening your child who has been adopted for tuberculosis (TB) is important to protect both the health of your child and, depending on the age of your child, people with whom your child interacts. The process can be confusing, so we hope answers to these Frequently Asked Questions (FAQs) are helpful to you and your family.
Tuberculosis (TB) is a disease caused by bacteria that are spread from person to person through the air. The general symptoms of TB disease can include coughing, fever, weight loss, and night sweats. TB bacteria get into the air when a person with TB disease in the lungs or throat coughs, speaks, or sings. These bacteria can stay in the air for several hours, depending on the environment. TB usually affects the lungs, but it can also affect other parts of the body, such as the brain, kidneys, or spine. People with TB can die if they do not get treatment. TB disease is different from a latent tuberculosis infection (LTBI). A person with LTBI is infected with the TB bacteria (Mycobacterium tuberculosis), but does not have TB disease. TB disease can be contagious while LTBI is not. It is not possible to get TB from someone with LTBI.
A young child with TB disease can spread TB infection to others, although the chance of that happening is much less likely than it is for a pre-adolescent, adolescent, or adult who has TB disease. Doctors have more concern about a young child possibly spreading TB infection if the child has (1) a chest x-ray showing TB disease in many areas of the lung or one or more cavities (holes caused by TB) in the lung; (2) a forceful and productive (bringing up mucus) cough; or (3) known exposure to a person with multidrug-resistant TB (MDR TB) or extensively drug-resistant TB (XDR TB) (see question #3) when the person with MDR or XDR TB was infectious (could spread TB infection to others). There have been several cases in which a child with TB disease was found to be infectious and spread TB infection to others. These cases highlight the need to use caution when assuming that children with TB disease cannot spread the infection. Learn more about TB in Children.
TB disease is among the top 10 causes of death in the world, and one of the most common diseases in people with weakened immune systems. Although the number of TB cases is declining in the United States, the speed of decline has slowed since 2000. A four-drug regimen is usually used to treat TB disease. This is called first-line treatment. MDR TB is caused by TB bacteria resistant to at least the two best first-line TB drugs (isoniazid and rifampin). This type of TB disease is both difficult and expensive to treat. Drugs used to treat MDR TB are called second-line TB drugs. XDR TB is caused by TB bacteria resistant to the most effective first- and second-line TB drugs. Thus, XDR TB is much more difficult to treat than MDR TB. Although XDR TB is very rare in the United States, it is more common in certain parts of the world and the number of cases appears to be rising worldwide.
TB Medical Exams
As required by US law, any child or adult who is applying for an immigrant visa to enter the United States needs an overseas medical exam, which includes testing for TB. This medical exam must be conducted by a panel physician, a doctor who has an agreement with the local US embassy or consulate to perform the exam according to Technical Instructions (requirements) determined by the US Centers for Disease Control and Prevention (CDC).
According to CDC’s Technical Instructions, several factors affect the choice of TB tests for a child. These include:
- The child’s age
- Whether the child has
- Known HIV infection
- TB signs or symptoms, or
- A personal history of TB disease
- Whether the child is undergoing the panel physician examination in a country with a TB disease rate ≥ 20 TB cases per 100,000 people.
- Whether the child is a known contact (e.g., lived in the same house with) of a person with TB disease.
Interferon Gamma Release Assay (IGRA)
This is a blood test conducted to detect and measure a child’s immune response to TB bacteria. It can have a positive result because of LTBI or TB disease.
- An IGRA is performed routinely in children 2-14 years of age who are examined in countries where TB disease rates are ≥ 20 cases of TB per 100,000 people. In these countries, it is also performed in children younger than 2 years of age with known HIV infection or TB signs or symptoms, or with personal history of TB disease. In countries with a TB disease rate < 20 TB cases per 100,000 people, an IGRA is required in any child younger than 15 years old with known HIV infection, TB signs or symptoms or with personal history of TB disease.
- Children who are a known contact of a person with TB disease also need an IGRA performed.
- If your child has a positive IGRA result, your child will need a chest x-ray to help distinguish between LTBI and TB disease.
A TST is performed only when IGRA is not licensed for use in the country where the overseas medical exam is taking place, or if the child is <2 years of age and needs a test of their immune response to tuberculosis. Like the IGRA, a TST is used to determine if your child has an immune response to TB. A TST can have a positive result because of LTBI or TB disease.
- The test is performed by a healthcare worker, who injects a small amount of fluid (called tuberculin) just under the top layer of the skin of your child’s lower arm.
- After 48-72 hours, your child returns to the healthcare worker, who looks for a raised, hard area or swelling at and around the injection site. A raised area measuring 10 millimeters or more is a positive TST result, indicating that your child needs a chest x-ray to help distinguish between TB infection and TB disease.
This is an x-ray of your child’s lungs that is performed if your child has a positive IGRA or TST, known HIV infection, TB signs or symptoms, or a personal history of TB disease.
Sputum Samples (3 total)
Sputum samples are needed if your child’s chest x-ray suggests TB disease, or if your child has a known HIV infection, or TB signs or symptoms.
- Under the direct observation of a trained healthcare worker, your child produces three samples of sputum (mucus that is coughed up) that are collected and tested for TB bacteria. One sputum sample is collected per day on three separate days.
- A child who is unable to cough up enough sputum for testing has the options of sputum induction or an early morning gastric aspirate.
- In sputum induction, your child is given an inhaler with saline solution (a mixture of salt and water) to help him or her cough up sputum. This can work well if your child is old enough to cooperate with directions.
- In an early morning gastric aspirate, a tube is passed through your child’s nose into his or her stomach and used to collect lung mucus that your child has swallowed. This method can be very helpful if your child is too young to follow directions to cough.
Sputum Smear (3 total)
To confirm whether your child has TB disease, the sputum sample is processed, placed on a microscope slide, and examined for TB bacteria under a microscope. There are several types of bacteria that can resemble TB; therefore a positive smear is only suggestive of TB. Because small amounts of TB bacteria can be missed under a microscope, a negative smear does not confirm that the child does not have TB disease.
Sputum Culture (3 total)
To confirm whether your child has TB disease, the sputum sample is processed, placed in a tube with growth nutrients, and kept in a lab for 8 weeks to watch for the growth of TB bacteria.
- Sputum culture is the most accurate laboratory test that doctors can use to determine whether your child has TB disease.
- If your child has TB disease, the bacteria should grow and be visible within 2-8 weeks, which means a positive diagnosis of TB disease. Because TB bacteria often grow slowly, a full 8 weeks must pass to allow the bacteria to grow.
- If your child does not have TB disease, no bacteria will grow by the end of 8 weeks. This is called a negative TB culture. However, sometimes, even if the laboratory tests are negative, if your child has persistent TB signs or symptoms, the doctor may make a clinical diagnosis of TB disease because not treating TB can have severe consequences.
Drug Susceptibility Test (DST)
If your child has a positive sputum culture, this laboratory test determines which medications can kill the TB bacteria. Based on the results of this test, doctors will be able to select and give your child the TB medications that are most effective against the strain of TB your child has.
In order to determine which TB tests are required for your child, you must first determine what the rate of TB is for the country in which your child is having their panel physician exam. The CDC accepts the World Health Organization’s Tuberculosis country profiles to determine the rate of TB disease for any given country.
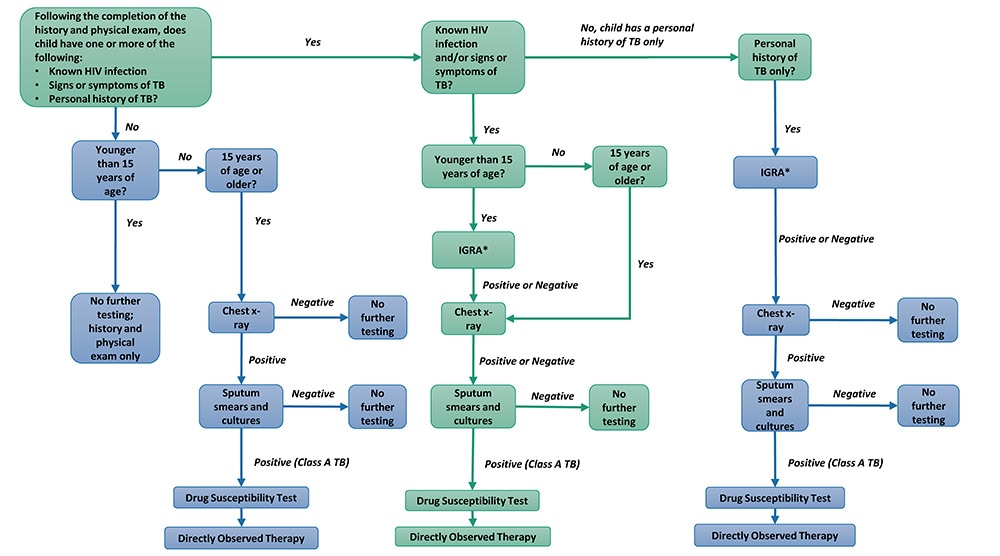
Tuberculosis Algorithm: Countries With Incidence < 20 Cases per 100,000 Population
View Text Description and Overview of Flowchart
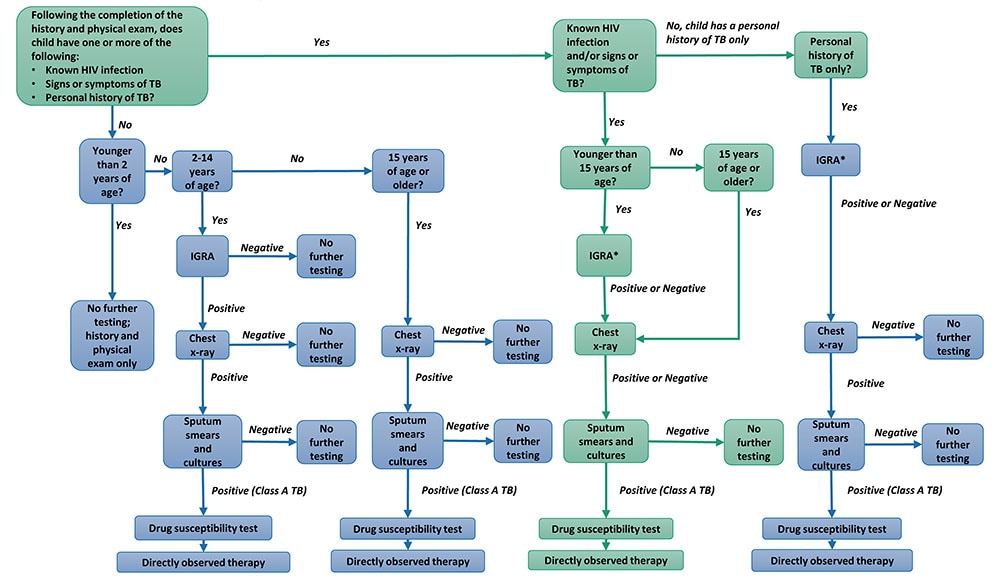
Tuberculosis Algorithm: Countries With Incidence ≥ 20 Cases per 100,000 Population
| TB Test | Time typically required |
|---|---|
| IGRA | less than a week |
| TST | 2-3 days |
| Chest x-ray | 2-3 days |
| Sputum smears | 1-2 days after last of 3 sputa collected |
| Sputum culture | 8 weeks |
| DST | 2-4 weeks |
In recent years, molecular tests for TB (such as the GeneXpert MTB/RIF® and the Hain GenoType® MTBDR plus assay) have been developed to help diagnose patients with TB disease more quickly. While the results of these rapid tests are available more quickly than the results of the sputum culture test, studies have shown that they are less accurate than sputum culture tests. Because a molecular test cannot detect TB as well as a sputum culture, a negative molecular test result does not confirm that your child does not have TB. Therefore, sputum culture testing must still be completed before your child can be cleared for travel to the United States.
TB disease is treated with a combination of antibiotics determined by your child’s strain of TB. If your child is receiving medication to treat TB disease, a healthcare worker or other trained person will watch your child swallow each dose of medication. This treatment is called directly observed therapy (DOT), and is the standard care. DOT typically takes at least 6 months to complete, although longer treatment is needed for MDR or XDR TB.
TB and HIV
TB disease is the leading cause of death among people with known HIV infection and one of the most common diseases for people with weakened immune systems. Additionally, HIV infection is the most common risk factor that can cause LTBI to become TB disease. Without treatment, TB disease can be fatal. Therefore, it is especially important for people with known HIV infection to be tested for TB.
Because HIV infection weakens a person’s immune system, and some of the TB tests measure a person’s immune response to the TB bacteria, people with known HIV infection and TB may
- Test negative on the IGRA, chest x-ray, and sputum smears, BUT
- Test positive on the sputum culture.
- A known HIV infection is not the only reason as to why your child’s sputum smears may be negative but the sputum culture test positive.
Therefore, to accurately determine whether people with known HIV infection have TB disease and to help them receive appropriate medical care as quickly as possible, they are required to undergo multiple tests.
If your child has known HIV infection, he or she must have an IGRA or TST (if younger than 15 years of age) and a chest x-ray before the sputum smears and cultures. Some people with HIV infection and TB disease in the lungs don’t have enough of an immune response to show their lung TB on chest x-ray; others will show TB disease in the lungs on x-ray. For those who do show lung TB disease, the panel site radiologist can compare the panel physician examination chest x-ray with chest x-rays taken during and after treatment to help determine whether the medication your child is taking is effectively curing the TB disease.
Waivers and Exemptions
People who have TB disease and apply to immigrate to the United States are required to complete TB treatment before traveling to the United States. However, for people whose medical situations suggest they would benefit from receiving their TB treatment in the United States, the Department of Homeland Security’s US Citizenship and Immigration Services may grant a Class A waiver allowing them to travel to the United States before the end of their TB treatment. To learn more about Class A conditions, please see the Class A Conditions and the Waiver Process page.
People who have latent TB infection are not infectious, therefore, they do not require treatment for this condition before immigration and do not need a waiver.
Immigrant applicants (including children who have been adopted from other countries) older than age 10 cannot travel to the United States until culture results are ready. However, applicants 10 years of age or younger who require sputum cultures, regardless of HIV infection status, may travel to the United States immediately after sputum smear analysis (while culture results are pending) if none of the following conditions exist:
- Sputum smears are positive for acid-fast bacilli (AFB). If the child could not provide sputum specimens and gastric aspirates were obtained, positive gastric aspirates for AFB do not prevent travel while culture results are pending.
- Chest X-ray that shows―
- One or more cavities, or
- Widespread TB disease in the lungs (especially in the upper area of the lung)
- A forceful and productive cough
- Known contact with a person with MDR or XDR TB who could have spread TB bacteria at the time of contact
Children participating in hosting programs usually visit the United States on tourist visas. Under the Immigration and Nationality Act, people applying for tourist visas are not required to have a medical examination. People becoming permanent US residents—including children who have been adopted—who must have an immigrant visa, are required to have a medical exam, including testing for TB.
You may not have to wait. In many countries, CDC has worked with the adoption service providers, US consular sections, and panel physicians to have children evaluated by a panel physician before the adoption process is complete. The adoption service provider, orphanage, or the consular section of the US Embassy with whom you are working in the home country of your child may be able to help with having the required medical exam performed before you arrive in country.
If your child’s sputum smears and/or cultures show TB bacteria, the panel physician will make a diagnosis of TB disease. Regardless of lab tests, if your child has signs or symptoms of TB disease, or signs of TB disease on the chest x-ray, the panel physician may determine that your child should start treatment for TB disease. In either situation, TB treatment must begin overseas.
TB disease is treated with a combination of antibiotics determined by your child’s strain of TB (determined by drug susceptibility testing). At least 4 drugs are needed in the beginning; fewer drugs may be needed later in the course of treatment. A healthcare worker or other trained person will watch your child swallow each dose of the drugs. This way of providing treatment is called directly observed therapy (DOT). DOT is the most effective way to treat TB and is required for US immigration of people with TB disease. DOT typically takes at least 6 months to complete. The panel physician compares findings on the first chest x-ray with those on a chest x-ray taken during treatment to show whether the drugs are working. Follow-up smears and cultures are also used to show that treatment is working. It is important to note that if a child stops taking the drugs before completion, the child can become sick again. If drugs are not taken correctly, the bacteria that are still alive may become resistant to those drugs. TB that is resistant to drugs is harder and more expensive to treat, and treatment lasts much longer (up to 18 to 24 months).
CDC Technical Instructions have required TB screening of immigrant visa applicants for decades. The most significant change to the Technical Instructions occurred in 2007, when sputum culture testing and directly observed therapy were introduced. In 2018, minor updates included requiring a TB blood test or IGRA (when available) rather than TST when testing for TB infection is needed. The 2018 changes did not significantly alter the timeline, screening procedures, or treatment for applicants.
Additional Resources
References
- Centers for Disease Control and Prevention. Tuberculosis Technical Instructions for Panel Physicians. Cited October 1, 2018.
- Centers for Disease Control and Prevention. Tuberculosis (TB). Cited October 1, 2018.
- U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention Annual Report Fiscal Year 2012 [PDF – 24 pages]. U.S. Department of Health and Human Services. 2012. Cited October 1, 2018.
- Centers for Disease Control and Prevention. Test for Tuberculosis (TB). Cited October 1, 2018.
- Centers for Disease Control and Prevention. Technical Instructions for Panel Physicians and Civil Surgeons. Cited October 1, 2018.