Publications
New Study Investigates Alcohol and Other Substance Use Among Teens Before and During COVID-19
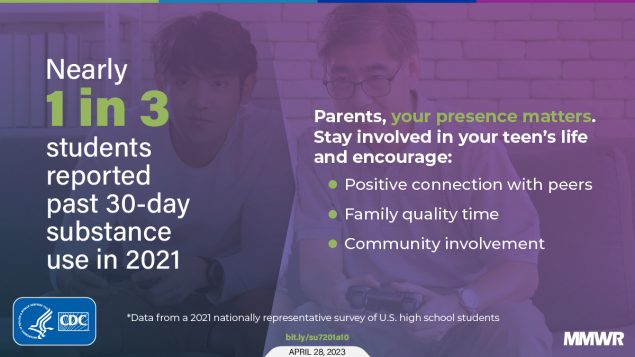
Youth substance use has declined over the past decade, including during the COVID-19 pandemic. However, substance use remains common among U.S. high school students. Supporting tailored policies, programs, and practices that are likely to reduce factors that contribute to teen substance use and promote protective factors may help further decrease substance use among teens and adolescents.