Improving Antibiotic Use in Outpatient Hemodialysis Facilities
Antibiotic Use in Outpatient Hemodialysis
Over 450,000 people across the United States utilize roughly 6,800 facilities to receive hemodialysis treatment on a regular basis. Patients on maintenance hemodialysis have an increased risk of infection due to an impaired immune system and frequent use of catheters or insertion of needles to access the blood stream. Infections are the second leading cause of death among patients on hemodialysis and many of those deaths are caused by sepsis.
Patients on maintenance hemodialysis have high rates of colonization and infection with multidrug-resistant organisms (MDROs). Studies suggest that end-stage renal disease requiring dialysis is a risk factor for Clostridioides difficile infection.
Antibiotic use is critical in this population to treat infections, but it is also important to develop strategies to optimize treatment outcomes and prevent adverse events associated with antibiotic use.
Research shows 30% of patients on maintenance hemodialysis treated in the United States receive intravenous (IV) antibiotics at least once per year. Vancomycin is the most frequently used IV antibiotic in the dialysis setting, accounting for approximately 70% of initial IV antibiotic doses. Some studies have found up to 30% of IV doses administered to patients on maintenance hemodialysis were inappropriate or unnecessary. One common area of inappropriate prescribing is treating ꞵ-lactam susceptible organisms with vancomycin.
Antibiotic Stewardship in Dialysis
CDC and partners published a white paper, Opportunities to Improve Antibiotic Prescribing in Outpatient Hemodialysis Facilities, external iconhighlighting opportunities and strategies to optimize antibiotic use in outpatient hemodialysis facilities.
To establish a framework to improve antibiotic use across different healthcare settings, CDC released the Core Elements of Antibiotic Stewardship. The Core Elements offer providers and facilities a set of principles to improve antibiotic use, optimize patient safety, and improve outcomes. There are no Core Elements specific to the outpatient dialysis setting. However, strategies that have been successful in other settings can be adapted to the outpatient dialysis setting and can improve antibiotic prescribing in this setting.
Some unique characteristics in outpatient dialysis settings that may inform these strategies include:
- There are no well-established standards for diagnosing and treating infections in the hemodialysis population.
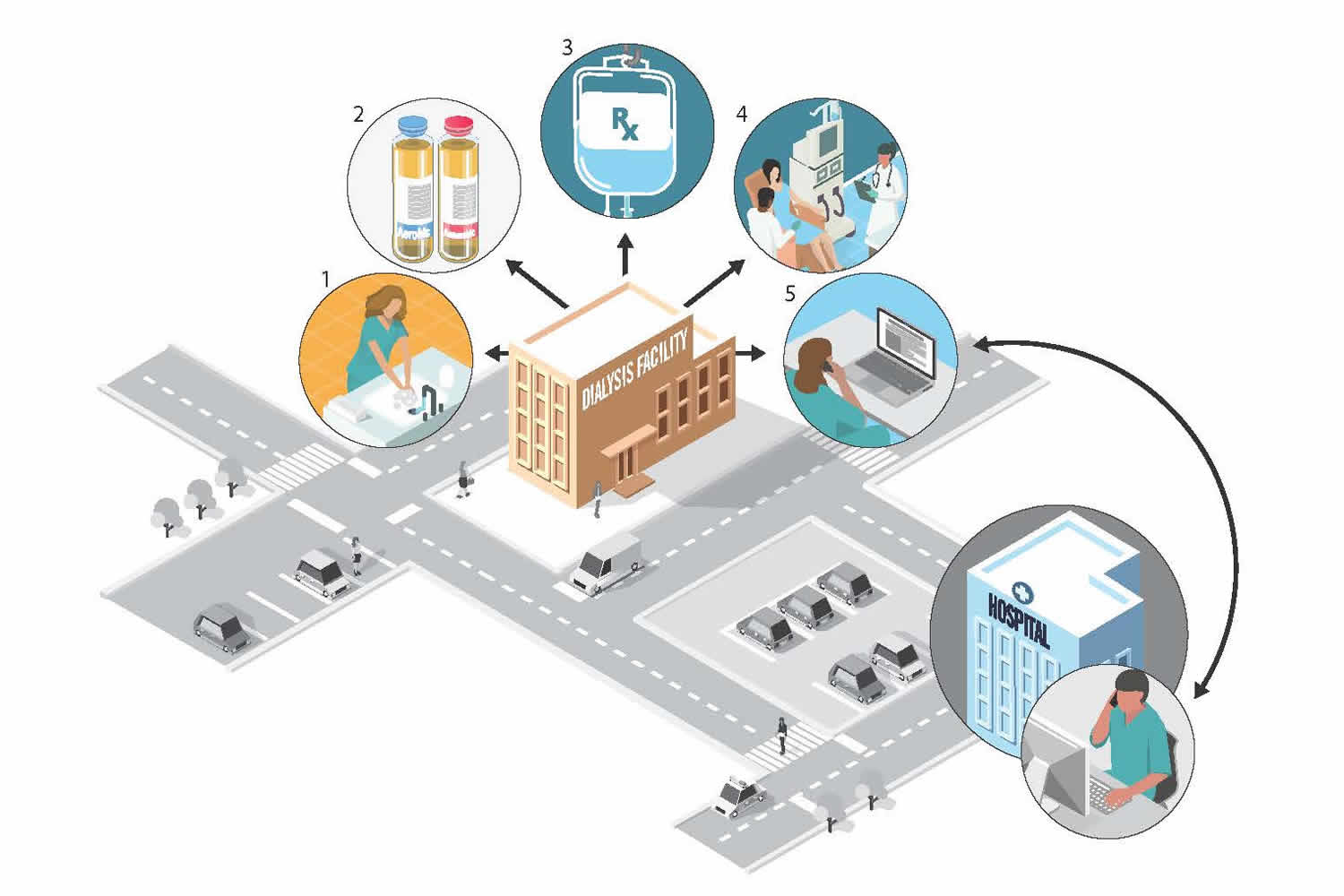
- Nephrologists cannot always be on site during a patient’s dialysis session, therefore reports from nurses and other frontline staff are critical to determining the need to initiate antibiotics.
- Dialysis facilities do not commonly have infectious diseases or pharmacy expertise to assist with antibiotic prescribing.
- Patients often receive care in the acute care setting and communication and transfer of information between the acute care facilities and outpatient dialysis facilities can be challenging and fragmented.
- Dialysis providers may be unaware of antibiotics (particularly oral antibiotics) prescribed in other outpatient or ambulatory settings.
Strategies to Improve Antibiotic Prescribing in Outpatient Dialysis Settings
| Suggested Strategy | Description | Examples |
|---|---|---|
| Infection prevention and sepsis prevention efforts | Engage all staff and patients in preventing infections such as bloodstream infection and vascular access infection. |
|
| Blood culture practices | Implement standardized practices to improve blood culture collection. |
|
| Treatment of methicillin-susceptible Staphylococcus aureus (MSSA) infections | Treat MSSA infections with β-lactams instead of vancomycin for better treatment outcomes. |
|
| Communication with prescribing providers | Implement practices to improve communication between onsite nurses and prescribing physicians or physician extenders. |
|
| Communication across care transitions | Implement practices to improve communication across transitions of care between the outpatient dialysis facility and other healthcare settings. |
|
Strategies Utilized in Other Healthcare Settings
These strategies have been used in other healthcare settings and may be applicable in the outpatient dialysis setting.
- clipboard iconImprove Processes for Detection and Treatment of Common Infections. Several interventions such as clinical decision support protocols for antibiotic initiation, and prospective audits and feedback of antibiotic prescriptions have been shown to improve antibiotic prescribing.
- hands helping solid iconEstablish Relationships with Infectious Diseases Experts. They can provide expertise in the diagnosis and treatment of relevant infections and in developing processes and protocols for antibiotic dosing, selection, adjustment, and de-escalation.
- people iconEngage Leadership to Support Antibiotic Stewardship Interventions. Support from leadership shows that antibiotic stewardship activities are an organizational priority and ensure that needed resources are provided for education of staff and patients, antibiotic prescribing and stewardship expertise, and development and promotion of antibiotic prescribing pathways and protocols.
- book iconProvide Education on Antibiotic Use. Clinician education is critical to any antibiotic stewardship activity. However, education should be paired with other interventions to improve prescribing practices. Some education topics should include: early sepsis prevention and management, antibiotic selection and dosing for empiric treatment of common infections, blood culture collection procedures, and antibiotic adjustment based on microbiology data.
- grid iconIntegrate Antibiotic Stewardship Practices with other Quality Improvement Initiatives. Outpatient dialysis facilities use existing structures and programs to assess quality measures and conduct quality improvement initiatives. Facilities are incentivized by the Centers for Medicare & Medicaid Services (CMS) to report bloodstream infections to NHSN, and are mandated by CMS to have monthly Quality Assessment and Performance Improvement (QAPI) program meetings where specific health outcome measures, such as bloodstream infection rates, are reviewed by the medical director and clinical staff.
Additional Resources
Publications on Antibiotic Use and Stewardship Initiatives in Dialysis
- Apata IW, Kabbani S, Neu AM, Kear TM, D’Agata EMC, Levenson DJ, Kliger AS, Hicks LA, Patel PR. Opportunities to Improve Antibiotic Prescribing in Outpatient Hemodialysis Facilities AJKD 2020. https://doi.org/10.1053/j.ajkd.2020.08.011external icon
- Hahn PD, Figgatt M, Peritz T, Coffin SE. Inappropriate intravenous antimicrobial starts: An antimicrobial stewardship metric for hemodialysis facilities. Infect Control Hosp Epidemiol. 2019:1-3.
- D’Agata EMC, Lindberg CC, Lindberg CM, et al. The positive effects of an antimicrobial stewardship program targeting outpatient hemodialysis facilities. Infect Control Hosp Epidemiol. 2018;39(12):1400-1405.
- D’Agata EMC, Tran D, Bautista J, Shemin D, Grima D. Clinical and Economic Benefits of Antimicrobial Stewardship Programs in Hemodialysis Facilities: A Decision Analytic Model. Clin J Am Soc Nephrol. 2018;13(9):1389-1397
- Nguyen DB, Shugart A, Lines C, et al. National Healthcare Safety Network (NHSN) Dialysis Event Surveillance Report for 2014. Clin J Am Soc Nephrol. 2017;12(7):1139-1146.
- Hui K, Nalder M, Buising K, et al. Patterns of use and appropriateness of antibiotics prescribed to patients receiving haemodialysis: an observational study. BMC Nephrol. 2017;18(1):156.
- Snyder GM, Patel PR, Kallen AJ, Strom JA, Tucker JK, D’Agata EM. Factors associated with the receipt of antimicrobials among chronic hemodialysis patients. Am J Infect Control. 2016;44(11):1269-1274.
- Patel PR, Shugart A, Mbaeyi C, et al. Dialysis Event Surveillance Report: National Healthcare Safety Network data summary, January 2007 through April 2011. Am J Infect Control. 2016;44(8):944-947.
- Zvonar R, Natarajan S, Edwards C, Roth V. Assessment of vancomycin use in chronic haemodialysis patients: room for improvement. Nephrol Dial Transplant. 2008;23(11):3690-3695.
- St. Peter WL SC. Outpatient IV antibiotic use in the U.S. hemodialysis population, 1995 to 2007.
- Klevens RM, Edwards JR, Andrus ML, et al. Dialysis Surveillance Report: National Healthcare Safety Network (NHSN)-data summary for 2006. Semin Dial. 2008;21(1):24-28.
- Berman SJ, Johnson EW, Nakatsu C, Alkan M, Chen R, LeDuc J. Burden of infection in patients with end-stage renal disease requiring long-term dialysis. Clin Infect Dis. 2004;39(12):1747-1753.
- Green K, Schulman G, Haas DW, Schaffner W, D’Agata EM. Vancomycin prescribing practices in hospitalized chronic hemodialysis patients. Am J Kidney Dis. 2000;35(1):64-68.