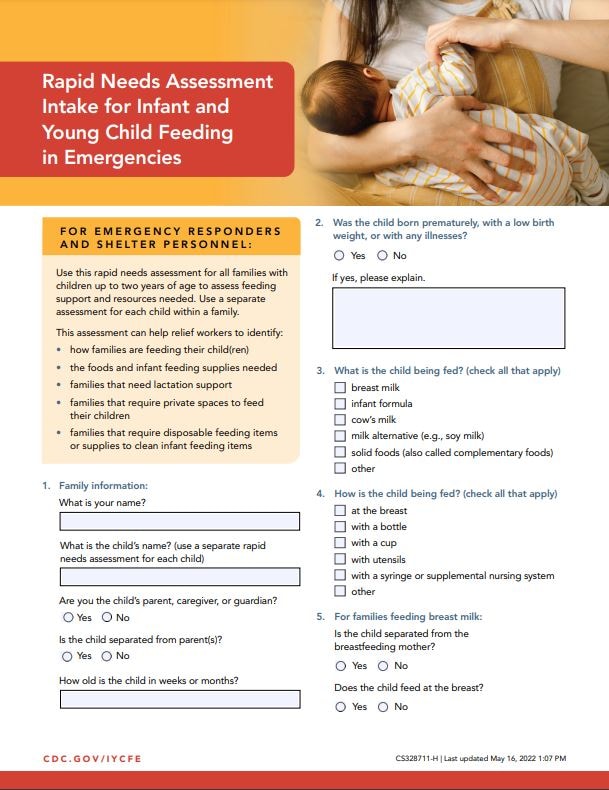
Rapid Needs Assessment Intake for Infant and Young Child Feeding in Emergencies
Download this fillable Rapid Needs Assessment Intake Form [PDF-389KB]. It can be filled out electronically or printed and filled out by hand.
For emergency responders and shelter personnel:
Use this rapid needs assessment for all families with children up to two years of age to assess feeding support and resources needed. Use a separate assessment for each child within a family.
This assessment can help relief workers to identify:
- how families are feeding their child(ren)
- the foods and infant feeding supplies needed
- families that need lactation support
- families that require private spaces to feed their children
- families that require disposable feeding items or supplies to clean infant feeding items
Responses to the questions in the downloadable Rapid Needs Assessment Intake should inform these next steps:
- Reassure breastfeeding women that breastfeeding is the safest way to feed their child during the emergency. Tell these families that they can and should continue to breastfeed and can offer the breast as much as their infant wants.
- Provide families with age-appropriate information about how to continue to safely feed their children during the emergency. Education should be tailored to how they are currently feeding their children and should include guidance for safe cleaning of feeding equipment for all families, including those providing complementary foods. Refer to the Guidelines for Feeding Solid Foods During an Emergency handout in CDC’s IYCF-E toolkit for more information.
- If pasteurized donor human milk is available (e.g., from a human milk bank), ensure that breastfed infants who are separated from their breastfeeding mother and/or do not have access to breast milk are able to receive pasteurized donor human milk.
- If families are using a breast pump to express milk to feed their child, encourage them to breastfeed at the breast more and/or hand express their milk for feedings. Refer to CDC’s handout on hand expression.
- If families rely on an electric breast pump, make sure they have access to electricity and/or batteries to operate the pump, and a refrigerator to store their milk. These families also need access to safe water and cleaning supplies to properly clean the pump part kits after every use. If proper cleaning of breast pumps (manual or electric) is not possible, they should not be used. Contact a lactation support provider to help support the family and teach hand expression.
- If families are using bottles and nipples, or other reusable cups to feed their children breast milk or infant formula, AND safe water and cleaning supplies ARE NOT available, provide disposable cups and instructions on cup feeding. If proper cleaning of infant feeding items such as bottles and nipples is not possible, they should not be used. Refer to CDC’s handout on how to cup feed.
- If families are using bottles and nipples, or other reusable cups to feed their children breast milk or infant formula, AND safe water and cleaning supplies ARE available to clean these items, provide education on proper cleaning practices. Note: Disposable feeding items are preferred in congregate shelter settings to minimize risk of contamination that can make babies sick.
- Tell families how they can get help with infant feeding if they have any concerns or problems.
Concerns requiring further assessment with a trained health professional and or lactation support provider:
- Child appears unwell, thin, or dehydrated (get medical help immediately).
- Child is normally fed breast milk but is separated from breastfeeding mother.
- Child not breastfeeding well (latch, suck, transfer).
- Breastfeeding problems (e.g., plugged ducts, breast infection, thrush, engorgement, slow or difficult let-down, oversupply, use of special equipment like a supplemental nursing system or G-tube).
- Parent/caregiver think child is not eating enough.
- Mother thinks she is not producing enough breast milk for child.
- Breastfeeding family requests infant formula.
- Child is over 6 months of age and family has concerns with feeding the child complementary foods.
- Mother needs to learn how to hand express milk.
- Mother wants to relactate. Relactation is when you start breastfeeding again after having stopped for some time (weeks or months).
- Child has food allergies or dietary restrictions.
View Page In: PDF-389KB
Error processing SSI file
Page last reviewed: September 13, 2022