

|

|

Volume 5:
No. 4, October 2008
ORIGINAL RESEARCH
Characteristics of Young Women
Who Gave Birth in the US-Mexico Border Region, 2005: The Brownsville-Matamoros Sister City Project for Women’s Health
Francisco Gerardo Galván González, MD, Gita G. Mirchandani, PhD, MPH, Jill A. McDonald, PhD, Mauro Ruiz, BS, Alonso Echegollen Guzmán, MD, Brian C. Castrucci, MA, Ginger L. Gossman, PhD, Kayan L. Lewis, PhD
Suggested citation for this article: Galván González
FG, Mirchandani GG, McDonald JA, Ruiz M, Echegollen Guzmán A, Castrucci BC,
et al. Characteristics of young women who gave birth in the US-Mexico border
region, 2005: the Brownsville-Matamoros Sister City Project
for Women’s Health. Prev Chronic Dis 2008;5(4).
http://www.cdc.gov/pcd/issues/2008/
oct/08_0060.htm. Accessed [date].
PEER REVIEWED
Abstract
Introduction
Childbearing during adolescence and young adulthood is associated with adverse effects on health and quality of life. Lowering
birth rates among young women is a binational priority in the US-Mexico border region, yet baseline information about birth rates and pregnancy risk is lacking. Increased understanding of the characteristics of young women
who give birth in the region will help target high-risk groups for sexual and reproductive health services.
Methods
We examined data on reproductive health characteristics collected in hospitals from 456 women aged 24 years
or younger who gave birth from August 21 through November 9, 2005, in Matamoros, Tamaulipas, Mexico, and Cameron County, Texas. We calculated weighted percentages and 95% confidence intervals
(CIs) for each characteristic and adjusted odds ratios
(AORs) for Matamoros and Cameron County women by using multiple logistic regression techniques.
Results
Numbers of births per 1,000 women aged 15 to 19 years and 20 to 24 years were
similar in the 2 communities (110.6 and 190.2 in Matamoros and 97.5 and 213.1 in
Cameron County, respectively). Overall, 38.5% of women experienced cesarean
birth. Matamoros women reported fewer prior pregnancies than did Cameron County
women and were less likely to receive early prenatal care but
more likely to initiate breastfeeding. Few women smoked
before pregnancy, but the prevalence of alcohol use in Cameron County was more than double that of Matamoros. In both communities combined, 34.0% of women used contraception at first sexual intercourse.
Conclusion
Despite geographic proximity,
similar ethnic origin, and comparable birth outcomes, young Mexican and US women
showed different health behavior patterns. Findings suggest possible
pregnancy prevention and health promotion interventions.
Back to top
Introduction
Childbearing and parenting among adolescents and young adult women is associated with adverse effects on health and quality of life for both mother and infant (1,2). The birth rate for young US
women of Hispanic origin is higher than that for young US women overall: in 2006, the birth rate for Hispanic women
aged 15 to 19 years was 83 per 1,000, compared with 42 per 1,000 for all US women in the same age group. The birth rate for Hispanic women
aged 20 to 24 years was 177 per 1,000, compared with 106 per 1,000 for all US women in this age group (3). Adolescent birth rates are high in US counties
on the Mexican border, where Hispanic concentration is high (4,5). In 2004, for example, the birth rate among women aged 15
to 19
years was 62 per 1,000 in Texas and 96 per 1,000 in the border’s southernmost county, Cameron County
(J.
Jackson, MPH, written communication, February 2008).
The birth rate among young Mexican women is also high. Vital statistics data from 2006 indicate a national rate of 74
per 1,000 women aged 15 to 19
years. Similar adolescent birth rates are documented in the border state of Tamaulipas (75
per 1,000), which borders Texas, and in the municipality of Matamoros, Tamaulipas (75
per 1,000), which is directly across the international boundary from Cameron
County (Figure). Birth rates among women aged 20 to 24 years in 2006 were 140 per 1,000 in Mexico,
139 per 1,000 in Tamaulipas, and 126 per 1,000 in Matamoros (6,7).
[
View enlarged image and descriptive text. ]
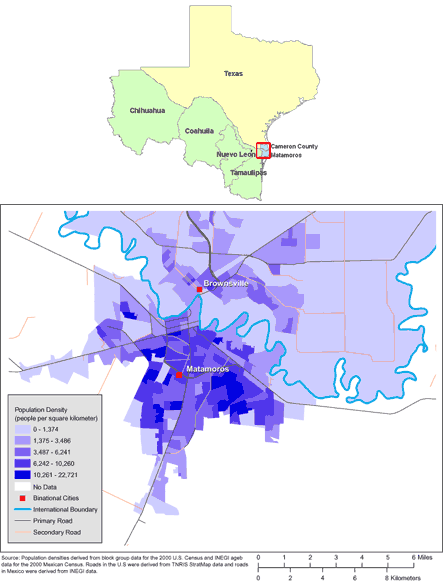
Figure. Maps of the US-Mexico Border Region (Top) and
of Brownsville, Texas, and Matamoros, Tamaulipas, Mexico (Bottom). (The authors
thank Allison Abell Banicki of the Office of Border Health, Texas Department of
State Health Services, for creating the map of the Texas-Mexico border states
and thank Jean W. Parcher, Sylvia N. Wilson, and the United States Geological
Survey [USGS] for providing the map of population density in Brownsville and
Matamoros.)
In part because of these statistics, the United States-Mexico Border Health Commission has set objectives for reducing adolescent birth rates on both sides of the border and improving the delivery of prenatal care to women of all ages by 2010 (8). The target is a 20% reduction
in births among adolescents in the border region of Mexico and a 33% reduction in the border region of the United States (8).
Unfortunately, little more than the overall rates is known about births among adolescents and other young women
in the US-Mexico border region, and the reliability of those rates is unclear, especially in the Mexican states where state governments are actively engaged in campaigns to increase birth registration (9). Such information is critical for planning and evaluating health education and teenage pregnancy prevention programs
created for this population. Insufficient family planning resources are available for adolescents and young women in border communities
(B.R. Smith, MD, MPH, written communication, March 2008).
To provide the information needed for such programs, the Centers for Disease Control and Prevention (CDC) recently developed the Brownsville-Matamoros Sister City Project for Women’s Health (BMSCP), a model for reproductive health risk factor surveillance in border communities, in collaboration with governmental health institutions in Tamaulipas and Texas and other community partners (10). The BMSCP pilot survey, conducted in 2005, covered a range of reproductive and chronic
disease indicators, including data on prepregnancy, prenatal, and birth experiences. The survey interviewed a representative sample of women who gave birth in the municipality of Matamoros or in Cameron County, where the city of Brownsville is. We used the BMSCP data to 1) provide another measure of age-specific birth rates among young women in the 2 communities, 2) describe the sociodemographic and reproductive health characteristics of young women who gave birth in each community and
overall, and 3) compare findings between the 2 communities.
Back to top
Methods
This surveillance pilot project was reviewed for human subjects concerns by CDC and was determined to be “nonresearch” or public health practice. Therefore, institutional review board approval was not required. Data were collected between August 21 and November 9, 2005, through a hospital-based, postpartum survey of women who gave birth in Matamoros or Cameron County (10). Briefly, we used a stratified cluster sampling design to select women for interview who delivered a live infant in either community in a hospital that experienced 100 or more deliveries in 2004. All women who delivered a live infant on selected days were included in the sample. Sampled women were identified through review of
hospital delivery logs. Retrospective review of vital statistics data showed that the sampling approach included 95% of the birth population and that more than 97% of women in each community who delivered live infants in study hospitals on sample days were successfully sampled. Among the 999 women sampled, 947 (95%) completed interviews. In the current analysis, we include only BMSCP respondents aged 24 years or younger (n = 456).
We calculated age-specific birth rates within each community for girls and women aged 10
to 19, 15 to 19, and 20 to 24
years, and then for all girls and women aged 10 to 24 years. The number of women aged
younger than 15 years was too small for separate analysis. Survey data were weighted to approximate the number of women
who gave birth in each community during the 81-day study period. We derived annualized estimates of the number of births in the population in 2005 and corresponding 95% confidence intervals
(CIs) by multiplying the weighted population estimate and associated standard error by 4.51 (365 days/81 study period days). We used age- and sex-specific midyear population estimates for July 1, 2005, as denominators for the rates (11,12).
We calculated birth rate estimates from vital statistics and census data as a comparison. For Cameron County, we used provisional 2005 birth counts, the most recent we could obtain (J. Jackson, MPH, written communication, February 2008). For Matamoros, we used 2006 birth data and population estimates because 2005 birth data were not available (6,7).
Weighted frequencies and proportions were calculated for sociodemographic and reproductive health characteristics for all women in Matamoros, Cameron County, and the combined sample. We analyzed 9 sociodemographic variables from the survey: age, ethnicity, place of birth, interview language, marital status, education, employment status, health care coverage before pregnancy, and health care coverage during pregnancy. Ethnicity was based on self-report in Cameron County, whereas all mothers
who lived in Mexico were coded as being Hispanic. Interview language was coded as Spanish if the respondent opted for a Spanish-language interview or used Spanish at any point during the interview. Employment status referenced the 3 months
before pregnancy; we classified respondents as 1) employed (employed for wages or self-employed), 2) unemployed (out of work), or 3) not in the labor market (ie, homemaker, student, retired, or unable to work). Small numbers prevented analyses of
these variables by age group. We tested for sociodemographic differences between the 2 communities using the Pearson
χ2 test, with a P value of ≤.05 as the cutoff for statistical significance.
We examined 16 reproductive health characteristics, including 6 pregnancy characteristics: gravidity, intention of pregnancy, low birth weight (<2,500 g), preterm birth (<37 weeks’ gestation), method of delivery, and breastfeeding initiation. Unintended pregnancy was defined as a pregnancy the respondent said she would have liked to have later or not at all. Women who responded that they began prenatal care within the first 13 weeks of pregnancy were defined as having had early
prenatal care. Those responding yes to the question, “During any of your prenatal care visits, did a doctor, nurse, or other health care worker talk with you about birth control methods to use after your pregnancy?” were coded as having received postpartum contraception counseling.
Respondents were asked about risk behavior and knowledge related to contraception, HIV, smoking and drinking, and history of a
Papanicolaou (Pap) test. Depending on their unprompted responses to the question, “What can a person do to protect himself or herself from getting HIV/AIDS?” we coded each respondent as knowing both,
1, or neither highly effective method of HIV prevention: 1) using a condom and 2) limiting sex/staying faithful to
a single partner. We used an aggregate measure of “high-risk behavior,”
defined as experiencing 1 or more of the following during the previous year: 1) intravenous drug use, 2) treatment for a sexually transmitted infection (STI), and 3)
more than 2 sex partners. Respondents were not asked to identify which behaviors applied to them but only to respond positively if 1 or more applied. Smoking and alcohol status were obtained from questions that asked how many cigarettes were smoked on an average day and how many drinks were consumed in an average
week during the 3 months before pregnancy. We coded women as smokers or drinkers if they reported any level of consumption. Most survey questions were taken or adapted from established surveys (10). Birth weight was obtained from the hospital record, and gestational age was obtained from the birth certificate. All other variables were derived from the survey questionnaire.
We computed unadjusted odds ratios (ORs), 95% CIs, and P values for the associations between place of residence and each reproductive health characteristic. We used multivariate logistic regression techniques to calculate the adjusted odds ratio (AOR), 95% CI, and P value for each characteristic, adjusted for an
a priori set of sociodemographic
variables (13), including age (continuous), ethnicity (2-category), marital
status (3-category), education (3-category), and health care coverage before
pregnancy (2-category). For characteristics with more than 2 outcome categories,
we used multinomial logistic regression (14). We conducted all analyses with Stata software, version 9 (StataCorp
LP, College Station, Texas), taking survey weights and the complex survey design variables into account.
Back to top
Results
Among the 456 women included in this study, 248 reported living in Mexico and were presumed to be Matamoros residents, and 207 reported living in the United States and were presumed to be residents of Cameron County. One other respondent who delivered in Cameron County had a missing response and was classified as a US resident. Among the women who resided in Mexico, 4% (11/248) delivered in a Cameron County hospital.
Only 1 of 208 Cameron County residents delivered in a Matamoros hospital.
Annual birth rates per 1,000 Matamoros women aged 15 to 19 years and Cameron County women aged 15-19 years were similar
(Table 1). Annual birth rates among women aged 20
to 24
years were approximately twice those in the younger age group for both communities. In Matamoros, the birth rate in each age group as determined by vital statistics fell below the 95% CI of the birth rate derived from the study.
One-third of women in the study were younger than 20 years (Table 2). Ninety-four percent were Hispanic; Mexico was the birthplace of 99.5% of the Matamoros women and 40.4% of the Cameron County women. Matamoros mothers were less educated but were more likely to be married/living together
and to have health care coverage before pregnancy. Overall, approximately two-thirds of women had health care coverage during their pregnancy.
Fewer Matamoros women reported prior pregnancies (Table 3). In each community, fewer than half of the pregnancies were intended. Although Matamoros mothers had
less frequent low-birth-weight and preterm births, these differences were not statistically significant. The proportion of cesarean
births reached almost 40% in each community. Matamoros mothers were 4 times as likely as Cameron County mothers to have initiated breastfeeding by the time of interview.
Virtually all women had some prenatal care (data not shown), but more Cameron County women (69.9%) than Matamoros women (57.9%) had first-trimester prenatal care. Counseling for postpartum contraception was more frequently a part of prenatal care for Matamoros women (69.4%) than for Cameron County women (58.8%).
The mean age at first sexual intercourse among the 440 women who provided a response was 16.9 years in Mexico and 16.5 years in the United States (P = .09). Among women
aged 20 years or younger, the mean ages were 15.8 years in Matamoros and 15.6
years in Cameron County (P = .22) (data not shown).
Women residing in Matamoros were less likely than women residing in Cameron County to use contraception at first sexual intercourse, but the association was attenuated in the adjusted analysis. More Matamoros women than Cameron County women used an intrauterine device (IUD) as their first method of contraception. Barrier methods were the most common choice in each community.
Use of alcohol before pregnancy was more prevalent among Cameron County women. Only 6% of women in each community reported using intravenous drugs, having been treated for an STI, or having had
more than 2 sexual partners in the past year. Fewer women in Mexico reported ever receiving a Pap test.
Back to top
Discussion
One purpose of this study was to compare rates calculated via this sample survey with rates from vital statistics as evidence of the validity of published birth rates in both communities. Results suggest that vital statistics in Matamoros may underestimate the true birth rates. In Cameron County, estimates from the survey and vital statistics were more compatible. This may be in part because
our survey estimates included births to Matamoros residents that occurred in Cameron County. Those
infants may not have received Tamaulipas birth certificates, and Texas does not routinely share birth certificates of infants of nonresident mothers with Tamaulipas. This factor would not have affected Cameron County rates because so few Cameron
County residents gave birth in Mexico, and births to Mexican residents in Cameron County are not counted in the vital statistics rates.
Although birth rates generated by this surveillance system were comparable in
the 2 communities, more Cameron County women than Matamoros women reported a
previous pregnancy. Because of small numbers, we did not examine the outcomes of
previous pregnancies in these data. However, Cameron County
women may have had more pregnancies that did not result in a live birth.
Half of all abortions in the United States occur among women
younger than 25 years, and abortion rates among Hispanic women in the United States
are increasing (15). Women in Matamoros may have been less
likely than those in Cameron County to report a previous pregnancy that did not
result in a live birth, since most abortions are illegal in Mexico (16-18).
The large proportion of unintended and repeat pregnancies are cause for
concern. The situation appears to be somewhat worse in Cameron County, where
more of the women were single and lacked health insurance at the time of
conception. Possible contributors to the problem in Cameron County include
higher rates of alcohol consumption (19), lower crude rates of postpartum
contraception counseling during prenatal care, and lower rates of breastfeeding, which reduces fertility temporarily.
Additional analysis of survey data revealed that multigravida women in Cameron County reported a median interval of 24 months between the current live birth and the birth of the previous child, whereas the median interval for Matamoros women was 36 months.
The overall high proportion of unintended pregnancies is related to the low rates of contraception use both at first sexual intercourse (34.0%) and at conception (40.7%). Unintended pregnancy in this population may also be related to ineffective use of contraception, given that so many women reported use of contraception at conception. By comparison, US Hispanic females aged 15
to 19 years are nearly twice as likely to have used contraception at first sexual intercourse (66%) (20), and
similarly large proportions of female US Hispanic (55.5%) and Tamaulipas (54.3%) adolescents report using a condom at first sexual intercourse (20,21).
Condoms were the most common first method of contraception among both Matamoros and Cameron County women. The higher prevalence of IUD use in Matamoros may be due to greater emphasis on IUDs in public family planning services throughout Mexico, including Tamaulipas (18). Use of a method such as an IUD that is provider-administered and requires planning may also be more common among women who are married or cohabiting with their partners and
among women with health insurance, who represented a
larger proportion of the Matamoros than the Cameron County sample. While the IUD and injectable hormones offer greater long-term protection against pregnancy, neither protects against STIs, and rates of STIs are thought to be high and increasing in the border region (22-24). Although almost all study women knew at least 1 way to prevent HIV infection, almost 40% used a nonbarrier method of contraception. This survey did not include questions about dual use of contraceptive methods.
The rates of smoking at the time of pregnancy among the women in this study, most of whom were born in Mexico,
were considerably lower than those reported by all US (25) and Texas (26) Hispanic childbearing women (10.5% and 8.4%, respectively) in the Pregnancy Risk Assessment Monitoring System (PRAMS). Similarly, in preliminary Texas PRAMS data from 2005, 8.5% of Hispanic women aged 14
to 24
years reported smoking 3 months before giving birth (Eric
Miller, PhD, MSPH, written communication, March 2008). These rates differ dramatically from current smoking rates reported by US Hispanic female high school students (19.2%) (19). In Tamaulipas, we
did not measure current smoking, but 8.6% of all adolescent women reported having
ever smoked (21). The higher rates of smoking among Hispanic women in Texas and the United States
were lower than rates for US women overall (19,25-26) and may have resulted from increased levels of acculturation and years of residence in the United States (27).
The prevalence of alcohol use in Cameron County (38.4%) was comparable to that of young Hispanic women in Texas PRAMS data (35.8%) (26) and Hispanic female high school students
in the United States (44.8%) (19). Current alcohol use among Matamoros women in this survey (15.3%) was lower than lifetime prevalence of alcohol use among females aged 10
to 19 years in Tamaulipas (27.3%) (21). Cameron County women were more likely to
have used alcohol than were Matamoros women
despite the fact that the legal drinking age in
Mexico is 18, compared with 21 in the United States. This difference could also be due to acculturation of young Cameron County women,
or greater reluctance to admit drinking by women in Mexican society. Drinking was more common among Cameron County women who spoke English (46%) than
those who spoke Spanish (29%) (data not shown).
Cultural factors, such as a less favorable attitude toward breastfeeding in the United States, may contribute to the lower prevalence of breastfeeding in Cameron County than in Matamoros (28). This difference may also result from the lack of any national policy on breastfeeding in the United States, in contrast to very strong policies supporting breastfeeding in Mexico (29), and the provision of discounted infant formula to women in Cameron County hospitals (28). The breastfeeding prevalence in Matamoros was comparable to the prevalence reported by Tamaulipas adolescents in the mid-1990s (78.1%) (18). The 62.6% weighted prevalence of hospital breastfeeding among Cameron County women aged 14
to 24
years is consistent with findings from another study conducted in Texas in 2007 that showed a prevalence of 61.2% in this age group
(30). Increased and improved educational interventions to promote breastfeeding are needed in
the United States.
Most young women on both sides of the border had health care coverage during
pregnancy and received prenatal care. Rates of early prenatal care in Cameron
County were lower than those for all US women and nearly identical to rates
among US Hispanic women (25). The 57.9% prevalence of first trimester prenatal
care in Matamoros was lower than the 73.0% prevalence reported for all
Tamaulipas adolescents in an earlier survey (18). The low prevalence of cervical
cancer screening in Matamoros may be because such screening is not a routine
part of prenatal care for young women in Mexico (31). The most remarkable
feature of the clinical care received by these women is the high prevalence of
cesarean births in both communities. These levels are higher than overall US and
Tamaulipas rates (18,32) and much higher than what is considered optimal (15%) (33).
Despite the high rates of cesarean births, the gaps in prenatal care in both communities, and the low educational attainment, there is little indication in these data that the prevalence of low birth weight or preterm birth in these communities is
substantially different from that of the Mexican or US population as a whole (34,35). This phenomenon has been termed the “Hispanic paradox” (36) and has been noted among US Hispanics even after adjustment for the lower prevalence of
smoking among Hispanic women.
The overall strengths and limitations of the BMSCP that are discussed elsewhere (10) apply to this analysis. A contribution of this particular analysis is the way it helps isolate the effects of the social and health care environment on the pregnancies of groups of adolescents and other young women who have common genetic and cultural
traits. The study’s major weakness is the small number of adolescents,
which limited the possibilities for special analysis of
this age group. A second weakness is potential response bias from social pressure to avoid revealing undesirable behavior, especially with the stigma already associated with pregnancy among adolescents and single women.
Renewed efforts are needed to reduce the rates of unplanned pregnancies among adolescents
living in the US-Mexico border region, perhaps through
the creation of programs to increase the use
of contraception. Both communities need to provide low-cost health care coverage both before and during pregnancy. Increasing the percentage of women enrolled in prenatal care early should remain a priority. Preconception and postconception
reproductive health care should incorporate information about high-risk
behaviors such as smoking and alcohol consumption and increase rates of cervical
cancer screening. Hospitals should encourage breastfeeding and reduce the rates of cesarean
births. Several concerns identified in this analysis are evident on both sides of the border, and many of the young mothers and fathers involved have occupational, social, and familial ties in both countries; a joint effort of sister cities
to address these concerns, employing a
consistent binational and bilingual approach, would have many advantages.
Back to top
Acknowledgments
The BMSCP was funded through CDC’s Division of Reproductive Health and the Office of Global Health Promotion at the National Center for Chronic Disease Prevention and Health Promotion, under a
cooperative agreement with the United States-Mexico Border Health Association, No. U65 CCU 623699-01-2, and through interagency personnel agreements with the University of Texas at Brownsville and Texas Southmost College and the
University of Texas-Houston School of Public Health, Brownsville Regional Campus. In-kind project support was provided by CDC’s Division of Health Examination Statistics at the National Center for Health Statistics; the Texas Department of State Health Services, Region 11; the Secretariat of Health, Tamaulipas; and the Mexican Institute of Social Security, Tamaulipas.
Support from the following local, regional, and national institutions was
critical to the project: the National Center for Gender Equity and Reproductive Health, Mexican Health Secretariat; National Center for Epidemiologic Surveillance and Disease Control, Mexican Health Secretariat; National Center for Health Promotion, Mexican Health Secretariat; National Institute of Statistics, Geography and Informatics, Tamaulipas; Civil Registry, Tamaulipas;
Institute for Social Security and Services for State Workers, Tamaulipas; Secretariat of Health, Jurisdiction III, Tamaulipas;
Texas Department of State Health Services, Region 11 and Office of Border Health; City of Brownsville Department of Public Health; Cameron County Health Department; Valley Baptist Medical Center in Harlingen; Valley Baptist Medical Center in Brownsville; Valley Regional Medical Center; Harlingen Medical Center; Cameron Park Cultural Center; Brownsville Community Health Center; Dr. Alfredo Pumarejo Lafaurie, General Hospital of Matamoros; Mexican Institute of Social Security General Hospital,
Zone #13, Matamoros; Dr Manuel F. Rodríguez Brayda Clinical Hospital,
Matamoros; Hospital Guadalupe; Matamoros Center of Family Orientation; Medical Center of Surgical Specialties of Matamoros, and the United States-Mexico Border Health Commission.
We thank Dr Ruben Smith of the Division of Reproductive Health, CDC, for statistical assistance with birth rate calculations; Dr
Eric Miller, PRAMS Coordinator at the Texas Department of State Health Services,
for providing PRAMS data and comments on the manuscript; and Dr Ushma Upadhyay for her review of the manuscript. Special thanks to the National Center for Gender Equity and Reproductive Health, Secretariat of Health, Mexico, for coordinating review of this
manuscript in Mexico and to the United States-Mexico Border Health Commission for providing the English-Spanish translation.
Back to top
Author Information
Corresponding Author: Jill A. McDonald, PhD, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division of Reproductive Health, 4770 Buford Hwy NE, MS K-22, Atlanta, GA 30341-3724. Telephone: 770-488-6373. E-mail: Ezm5@cdc.gov.
Author Affiliations: Francisco Gerardo Galván González, Instituto Mexicano del Seguro Social, Coordinación Delegacional de Salud Reproductiva,
Ciudad Victoria, Tamaulipas, Mexico; Gita G. Mirchandani, Brian C. Castrucci, Ginger L. Gossman, Kayan L. Lewis, Texas Department of State Health Services, Division of Family and Community Health Services, Office of Title V, Austin, Texas; Mauro Ruiz, Texas Department of State Health Services, Region 11, Harlingen, Texas; Alonso Echegollen Guzmán, Instituto Mexicano del Seguro Social, Coordinación Delegacional de Investigación en Salud, Ciudad Victoria, Tamaulipas, Mexico.
Back to top
References
-
Shah IH, Leal OF, Bronfman M.
Sexual and reproductive health of young people. Salud Pública Méx 2008;50(1):8-9.
-
Jejeebhoy SJ. Sexual and reproductive health of young people: expanding the research and program agenda.
Los Altos (CA): David and Lucile Packard
Foundation; 2006. http://www.packard.org/assets/files/population/program%20review/pop_rev_jejeebhoy.pdf.
Accessed February 19, 2008.
-
Hamilton BE, Martin JA, Ventura SJ. Births: preliminary data for 2006. Natl Vital Stat Rep
2007;56(7).
-
National Center for Health Statistics. VitalStats (Custom data request). Atlanta
(GA): Centers for Disease Control and Prevention. http://www.cdc.gov/nchs/vitalstats.htm.
-
Interactive atlas of reproductive health. Atlanta (GA):
Centers for Disease Control and Prevention. http://www.cdc.gov/reproductivehealth/gisatlas/.
Accessed November 27, 2006.
-
Mexico National Institute of Statistics, Geography and Informatics (Instituto
Nacional de Estadística, Geografía e Informática) 2006. http://www.inegi.gob.mx/inegi/default.aspx.
Accessed February 8, 2008.
-
México Sistema Nacional de Informacion en Salud.
Juárez, Cuauhtémoc (MX): Dirección General de Información en Salud. http://sinais.salud.gob.mx.
Accessed February 23, 2008.
-
Healthy Border 2010: an agenda for improving health on the United States-Mexico
Border. El Paso (TX): United States-Mexico Border Health Commission; 2003.
http://www.borderhealth.org/files/res_63.pdf.
Accessed March 22, 2008.
-
UNICEF. El registro de nacimiento: el derecho a tener derechos. Florence (IT): Innocenti Digest; 2002. No. 9. http://unicef-irc.org/publications/pdf/digest9s.pdf.
Accessed March 25, 2008.
-
McDonald JA, Johnson CH, Smith R, Folger SG, Chavez AL, Mishra N, et al.
Reproductive health surveillance in the US-Mexico border region, 2003-2006: the
Brownsville-Matamoros Sister City Project for Women’s Health. Prev
Chronic Dis 2008;5(4).
http://www.cdc.gov/pcd/issues/2008/oct/08_0055.htm
- Conteo de población y vivienda 2005: principales resultados por localidad. Aguascalientes (MX): Instituto Nacional de Estadística
Geografía e Informática; 2005. http://www.inegi.gob.mx/est/contenidos/espanol/sistemas/ conteo2005/localidad/iter/default.asp?s=est&c=10395,
Spanish. Accessed February 4, 2008.
- County population datasets 2005. Washington (DC): U.S. Census Bureau. http://www.census.gov/popest/counties/asrh/CC-EST2006-alldata.html.
Accessed February 4, 2008.
-
Hosmer DW, Lemeshow S. Applied logistic regression. New York (NY): John Wiley and Sons; 2002.
-
Boorah VK. Logit and probit: ordered and multinomial models. Thousand Oaks (CA):
SAGE Publications; 2001.
- Strauss LT, Gamble SB, Parker WY, Cook
DA, Zane SB, Hamdan S.
Abortion
surveillance, United States--2004. MMWR Surveill Summ 2007;56(9):1-33.
-
Pregnant Pause. Summary of abortion laws around the world.
http://www.pregnantpause.org/lex/world02.htm. Accessed March 24, 2008.
-
Santos-Preciado JI, Villa-Barragán JP, García-Avilés MA, León-Alvarez G,
Quezada-Bolaños S, Tapia-Conyer R.
[The epidemiologic transition of the adolescents in Mexico]. Salud Publica
Mex 2003;45 Suppl 1:S140-52.
-
Zuñiga E, Zubieta B, Araya C, Delgado D. Cuadernos de salud reproductiva:
Tamaulipas. Primera edición. México D.F. (MX): Consejo Nacional de Población (CONAPO);
2000.
-
Eaton DK, Kann L, Kinchen S, Ross J, Hawkins J, Harris WA, et al.
Youth risk behavior surveillance, United States — 2005.
MMWR Surveill Summ 2006;55(5):1-108.
-
Abma JC, Martinez GM, Mosher WD, Dawson BS.
Teenagers in the United States:
sexual activity, contraceptive use, and childbearing, 2002. Vital Health
Stat 2004;23(24):1-48.
-
Encuesta Nacional de Salud y Nutrición 2006. Resultados por entidad federativa, Tamaulipas. Cuernavaca
(MX): Instituto Nacional de Salud Pública, Secretaría de Salud;
2007. http://www.insp.mx/ensanut/.
Accessed June 1, 2008.
-
Sexually transmitted disease surveillance, 2006. Atlanta (GA): Centers for
Disease Control and Prevention; 2007.
http://www.cdc.gov/std/stats/toc2006.htm.
Accessed February 10, 2008.
-
Rangel MG, Martínez-Donate AP, Hovell MF, Santibáñez J, Sipan CL, Izazola-Licea
JA.
Prevalence of risk factors for HIV infection among Mexican migrants and
immigrants: probability survey in the North border of Mexico. Salud Publica Mex 2006:48(1):3-12.
- Strathdee SA, Lozada R, Semple SJ, Orozovich P, Pu M, Staines-Orozco H, et al.
Characteristics of female sex workers with US clients in two Mexico-US border cities.
Sex Transm Dis 2008;35(3):263-8.
- McDonald JA, Suellentrop K, Paulozzi LJ, Morrow B.
Reproductive health of the rapidly growing Hispanic population: data from the Pregnancy Risk Assessment Monitoring System, 2002. Matern
Child Health J 2008;12(3):342-56.
-
PRAMS: Texas Pregnancy Risk Assessment Monitoring System. Annual report 2004.
Austin (TX): Texas Department of State Health Services.
http://www.dshs.state.tx.us/mch/pdf/PRAMS%20annual%2004%20FINAL.pdf.
Accessed January 8, 2008.
-
Bethel JW, Schenker MB.
Acculturation and smoking patterns among Hispanics: a review. Am J Prev Med 2005;29(2):143-8.
-
Gibson MV, Diaz VA, Mainous AG 3rd, Geesey ME.
Prevalence of breastfeeding and acculturation in Hispanics: results from NHANES 1999-2000 study. Birth 2005;32(2):93-8.
-
Atención de la mujer durante el embarazo, parto y puerperio y del recién nacido. Criterios y procedimientos para la prestación del servicio. Norma Oficial
Mexicana. NOM-007-SSA2-1993. Secciones 5.5.1.3, 5.7.1, 5.7.2, y 5.7.5-5.7.9.
-
Texas Department of State Health Services.
Breastfeeding beliefs, attitudes, and practices in the Texas WIC population.
Findings from the 2007 WIC Infant Feeding Practices Survey.
http://www.dshs.state.tx.us/wichd/nut/pdf/InfantFeedingPracticesSurvey.pdf.
- Castrucci BC,
Echegollen Guzmán A, Saraiya M, Smith BR, Lewis KL, Coughlin SS, et al. Cervical cancer screening among women residing near the US-Mexico border,
2005: the Brownsville-Matamoros Sister City Project for Women’s Health. Prev Chronic Dis 2008;5(4).
http://www.cdc.gov/pcd/issues/2008/oct/08_0063.htm.
-
Centers for Disease Control and Prevention. QuickStats: percentage of all live births by
cesarean delivery — National Vital Statistics System, United States, 2005. MMWR 2007;56(15):373. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5615a8.htm.
-
Althabe F, Belizán JM.
Caesarian section: the paradox. Lancet 2006;368(9546):1472-3.
-
Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Menacker F, Kirmeyer S, et al.
Births: final data for 2005. Natl Vital Stat Rep 2007;56(6):1-103.
- Torres-Arreola
LP, Constantino-Casas P, Flores-Hernández S, Villa-Barragán JP, Rendón-Macías E.
Socioeconomic factors and low birth weight in Mexico.
BMC Public Health 2005;5(1):20.
-
Franzini L, Ribble JC, Keddie AM.
Understanding the Hispanic paradox. Ethn Dis 2001;11(3):496-518.
Back to top
|
|
