 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Surveillance for Disparities in Maternal Health-Related Behaviors --- Selected States, Pregnancy Risk Assessment Monitoring System (PRAMS), 2000--2001Tanya M. Phares, M.P.H.1 Abstract Problem/Condition: Disparities in maternal and infant health have been observed among members of different racial and ethnic populations and persons of differing socioeconomic status. For the Healthy People 2010 objectives for maternal and child health to be achieved (US Department of Health and Human Services. Healthy People 2010. 2nd ed. With understanding and improving health and objectives for improving health [2 vols.]. Washington DC: US Department of Health and Human Services, 2000), the nature and extent of disparities in maternal behaviors that affect maternal or infant health should be understood. Identifying these disparities can assist public health authorities in developing policies and programs targeting persons at greatest risk for adverse health outcomes. Reporting Period Covered: 2000--2001. Description of System: The Pregnancy Risk Assessment Monitoring System (PRAMS) is an ongoing state- and population-based surveillance system designed to monitor selected maternal behaviors and experiences that occur before, during, and after pregnancy among women who deliver live-born infants. PRAMS employs a mixed mode data-collection methodology; up to three self-administered surveys are mailed to a sample of mothers, and nonresponders are followed up with telephone interviews. Self-reported survey data are linked to selected birth certificate data and weighted for sample design, nonresponse, and noncoverage to create annual PRAMS analysis data sets that can be used to produce statewide estimates of different perinatal health behaviors and experiences among women delivering live infants in 31 states and New York City. This report summarizes data for 2000--2001 from eight states (Alabama, Colorado, Florida, Hawaii, Illinois, Maine, Nebraska, and North Carolina) on four behaviors (smoking during pregnancy, alcohol use during pregnancy, breastfeeding initiation, and use of the infant back sleep position) for which substantial health disparities have been identified previously. Results: Although the prevalence of each behavior varied by state, consistent patterns were observed among the eight states by age, race, ethnicity, education, and income level. Overall, the prevalence of smoking during pregnancy ranged from 9.0% to 17.4%. Younger (aged <25 years) women, white women, American Indian women, non-Hispanic women (except in Hawaii), women with a high school education or less, and women with low incomes consistently reported the highest rates of smoking. Overall, the prevalence of alcohol use during pregnancy ranged from 3.4% to 9.9%. In seven states, women aged >35 years, non-Hispanic women, women with more than a high school education, and women with higher incomes reported the highest prevalence of alcohol use during pregnancy. Overall, the prevalence of breastfeeding initiation ranged from 54.8% to 89.6%. Younger women, black women, women with a high school education or less, and women with low incomes reported the lowest rates of breastfeeding initiation. The size of the black-white disparity in breastfeeding varied among states. Overall, use of the back sleep position for infants ranged from 49.7% to 74.8%. Use of the back sleep position was lowest among younger women, black women, women with lower levels of education, and women with low incomes. Ethnic differences in sleep position varied substantially by state. Interpretation: PRAMS data can be used to identify racial, ethnic, and socioeconomic disparities in critical maternal health-related behaviors. Although similar general patterns by age, education, and income were observed in at least seven states, certain racial and ethnic disparities varied by state. Prevalence of the four behaviors among each population often varied by state, indicating the potential impact of state-specific policies and programs. Public Health Action: States can use PRAMS data to identify populations at greatest risk for maternal behaviors that have negative consequences for maternal and infant health and to develop policies and plan programs that target populations at high risk. Although prevalence data cannot be used to identify causes or interventions to improve health outcomes, they do indicate the magnitude of disparities and identify populations that should be targeted for intervention. This report indicates a need for wider targeting than is often done. The results from this report can aid state and national agencies in creating more effective public health policies and programs. The data described in this report should serve as a baseline that states can use to measure the impact of policies and programs on eliminating these health disparities. IntroductionAdverse maternal and infant health outcomes (e.g., low birthweight, preterm delivery, cognitive impairment, and sudden infant death syndrome [SIDS]) often can be prevented by modifying maternal behaviors. Maternal tobacco use during pregnancy is the strongest known risk factor for low birthweight and is associated with spontaneous abortion and preterm delivery (1--4). Alcohol use during early pregnancy can result in spontaneous abortion, behavior and learning problems in children, fetal alcohol syndrome, or low birthweight; continued alcohol use throughout pregnancy can worsen these effects and cause preterm delivery (5--10). Because no safe level of alcohol use during pregnancy has been identified (8), women are encouraged to abstain from alcohol throughout pregnancy (4). Breastfeeding provides the best form of infant nutrition and immunity during the first 6 months of life and is beneficial to infant growth and development (11). The American Academy of Pediatrics recommends that infants be put to sleep on their backs because the supine (back) position is associated with a decreased risk of SIDS (12--14). The goal of Healthy People 2010 is to improve the health and well-being of women, infants, children, and families (4). For this goal to be achieved, objectives have been established along with specific targets. With respect to the four behaviors discussed in this report, Healthy People 2010 targets are that >99% of women abstain from smoking during pregnancy to reduce low birthweight, that <6% of women drink alcohol during pregnancy, that >75% of mothers initiate breastfeeding, and that >70% of mothers place their infants to sleep on their backs. Healthy People 2010 identified critical maternal and infant health disparities by using baseline data from 1998 (4). For the Healthy People 2010 objectives to be achieved, these disparities should be eliminated (4,15). This report uses recent data from eight states to monitor progress toward eliminating certain disparities. The burden of poor health among women and infants in the United States is experienced disproportionately by persons in certain age groups and members of certain racial, ethnic, and socioeconomic populations. For example, research published previously indicates that being white, having less than a high school education, and having a low income are risk factors for, or are associated with, smoking during pregnancy (16,17). The prevalence of smoking is reportedly higher among non-Hispanic women than among Hispanic women (18). Findings from the Behavioral Risk Factor Surveillance System indicate that age is a strong predictor of alcohol use; pregnant women who reported alcohol use tended to be aged >30 years, and older women were less likely than younger women to reduce alcohol consumption during pregnancy (10). Breastfeeding initiation has been associated with older maternal age, Hispanic ethnicity, higher socioeconomic status, previous breastfeeding experience, and having positive social support for breastfeeding (19--22). Use of the back sleep position is less common among non-Hispanic black, Hispanic, and Asian mothers than among other racial and ethnic populations and correlates positively with increased maternal age, education, and income (23,24). However, use of the back sleep position is also reported to be higher among Hispanic and Asian mothers than among other ethnic or racial populations (13). This report analyzes data concerning four maternal behaviors for which Healthy People 2010 objectives exist: smoking use during pregnancy, alcohol use during pregnancy, breastfeeding initiation, and placing infants in the back sleep position. These behaviors were chosen because substantial disparities in these behaviors were identified by Healthy People 2010. The results will be discussed in the context of sociodemographic disparities and Healthy People 2010 targets. The goal of this report is to provide information that states can use to target health services and to design and evaluate health promotion programs working to achieve Healthy People 2010 goals. The data provided in this report can serve as a baseline for monitoring progress toward eliminating these health disparities. MethodsProject DescriptionThe Pregnancy Risk Assessment Monitoring System (PRAMS) is an ongoing state- and population-based surveillance system designed to monitor selected self-reported maternal behaviors and experiences that occur before, during, and after pregnancy among women who deliver live-born infants. Initiated in 1987 and administered in collaboration with state health departments by CDC's National Center for Chronic Disease Prevention and Health Promotion, Division of Reproductive Health, PRAMS was established to help state health departments maintain an epidemiologic surveillance system of selected maternal behaviors and experiences, supplementing data from vital records. The program has expanded from the original six states in 1987 to 32 project areas in 31 states in 2003, including 28 states and one city that conduct traditional PRAMS surveillance, two states that completed a point-in-time survey in 2002, and one state that conducts traditional PRAMS surveillance as well as additional PRAMS activities. Live births in these project areas represent approximately 62% of all live births in the United States. Data CollectionReporting areas use a standardized data collection methodology developed by CDC. For traditional PRAMS surveillance, a monthly stratified sample of 100--300 new mothers is selected from eligible birth certificates in each project area. PRAMS uses a mixed mode data-collection methodology; up to three self-administered surveys are mailed to mothers in the sample, and nonresponders are followed up with a telephone interview. Typically, the first survey is mailed 2--3 months after delivery to permit collection of information about postpartum maternal and infant experiences. Self-reported survey data are linked to selected birth certificate data and weighted for sample design, nonresponse, and noncoverage to create the PRAMS analysis data sets. The PRAMS questionnaire is revised periodically to reflect changing priorities and emerging concerns. Each revision is referred to as a phase. The data highlighted in this report were collected with the Phase Four version of the questionnaire, which was implemented with the 2000 birth cohort. Additional details about the PRAMS methodology have been described elsewhere (25). Data AnalysisDuring 2000--2001, a total of 32 reporting areas participated in PRAMS (Figure 1). This report covers eight selected states that collected data during 2000--2001: Alabama, Colorado, Florida, Hawaii, Illinois, Maine, Nebraska, and North Carolina. These states had fully implemented PRAMS data collection procedures during 2000--2001 and achieved weighted response rates of >70% for each year. The weighted response rate indicates the proportion of women sampled who completed a survey, adjusted for sample design. These eight states were included in the analyses because their 2001 weighted data were available as of October 1, 2003. Data for the four maternal behaviors studied were self-reported on the survey. Because women often fail to report alcohol use during their first trimester before learning they are pregnant, PRAMS collects data on alcohol and smoking only during the 3 months before pregnancy and the last 3 months of pregnancy. Because women commonly cease smoking and drinking after they learn they are pregnant (26), smoking and alcohol use during the last 3 months of pregnancy were chosen as measures of maternal behavior for this analysis. Smoking during pregnancy was defined as smoking at any time during the last 3 months of pregnancy, and alcohol use during pregnancy was defined as drinking any alcohol during the last 3 months of pregnancy. Women who continue to smoke or use alcohol might be most in need of intervention. Using the last 3 months also permits comparison with Healthy People 2010 targets for smoking and alcohol use throughout pregnancy. Breastfeeding initiation was defined as breastfeeding or pumping breast milk to feed a baby after delivery. Infant sleep position was defined as whether an infant was usually put down to sleep in the supine (back) position. Prevalence estimates and confidence intervals for combined data for 2000--2001 are presented by state and by five maternal sociodemographic characteristics: age group, race, ethnicity, education, and income level. All characteristics except for income level were taken from birth certificates. Age was grouped into four categories: <20 years, 20--24 years, 25--34 years, and >35 years. Maternal race categories included white, black, American Indian, and Asian/Pacific Islander. In Hawaii, the Asian/Pacific Islander category was subdivided further into Filipino, Hawaiian, and other Asian; data for these subcategories are noted in this report but not presented in the tables. Ethnicity was reported as either Hispanic or non-Hispanic. Maternal education was categorized as less than high school (<12 years), high school (12 years), or more than high school (>12 years). Income level was self-reported on the PRAMS questionnaire and converted into a percentage of the federal poverty level (FPL) in multiple ways, varying by state. Because surveys asked about the period before the baby's birth, the 1999 FPL was used in each case. In Nebraska, respondents were asked an open-ended question about family income; the answer was converted to a percentage of FPL according to published charts of the federal poverty cut-offs by family size. For the remaining six states in which the question had closed-ended response categories, income was recalculated as a percentage of FPL by using the following methodology. First, a midpoint was calculated for each category. Because the highest categories were open-ended (e.g., >$40,000), the midpoints for these upper-income categories were determined by using Census 2000 income estimates for each state. Second, after adjustment for family size, incomes were categorized into three levels: <100% FPL, 101%--200% FPL, and >201% FPL. Because the Alabama PRAMS survey did not include questions on income level, income data are not available for that state. All tables in the report were produced by using weighted PRAMS data. Percentages and standard errors were calculated by using PROC CROSSTAB in SUDAAN, and 95% confidence intervals (CIs) were computed by using the formula CI = percentage ± (1.96 x standard error). The number of respondents is listed for each state. An estimate is noted in the tables when the percentage of missing values is >10%. In all states, a substantial percentage of respondents declined to report income. Because states and women not reporting income might differ from those that do, a "missing" category was included for income. For sleep position, >10% of data are missing for seven states. Data from women who reported using multiple positions (e.g., back and side or back and stomach) for putting their babies down to sleep were not used in the analysis. Because estimates based on limited samples are imprecise and might be biased, when the number of respondents was <30, estimates are not reported in the tables that present data by sociodemographic categories (27). Estimates based on <60 respondents are reported but might be unreliable as a result of the limited sample size (27). Chi-square testing was used to identify statistically significant disparities between sociodemographic categories. The chi-square test was considered significant if the p-value for the demographic characteristic was <0.05. Simple logistic regression was used to test for trend in ordered variables (age, education, and income level). The magnitude of the disparities among sociodemographic variables is best observed by examining the tables and figures. Calculating prevalence ratios to assess the magnitude of disparities was beyond the scope of this report. One figure for each behavior was chosen to depict the most substantial disparity observed within any state. ResultsCharacteristicsThe sociodemographic characteristics of women delivering live-born infants during 2000--2001 varied among states (Table 1). Among the eight states, the proportion of adolescents (persons aged <20 years) ranged from 8.9% to 15.9%. Although the majority of women in seven states were white, in four states (Alabama, Florida, Illinois, and North Carolina), the proportion of black women was approximately 20%. In Hawaii, the majority of women were Asian/Pacific Islanders. The proportion of Hispanic women varied among states, ranging from 1.0% in Maine to 28.3% in Colorado. Approximately half of all women had completed >12 years of education. Income distribution varied by state; the proportion of women with very low income (<100% FPL) ranged from 21.1% in Nebraska to 33.5% in Florida. Smoking During PregnancyNo states achieved the Healthy People 2010 target that <1% of women smoke during pregnancy. The overall prevalence of smoking during the last 3 months of pregnancy ranged from 9.0% in Hawaii to 17.4% in Maine (Table 1). Among the eight states, younger women, white or American Indian women, non-Hispanic women (except in Hawaii), women with <12 years of education, and women with low incomes consistently reported the highest rates of smoking during pregnancy (Table 2). In no state did women of any age group achieve the Healthy People 2010 target for abstinence from smoking during pregnancy. However, in all eight states, smoking decreased substantially with maternal age. No racial population achieved the Healthy People 2010 target for smoking prevalence. Overall, smoking prevalence was highest among American Indians in three states (Colorado, Nebraska, and North Carolina). However, estimated prevalence for American Indian women might be unreliable in two states (Colorado and North Carolina) as a result of limited sample sizes. Among white women, smoking prevalence was highest in Alabama; among black women, prevalence was highest in Colorado; and among Asian/Pacific Islanders, prevalence was highest among Native Hawaiian women (15.2%; data not shown). Only Hispanic women in Alabama achieved the Healthy People 2010 target for smoking abstinence. In six states (Alabama, Colorado, Florida, Illinois, Nebraska, and North Carolina), non-Hispanic women were more likely than Hispanic women to report smoking during pregnancy (Table 2). The Healthy People 2010 target for smoking abstinence was not achieved by women of any education level. In four states (Alabama, Florida, Hawaii, and Maine), smoking prevalence decreased as education increased. Among all states, women with >12 years of education had the lowest rates of smoking (Figure 2). No income level in any state achieved the Healthy People 2010 target for smoking abstinence during the last 3 months of pregnancy. In six states (Colorado, Hawaii, Illinois, Maine, Nebraska, and North Carolina), smoking prevalence decreased with increasing income level (Table 2). Among all states, women whose income levels were <100% FPL and 101%--200% FPL had higher rates of smoking than women with higher incomes. Alcohol Use During PregnancyThe overall prevalence of alcohol use during the last 3 months of pregnancy ranged from 3.4% in Nebraska to 9.9% in Colorado (Table 1). In six states (Alabama, Florida, Hawaii, Maine, Nebraska, and North Carolina), women achieved the Healthy People 2010 target of <6% alcohol use during pregnancy. In seven states, the highest prevalence of alcohol use during the last 3 months of pregnancy was reported by older women, non-Hispanic women, those with more than a high school education, and those with higher income (Table 3). In all states except Nebraska, the proportion of women aged >35 years reporting alcohol use during pregnancy exceeded the Healthy People 2010 target. However, the target was achieved among all women aged <25 years. Prevalence of alcohol use during pregnancy increased with age in all states; adolescents had the lowest rates of alcohol use, and women aged >35 years had the highest rates (Table 3, Figure 3). Asian/Pacific Islander women were the only racial population to achieve the Healthy People 2010 target for alcohol abstinence during pregnancy in multiple states. However, regional variation was noted in that both white and black women failed to achieve the Healthy People 2010 target in Colorado and Hawaii. The prevalence of alcohol use during pregnancy was greatest among white women in Colorado, among black and American Indian women in Hawaii, and among Asian/Pacific Islander women in Colorado. Hispanic women achieved the Healthy People 2010 target for alcohol abstinence in six states (Colorado, Florida, Hawaii, Illinois, Nebraska, and North Carolina). Non-Hispanic women also achieved this target in six states (Alabama, Florida, Hawaii, Maine, Nebraska, and North Carolina). In three states (Colorado, Illinois, and North Carolina), the prevalence of alcohol use during pregnancy was lower among Hispanic women than among non-Hispanic women (Table 3). In five states (Colorado, Florida, Illinois, Maine, and North Carolina), the Healthy People 2010 target for alcohol abstinence was not achieved by women with >12 years education. In six states (Colorado, Florida, Illinois, Maine, Nebraska, and North Carolina), alcohol use increased with education (Table 3). In six (Colorado, Florida, Hawaii, Illinois, Maine, and North Carolina) of seven states with income measures, alcohol use during pregnancy increased with income (Table 3). In six states (Florida, Hawaii, Illinois, Maine, Nebraska and North Carolina), women with income levels of <200% FPL achieved the Healthy People 2010 target for alcohol abstinence during pregnancy, but women with higher income levels did not. In Nebraska, the prevalence of alcohol use during pregnancy did not differ substantially by income level. Breastfeeding InitiationThe prevalence of breastfeeding initiation ranged from 54.8% in Alabama to 89.6% in Hawaii (Table 1). Four states (Colorado, Florida, Hawaii, and Maine) surpassed the Healthy People 2010 target of >75% of women initiating breastfeeding. In all eight states, younger women, black women, those with <12 years of education, and those with low incomes reported the lowest rates of breastfeeding initiation (Table 4). The size of the black-white disparity in breastfeeding varied by state (Figure 4). Although women aged >35 years achieved the Healthy People 2010 target of 75% in all but two states (Alabama and North Carolina), adolescents achieved the target in only two states (Colorado and Hawaii). In Colorado and Hawaii, women of all age groups achieved the Healthy People 2010 target for breastfeeding. In all states, the prevalence of breastfeeding initiation increased with age; the greatest differences were observed between women aged <25 years and those aged >25 years. Hawaii was the only state in which women of all racial populations achieved the Healthy People 2010 target for breastfeeding initiation. In five states (Alabama, Florida, Illinois, Nebraska, and North Carolina), the prevalence of breastfeeding initiation was higher among white women than among black women (Table 4). Black women did not achieve the Healthy People 2010 target in any state except Hawaii. Among black women, the rate of breastfeeding was lowest in Alabama and highest in Hawaii (Table 4). In Hawaii, the prevalence of breastfeeding initiation was highest among Filipino (91.8%; data not shown), other Asian (92.1%; data not shown), and white women (91.0%). In all states, breastfeeding among Hispanic women surpassed the Healthy People 2010 objective (Table 4). Among non-Hispanic women, only three states (Colorado, Hawaii, and Maine) reached the Healthy People 2010 target. In five states (Alabama, Florida, Illinois, Nebraska, and North Carolina), the prevalence of breastfeeding initiation was higher among Hispanic women than among non-Hispanic women (Table 4). In two states (Colorado and Hawaii), women of all education levels achieved the Healthy People 2010 target for breastfeeding initiation. In all states, breastfeeding prevalence increased substantially with higher education levels (Table 4). In all states with income measures, the prevalence of breastfeeding initiation increased with higher income level; women with incomes of <100% FPL and 101%--200% FPL reported lower rates of breastfeeding than women with higher incomes (Table 4). Breastfeeding initiation had the lowest disparity by income level in Hawaii and Colorado; women of all income levels achieved the Healthy People 2010 target for breastfeeding in these two states. In five states (Florida, Illinois, Maine, Nebraska, and North Carolina), women with incomes <100% FPL did not achieve the Healthy People 2010 target for breastfeeding initiation, and in three states (Illinois, Nebraska, and North Carolina), women with incomes <100% FPL and 101%--200% FPL did not achieve the target. Back Infant Sleep PositionThe overall prevalence of mothers using the recommended back sleep position for their infants ranged from 49.7% in Alabama to 74.8% in Maine (Table 1). Only two states (Colorado and Maine) achieved the Healthy People 2010 target of >70% of infants put to sleep in the back position. Among all eight states, use of the back sleep position was lowest among younger women, black women, women with lower levels of education, and women with low incomes; ethnic differences in sleep position varied by state (Table 5). Maine was the only state in which women of all age groups achieved the Healthy People 2010 target for sleep position. In three states (Alabama, Florida, and North Carolina), the sleep position target was not achieved by women of any age group. In all states except Maine, use of the back sleep position increased with maternal age (Table 5). In three states (Alabama, Florida, and North Carolina), women of all racial populations did not achieve the Healthy People 2010 target of >70% use of the back sleep position. In Nebraska, both Native American women and Asian/Pacific Islander women achieved the >70% target. However, black women did not achieve the target in any state. The prevalence of the back sleep position was lowest among black women in Alabama and Florida. In six states (Alabama, Florida, Hawaii, Illinois, Nebraska, and North Carolina), the prevalence of back sleep position was lower among black women than among white women (Table 5, Figure 5). Among all Hispanic women, the prevalence of putting infants to sleep on their backs was below the Healthy People 2010 target. Although Hispanic women were further from the target in several states, non-Hispanic women also did not achieve the Healthy People 2010 target for sleep position in six states (Alabama, Florida, Hawaii, Illinois, Nebraska, and North Carolina). In two states (Colorado and Florida), Hispanic women were less likely than non-Hispanic women to put their infants to sleep on their backs (Table 5). In three states (Alabama, Florida, and North Carolina), women of all education levels did not achieve the Healthy People 2010 target for the back sleep position. In all states, use of the back sleep position increased with higher education level. In no state did women whose income level was <100% FPL achieve the Healthy People 2010 target for infant sleep position. The prevalence of infants being put to sleep in the back position increased with higher income levels in the seven states that measured income (Table 5). The lowest reported prevalence of the back sleep position occurred in Florida, which had the highest percentage of women whose income level was <100% FPL (Table 1). Compared with infants from other states, infants were more often placed on their backs to sleep in Colorado and in Maine, which had the highest percentage of women with income levels of >200% FPL (Table 1). DiscussionAgeYounger women were less likely than older women to breastfeed their children and use the back sleep position, and they were more likely to report smoking during the last 3 months of pregnancy. However, for alcohol use, the pattern was reversed (i.e., prevalence of alcohol use increased with age). The association between older age and higher prevalence of alcohol use during pregnancy has been reported previously (28--30). Older age might reflect a longer duration of engaging in potentially addictive behaviors. The difference in the direction of association between age and smoking on the one hand, and age and alcohol use on the other, indicates that different factors might be involved. Adolescent pregnancy can have serious adverse long-term social and economic consequences for mothers and children (31,32). Preventing adolescent pregnancy, developing and applying effective methods for preventing adolescent smoking, and promoting other health-related behavior change among adolescents might reduce these disparities. RaceIn each state, the prevalence of each behavior varied widely within each racial population. This indicates that a state's social and policy environment might affect a woman's risk for certain behaviors during pregnancy (33). Because serious health consequences can result from smoking during pregnancy, greater efforts are needed to change behavior among all racial populations. Previous studies have demonstrated that pregnant women are motivated to stop smoking (30,34). The use of alcohol might be linked to social or cultural norms that can vary across racial or ethnic populations (35--37). However, women might be especially receptive to health promotion messages, education, and advice from medical professionals during pregnancy regardless of social norms. EthnicityHispanic women were more likely than non-Hispanic women to breastfeed their infants and abstain from smoking or alcohol use during the last 3 months of pregnancy. Breastfeeding rates for Hispanic women have been reported to be higher than rates for non-Hispanic women (38,39). Relatively favorable health-related behaviors and perinatal health outcomes have been reported among Hispanic women, despite relative socioeconomic disadvantage (39,40). After the national "Back to Sleep" campaign, adherence to recommendations on sleep position was most striking among Hispanics, with a sharp increase in the late 1990s (41). Although that increase over time indicates receptiveness of Hispanic families to such education efforts, the low prevalence of back sleep position reported in this study indicates that more needs to be done to reach these families with effective messages about infant sleep position. EducationWomen with >12 years of education were consistently more likely than women with less education to breastfeed their children, use the back sleep position for infants, and abstain from smoking. Women with less schooling might be less likely to receive or seek out information, or less likely to understand and use information they do receive, if that information requires literacy or comprehension skills that are too high. These findings indicate a need for prenatal health promotion materials that target women of lower literacy or education levels. IncomeThe prevalence of breastfeeding initiation and use of the back sleep position was lowest among women with the lowest incomes. Similarly, smoking was highest among women with the lowest incomes. For such disparities to be decreased, the specific needs of low-income women should be identified and addressed. LimitationsThe data presented in this report are subject to the following limitations:
ConclusionAchieving the Healthy People 2010 targets for maternal and infant health requires effectively reducing health disparities. Certain behaviors, including those examined in this report, are well established as proximate determinants of adverse maternal or infant health outcomes and therefore are a starting point for prevention efforts. Health behavior, in turn, is affected by various underlying conditions that might act as facilitating factors or barriers to optimal health behaviors; these more distal or underlying conditions also should be considered as potential starting points for prevention strategies. This report has described the prevalence of selected maternal behaviors among different populations of women categorized by their age, race, ethnicity, education, and income level. The goals of this report were to indicate the scope of the problem and to identify where efforts should be targeted but not to identify the factors that predict these behaviors. Continued research is needed to further examine factors experienced by these groups of women that prevent or enhance health-promoting behaviors, as well as factors at the state and regional levels that encourage and support healthy behaviors. These descriptive results reveal marked socioeconomic, racial, ethnic, and age disparities in four critical maternal health-related behaviors. Younger women, women with less education, and those with lower incomes were less likely to report breastfeeding and back sleep position and more likely to report smoking during pregnancy. The patterns were different, however, for alcohol use during pregnancy, which was more prevalent among older women, white women, those with more education, and those with higher incomes. Although interpreting this different pattern is difficult, similar findings have been reported previously (10,18). Further research should take cultural adaptation into consideration, because it might have a strong effect on maternal health behavior (39,42). Of importance to public health efforts is the finding that wider targeting might be needed to reach women at increased risk for negative health outcomes. Overall, women whose incomes were <100% FPL and 101%--200% FPL did not achieve Healthy People 2010 targets. Lower prevalence of healthy behaviors was observed among women without a high-school diploma and those who were high-school graduates than among those with more than a high-school education. PRAMS is an important source of data on maternal and infant health behaviors and outcomes along with socioeconomic and racial/ethnic information, permitting an examination of health disparities. The data provided in this report for 2000--2001 can be used as a baseline for subsequent monitoring of progress toward eliminating health disparities. Monitoring cannot determine causes but is crucial in assessing the impact of changes in policies and programs on health disparities. Acknowledgments The PRAMS Working Group: Alabama, Rhonda Stephens, M.P.H.; Colorado, Alyson Shupe, Ph.D.; Florida, Steven Wiersma, M.D.; Hawaii, Limin Song, M.P.H.; Illinois, Theresa Sandidge, M.A.; Maine, Martha Henson; Nebraska, Debbi Barnes-Josiah, Ph.D.; North Carolina, Paul Buescher, Ph.D.; CDC PRAMS Team, Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion. References
Table 1  Return to top. Figure 1 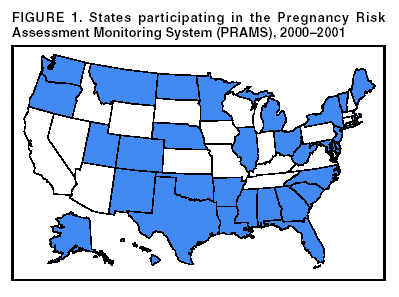 Return to top. Table 2 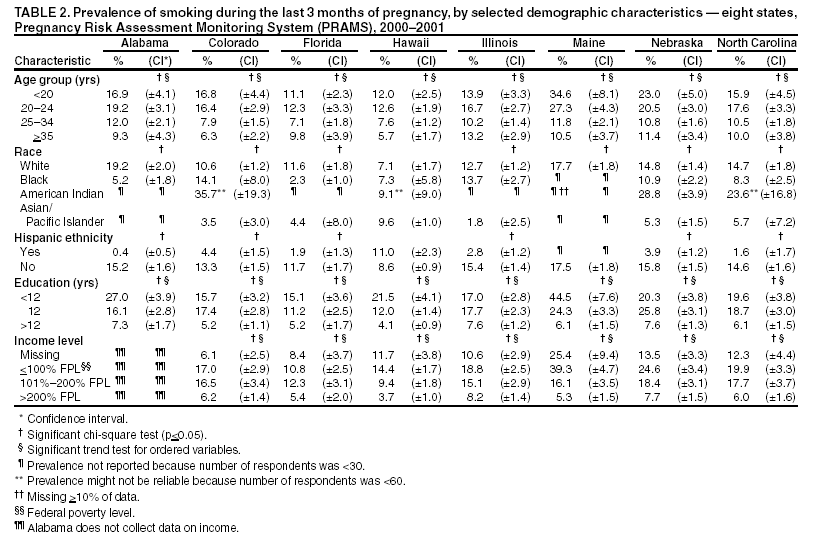 Return to top. Figure 2 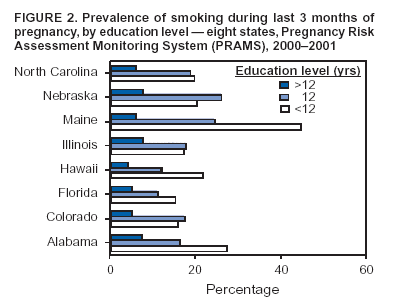 Return to top. Table 3 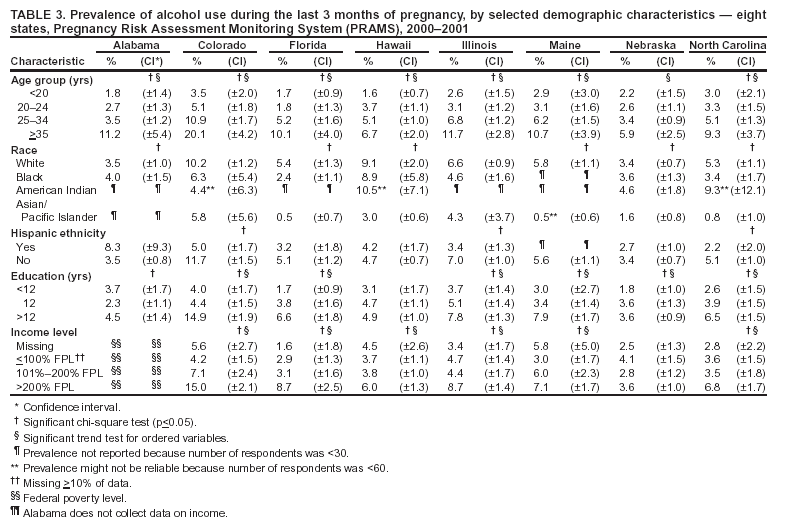 Return to top. Figure 3 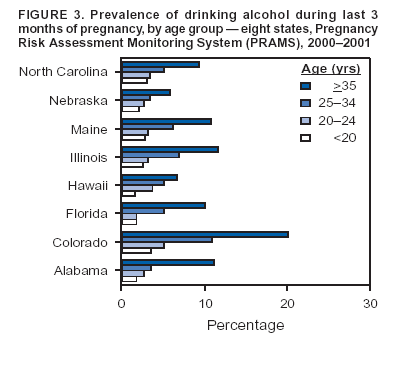 Return to top. Table 4 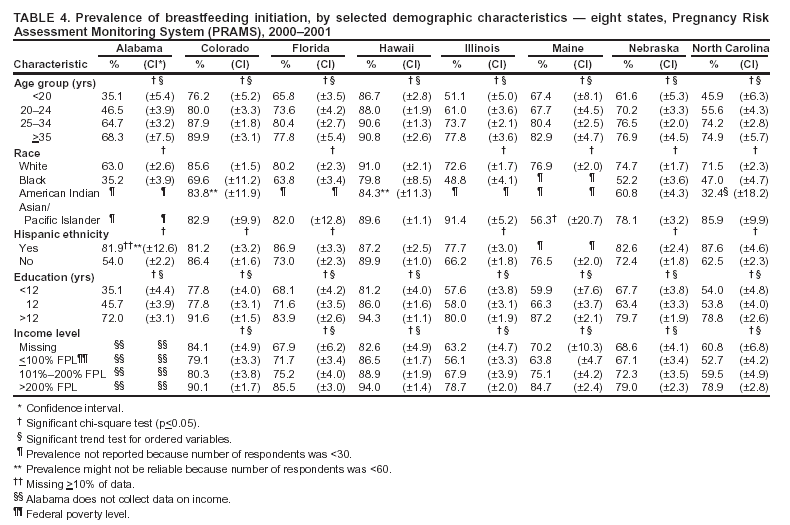 Return to top. Figure 4 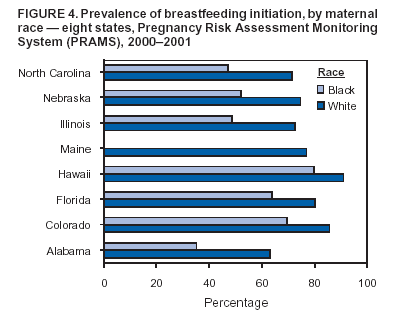 Return to top. Table 5 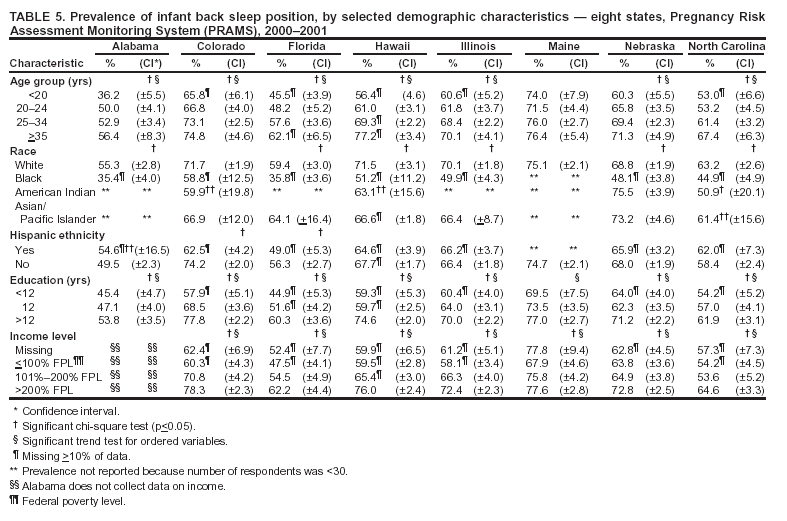 Return to top. Figure 5 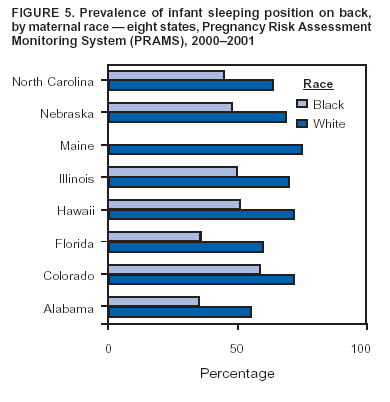 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 6/16/2004 |
|||||||||
This page last reviewed 6/16/2004
|