 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. School Health Guidelines to Prevent Unintentional Injuries and ViolenceTechnical Advisors for School Health Guidelines to Prevent Unintentional Injuries and Violence Olga Acosta, Ph.D. Kris Bosworth, Ph.D. Elaine Brainerd, M.A. Jack Campana, M.Ed. David Dilillo, Ph.D. Karen Dunne-Maxim, M.S. Doris Evans-Gates, M.S. Susan Scavo Gallagher, M.P.H. Andrea Carlson Gielen, Sc.D. Cynthia Hudley, Ph.D. Angela Mickalide, Ph.D. Kathleen Miner, Ph.D. Beatriz Perez, M.P.H. Lizette Peterson, Ph.D. Carol Runyan, Ph.D. Emilie Smith, Ph.D. Howard Spivak, M.D. Ronald Stephens Deborah Stone, M.S.W., M.P.H. Ann Thacher, M.S. Patrick Tolan, Ph.D. Douglas White, M.S. Participating Federal Agencies Consumer Product Safety Commission Federal Emergency Management Agency Office of National Drug Control Policy U.S. Department of Education U.S. Department of Justice U.S. Department of Transportation U.S. Department of Health and Human Services National Institute of Mental Health, National Institutes of Health Participating National Organizations American Academy of Pediatrics The following CDC staff members prepared this report: Lisa C. Barrios, Dr.P.H. Sujata Desai, Ph.D. David A. Sleet, Ph.D. Daniel M. Sosin, M.D., M.P.H. SummaryApproximately two thirds of all deaths among children and adolescents aged 5--19 years result from injury-related causes: motor-vehicle crashes, all other unintentional injuries, homicide, and suicide. Schools have a responsibility to prevent injuries from occurring on school property and at school-sponsored events. In addition, schools can teach students the skills needed to promote safety and prevent unintentional injuries, violence, and suicide while at home, at work, at play, in the community, and throughout their lives. This report summarizes school health recommendations for preventing unintentional injury, violence, and suicide among young persons. These guidelines were developed by CDC in collaboration with specialists from universities and from national, federal, state, local, and voluntary agencies and organizations. They are based on an in-depth review of research, theory, and current practice in unintentional injury, violence, and suicide prevention; health education; and public health. Every recommendation is not appropriate or feasible for every school to implement. Schools should determine which recommendations have the highest priority based on the needs of the school and available resources. The guidelines include recommendations related to the following eight aspects of school health efforts to prevent unintentional injury, violence, and suicide:
INTRODUCTIONInjuries are the leading cause of death and disability for persons aged 1--44 years in the United States (1). In 1998, a total of 14,616 U.S. children and adolescents aged 5--19 years died from injuries (2). Because injury takes such a toll on the health and well-being of young persons, the Healthy People 2010 objectives encourage schools to provide comprehensive health education to prevent unintentional injury, violence, and suicide (3). Coordinated school health programs, in conjunction with community efforts, can prevent injuries to students in school and help youth establish lifelong safety skills (4,5). This report is one in a series of CDC guidelines that provide guidance for school health efforts to promote healthy and safe behavior among children and adolescents (6--9). Risk factors and strategies for preventing and addressing unintentional injury, violence, and suicide are related. Therefore, the guidelines in this report address unintentional injury, violence, and suicide prevention for students in prekindergarten through 12th grade through school instructional programs, school psychosocial and physical environments, and various services schools provide. Because the health and safety of children and adolescents is affected by factors beyond the school setting, these guidelines also address family and community involvement. The primary audience for this report is state and local health and education agencies and nongovernmental organizations concerned with improving the health and safety of U.S. students. These agencies and organizations can translate the information in this report into materials and training programs for their constituents. In addition, CDC will develop and disseminate materials to help schools and school districts implement the guidelines. At the local level, teachers and other school personnel, community recreation program personnel, health service providers, emergency medical services providers, public safety personnel, community leaders, policymakers, and parents might use these guidelines and complementary materials to plan and implement unintentional injury, violence, and suicide-prevention policies and programs. Although these guidelines are designed primarily for traditional school settings, the broad recommendations would be applicable for alternative settings. In addition, faculty at institutions of higher education can use these guidelines to train professionals in education, public health, sports and recreation, school psychology, nursing, medicine, and other appropriate disciplines. CDC developed these guidelines by a) reviewing published research; b) considering the recommendations in national policy documents; c) convening specialists in unintentional injury, violence, and suicide prevention; and d) consulting with relevant federal, state, and local agencies and national nongovernmental organizations representing state and local policy makers, educators, parents, allied health personnel, and specialists in unintentional injury, violence, and suicide prevention. When possible, these guidelines are based on research evidence. They also are based on behavioral theory and evidence from exemplary practice in unintentional injury, violence, and suicide prevention, health education, and public health. The recommendations represent the state-of-the-science in school-based unintentional injury, violence, and suicide prevention. However, every recommendation is not appropriate or feasible for every school to implement nor should any school be expected to implement all recommendations. Schools should determine which recommendations have the highest priority based on the needs of the school and available resources. As more resources become available, schools could implement additional recommendations to support a coordinated approach to preventing unintentional injuries, violence, and suicide. UNINTENTIONAL INJURY, VIOLENCE, AND SUICIDEAn injury is defined as "unintentional or intentional damage to the body resulting from acute exposure to thermal, mechanical, electrical, or chemical energy or from the absence of such essentials as heat or oxygen" (3). Injuries can be further classified based on the events and behaviors that precede them as well as the intent of the persons involved. At the broadest level, injuries are classified as either violence or unintentional injuries. Violence is "the threatened or actual use of physical force or power against another person, against oneself, or against a group or community that either results in or has a high likelihood of resulting in injury, death, or deprivation" (10). Types of violence are homicide, suicide, assault, sexual violence, rape, child maltreatment, dating and domestic violence, and self-inflicted injuries. The events that lead to unintentional injuries often are referred to as "accidents," although scientific evidence indicates that many of these events can be predicted and prevented. Major causes of unintentional injuries include motor-vehicle crashes, drowning, poisoning, fires and burns, falls, sports- and recreation-related injuries, firearm-related injuries, choking, suffocation, and animal bites. Approximately two thirds of all deaths among children and adolescents aged 5--19 years result from injury-related causes: motor-vehicle occupants and pedestrians (32%), all other unintentional injuries (14%), homicide (13%), and suicide (10%) (2). Unintentional injuries, primarily those attributed to motor-vehicle crashes, are the leading cause of death throughout childhood and adolescence (Table 1). Homicide is the fourth leading cause of death among children aged 5--14 years and the second leading cause of death among adolescents aged 15--19 years. Suicide is rare among children aged 5--9 years but is the third leading cause of death among adolescents aged 10--19 years (2). Similarly, the relative importance of unintentional injury-related causes of death also changes throughout childhood and adolescence (Table 2). Morbidity caused by injuries is common during childhood and adolescence. Approximately 5.5 million children aged 5--14 years (145.7 per 1,000 persons) visit hospital emergency departments annually because of an injury. Approximately 7.4 million adolescents aged 15--24 years sustain injuries requiring hospital emergency department visits annually (210.1 per 1,000 persons) (11). Injuries requiring medical attention or resulting in restricted activity affect approximately 20 million children and adolescents (250/1,000 persons) and cost $17 billion annually in medical costs (12). HEALTH OBJECTIVES FOR UNINTENTIONAL INJURY, VIOLENCE, AND SUICIDE PREVENTION AMONG YOUNG PERSONSHealthy People 2010 sets an agenda for health promotion and disease prevention for the United States (3). The primary public health concerns are identified as 10 leading health indicators, including injury and violence and mental health; suicide prevention is included under the mental health indicator. To achieve the outcome of reduced morbidity and mortality caused by unintentional injuries, violence, and suicide, Healthy People 2010 includes objectives to
LEADING CAUSES OF CHILD AND ADOLESCENT INJURY MORTALITY AND MORBIDITYMotor-Vehicle--Related Injuries Motor-vehicle--related injuries are the leading cause of death from injuries among children and adolescents aged 5--19 years in the United States (2) (Table 2). Among this age group, 70% of unintentional injury deaths are caused by motor-vehicle crashes (2). Each year, approximately 1.5 million children and adolescents aged 5--24 years visit the hospital emergency department because of injuries received in motor-vehicle crashes (11). The likelihood that children and adolescents will sustain fatal injuries in motor-vehicle crashes increases if the driver is using alcohol (13--15); passengers are in the vehicle (16); young children are riding in the front seat rather than the back seat (17); and child safety seats and booster seats are not used or are misused (17,18). Traffic-related injuries also include those sustained while walking, riding a bicycle, or riding a motorcycle. In 1998, among children and adolescents aged 5--19 years, a total of 778 deaths occurred among pedestrians; 148 deaths occurred among those riding motorcycles, and 260 deaths occurred among those riding bicycles (2). Among the bicycle-related deaths, 90% were attributed to collisions with motor vehicles (2). Children and adolescents aged 10--14 years have the highest rate of bicycle-related fatalities. Severe head injuries are responsible for 64%--86% of bicycle-related fatalities (19,20). Violence During 1981--1990, the homicide death rate among children and adolescents aged 5--19 years increased 47%, whereas the rate among the overall U.S. population decreased by 2% (2). During 1990--1998, the homicide death rate decreased 30% among children and adolescents and 29% among the overall population (2). The U.S. child homicide rate (2.6 per 100,000 for children aged <15 years) is five times higher than the rate of 25 other industrialized countries combined (21). In the United States, minority males bear the majority of the burden of homicide victimization. In 1998, the homicide death rate among males aged 15--19 years was 5.0 per 100,000 among white, non-Hispanic males; 11.0 per 100,000 among Asian/Pacific Islander males; 23.0 per 100,000 among American Indian/Alaskan Native males; 33.5 per 100,000 among Hispanic males; and 72.5 per 100,000 among black, non-Hispanic males (2). In absolute numbers, more black, non-Hispanic males die from homicide (1,058 in 1998) than white (332), Asian/Pacific Islander (41), American Indian/Alaskan Native (22), and Hispanic (472) males combined. Violence that occurs or is threatened within the context of dating or courtship is referred to as dating violence (22). Approximately 20% of female high school students have reported being physically or sexually abused by a dating partner (23). An increased proportion of male and female high school students have been victims of nonsexual dating violence (24--27). Twenty-five percent of male and female students in eighth and ninth grade have been victims of nonsexual dating violence, and 8% have been victims of sexual dating violence (e.g., nonconsensual sexual contact, completed or attempted rape, abusive sexual contact, or noncontact sexual abuse) (28). Some studies have indicated that males and females inflict and receive dating violence in equal proportion (25,29,30). Other studies report that females are victims of dating violence twice as often as males, that females sustain substantially more injuries than males, and that females more often act for self-defensive purposes than males (31,32). Female high school students who have experienced dating violence are more likely to engage in substance use, unhealthy weight-control practices, and sexual risk behaviors; to have ever been pregnant; and to have considered or attempted suicide (23). Community and family instability, housing and population density, extreme poverty (particularly in close physical proximity to middle-class households), and high residential mobility are associated with community violence (33--39). Exposure to media violence is associated with aggressive behavior in children (40). Children are exposed regularly to violence in news broadcasts (41), music videos (42), electronic games (43), and G-rated animated films (44). A recent study indicated that an intervention to reduce television, videotape, and video game use decreased aggressive behavior in elementary school students (45). The relation between media violence and aggressive behavior could be mediated by cultural and group norms (46). For example, children who live in communities where aggressiveness is unacceptable are less likely to react aggressively to media violence. The effect of media violence on violent behavior, as opposed to aggressive behavior, is still unclear (47). Physical injuries are not the only consequences of violence; violence affects the emotional, psychological, and social well-being of young persons. The trauma associated with witnessing or being a victim of violence can adversely affect the ability of students to learn (48--54). Childhood maltreatment also increases the likelihood that young persons will engage in health risk behaviors (55--57), including suicidal behavior (58) and delinquent and aggressive behaviors in adolescence (59,60). Being victimized as a child also might increase the risk for victimizing others in adulthood (61,62). Childhood maltreatment has been linked to several adverse health outcomes in adulthood, including mood and anxiety disorders (63,64), and diseases, including ischemic heart disease, cancer, and chronic lung disease (55). Suicidal Behavior and Ideation In 1998, a total of 2,061 children and adolescents aged 5--19 years died by suicide in the United States (2). One of the first detectable indications of suicide contemplation is suicidal ideation and planning. In 1999, a total of 19% of high school students had suicidal thoughts and 15% had made plans to attempt suicide in the year preceding the survey (65). Three percent of high school students reported making a suicide attempt that required medical treatment during the preceding year. Students attending alternative high schools are at even higher risk. In 1998, 21% made a suicide plan, 16% attempted suicide, and 7% made a suicide attempt that required medical attention (66). Mental disorders, including depressive disorders and substance abuse, are present in the majority of adolescent suicide victims (67--73). Those with more than one psychiatric diagnosis are at an increased risk for attempted suicide (69). Other risk factors, which can interact with mental disorders to increase risk for adolescent suicide, are family discord, arguments with a boyfriend or girlfriend, school-related problems, hopelessness, and contact with the juvenile justice system (68,72,74--76). Exposure to the suicide of others also might be associated with increased risk for suicidal behavior (69,71,77--80). Sexual Assault and Rape An estimated 302,100 women and 92,700 men are forcibly raped each year in the United States (81). Approximately one half of female rape victims were aged <18 years when they experienced their first rape (81). Females aged 18--21 years have the highest rate of rape or sexual assault victimization (13.8 per 1,000) followed by those aged 15--17 years (12 per 1,000), 22--24 years (11.8 per 1,000), and 12--14 years (6.7 per 1,000) (82). Being raped before age 18 years doubles the risk for subsequent sexual assault; 18% of women raped before age 18 years were also rape victims after age 18 years, compared with 9% of women who did not report being raped before age 18 years (81). Sexual violence is often perpetrated by someone known to the victim (83--86). During 1992--1993, approximately one half of the 500,000 rapes and sexual assaults reported to police by females aged >12 years were committed by friends, acquaintances, or relatives; 26% were committed by intimate partners (84). CONTEXT OF INJURY OCCURRENCEInjuries occur in the context of physical and social environments and in many different settings (87). This section describes injuries related to school, sports, and work. School-Related Injuries Injury is the most common health problem treated by school health personnel. One study reported that 80% of elementary school children visited the school nurse for an injury-related complaint (88). Approximately 10%--25% of child and adolescent injuries occur on school premises (12,89--91). Approximately 4 million children and adolescents are injured at school per year (12). However, the majority of school injuries are minor; serious injuries are more likely to occur at home or in the community. Emergency medical service (EMS) dispatches to schools represent 6% of all EMS incidents for school-aged children (92). Fatalities at school are rare; approximately 1 in 400 injury-related fatalities among children aged 5--19 years occur at school (93). No national reporting system for school-associated injuries or violence exists (94). In 31% of states and 90% of districts, schools are required to write an injury report when a student is seriously injured on school property (95). Among the states that require injury reports, only two require districts or schools to submit injury report data to the state education agency or state health department (95). The majority of injuries at school are unintentional, not violent. Injuries at school are most likely to occur on playgrounds (particularly on climbing equipment), on athletic fields, and in gymnasiums (89,96--102). Injuries during shop class account for 7% of injuries at school (103). The most frequent causes of school-associated injuries resulting in hospitalization are falls (43%) and sports activities (34%) (100). Assaults account for 10% of school-associated injuries resulting in hospitalization (100). Male students are injured 1.5 times more often than female students (93,97), and males are three times more likely than females to sustain injuries requiring hospitalization (100). Middle and high school students sustain more injuries at school than elementary school students: 41% of victims are aged 15--19 years; 31% are aged 11--14 years; and 28% are aged 5--10 years (93). Although shootings in U.S. schools have captured media and public attention, homicides and suicides rarely are associated with schools. Fewer than 1% of homicides and suicides among children and adolescents are school-related (104). During 1992--1994, 105 school-associated violent deaths occurred in the United States, including 85 homicides and 20 suicides (104). These deaths occurred in 25 states, in both primary and secondary schools, and in communities of all sizes. Approximately three fourths of the victims (72%) were students, and 83% were male. Firearms were the method of injury in 77% of the fatalities. Approximately 30% of fatal injuries occurred inside school buildings, and 35% occurred outdoors on school property. The remaining fatalities occurred off campus, either on the way to or from school or at or in transit to or from school-sponsored events. Approximately the same number of students die in school bus-related crashes each year as die from school-related homicides. An average of 29 school-aged children die in school bus-related traffic crashes annually: 9 as school bus occupants and 21 as pedestrians (105). During 1989--1999, a total of 1,445 persons died in school bus-related crashes (105). A majority of fatalities (65%) involved occupants of other vehicles involved in the crash. Nonoccupants (e.g., pedestrians and bicyclists) accounted for 25% of the fatalities, and school bus occupants accounted for 10%. Sports-Related Injuries In the United States, approximately 8 million high school students participate in school- or community-sponsored sports annually (65). Approximately one million serious (i.e., injuries resulting in hospitalization, surgical treatment, missed school, or one half day or more in bed) sports-related injuries occur annually to adolescents aged 10--17 years (106), accounting for one third of all serious injuries in this age group. From 1996 to 1998 in Washington, D.C., approximately 5% of the adolescent population visited a hospital emergency department because of >1 sports-related injuries (107). Sports cause approximately 55% of nonfatal injuries at school (91). Each year, approximately 300,000 mild to moderate traumatic brain injuries are classified as sports-related (108). Males are twice as likely as females to sustain a sports-related injury, probably because males are more likely than females to participate in organized and unorganized sports that pose the highest risk for injury (e.g., football, basketball, gym games, baseball, and wrestling) (100,107,109,110). Among sports with substantial numbers of female participants, gymnastics, track and field, and basketball pose the highest risk for nonfatal injury (111,112). Among sports with male and female teams (e.g., soccer and basketball), the female injury rate per player tends to be higher than the male injury rate per player (113). Children and adolescents also are involved in recreational activities (e.g., in-line skating, skateboarding, and scooter use) that pose substantial injury risks. The most common injuries to in-line skaters seen in hospital emergency departments are wrist injuries (114,115). Hospitalization data indicate that skateboarders are more likely to sustain head injuries than in-line skaters or roller skaters, but the latter two groups are also at risk (116). Since a new version of lightweight, foot-propelled scooters were introduced in the United States in 2000, hospital emergency departments have treated a large number of scooter-related injuries; an estimated 42,500 persons sought emergency department care for scooter-related injuries during 2000 (U.S. Consumer Product Safety Commission, oral communication, August 2001). Approximately 85% of persons treated were aged <15 years. Similar to injuries from skateboarding and in-line skating, the majority of injuries were to the arm or hand (117). Many sports injuries are a result of reinjury (118). One such injury, called second impact syndrome, is a result of repeated mild brain concussions over a short time (119). Severity of concussions increases with recurrent injuries (120). Second impact syndrome might lead to severe traumatic brain injuries and death (119). Other reinjuries (e.g., those occurring to the knee or ankle) can lead to lasting disability (121--123). Work-Related Injuries Approximately 5 million adolescents and children are legally employed; 1--2 million more could be employed illegally, working at less than minimum wage or with dangerous and prohibited equipment (124). One half of all adolescents aged 16--17 years and 28% of those aged 15 years are employed (125). Approximately one half (46%) of high school seniors work >19 hours per week during the school year as well as 25% of students in the ninth grade (126). Although working has many benefits (e.g., earning money, developing employability skills, and building responsibility), potential health risks also result (127). In 1992, approximately 64,000 adolescents aged 14--17 years required treatment in a hospital emergency department for injuries sustained at work. Approximately 70 adolescents aged <18 years die on the job each year (128). Adolescents are most commonly employed in the retail and service sector, particularly in fast-food and other restaurants, but they also work in construction, commercial fishing, manufacturing, and agriculture (124). Adolescents are exposed to many hazardous conditions at work, including ladders and scaffolding, tractors, forklifts, restaurant fryers and slicers, motor vehicles, and night work (127). In particular, motor vehicles and machinery frequently are associated with injuries and deaths that occur on the job (129,130). Night work is associated with an increased risk for homicide, which is the leading cause of death on the job for females of all ages (130). Farming raises special concerns because approximately 2 million children and adolescents live and work on farms and are exposed to farming-related hazards, including tractors, large animals, all-terrain vehicles, farm trucks, rotary mowers, and pesticides (131). Approximately 27,000 children and adolescents aged <20 years who live on farms are injured every year (132). During 1992--1996, a total of 188 agricultural work-related fatalities occurred among persons aged <20 years (133). Injuries on farms are caused primarily by tractors, farm machinery, livestock, building structures, and falls (132,134,135). RISK BEHAVIORS ASSOCIATED WITH INJURYChildren and adolescents can engage in many behaviors that increase their risk for injury. These behaviors often co-occur. Among high school and college students, associations have been reported among suicide ideation, not using seat belts, driving after drinking alcohol, carrying weapons, and engaging in physical fights (136--139). Certain behaviors (e.g., not using helmets or seatbelts, using alcohol, and having access to weapons) can lead to increased risk for multiple causes of injury. Inadequate Use of Helmets or Seat Belts Inadequate use of bicycle and motorcycle helmets or automobile seat belts is associated with many motor-vehicle--related injuries and deaths. Proper use of lap and shoulder belts could prevent approximately 60% of deaths to motor-vehicle occupants (140). Motorcycle helmets might prevent 35% of fatal injuries to motorcyclists and 67% of brain injuries (140). Bicycle helmets might prevent approximately 56% of bicycle-related deaths (141). Proper use of bicycle helmets can eliminate 65%--88% of bicycle-related brain injuries and 65% of serious (i.e., facial fractures and lacerations seen in the emergency department) injuries to the upper and middle regions of the face (142--144). Nationwide, 16% of high school students never or rarely use seat belts when riding in a car driven by someone else (65). Of the 71% of high school students who rode a bicycle in the previous year, 85% rarely or never wore a bicycle helmet (65). Peer pressure and modeling by family members might keep adolescents from using seat belts and bicycle helmets (145--149). Alcohol Use Each month, 50% of high school students drink alcohol on >1 day, and 32% engage in episodic heavy drinking (i.e., consuming >5 drinks on a single occasion) (65). Alcohol use is associated with 56% of motor-vehicle--related fatalities among persons aged 21--24 years, 36% of fatalities among those aged 15--20 years, and 20% of fatalities among children aged <15 years (150). During 1985--1996, a total of 5,555 child passengers aged 0--14 years died in motor-vehicle crashes involving a drinking driver (15). Among these deaths, 64% occurred while the child was riding with the drinking driver; 67% of the drinking drivers were old enough to be the parent or caregiver of the child (15). Alcohol use is a factor in approximately 30% of all drowning deaths (151), 14%--27% of all boating-related deaths (152), 34% of all pedestrian deaths (153), and 51% of adolescent traumatic brain injuries (154). Alcohol use also is associated with many other adolescent risk behaviors, including other drug use and delinquency (39,155), weapon carrying and fighting (156,157), attempting suicide (136,138), perpetrating or being the victim of date rape (83), and driving while impaired (158). Nationwide, during the previous month, 13% of high school students drove a motor vehicle after drinking alcohol, and 33% rode in a car with a driver who had been drinking alcohol (65). Access to Weapons In 1998, firearms were the mechanism of injury in 78% of homicides and 60% of suicides among children and adolescents aged 5--19 years (2). For every firearm-related death of a person aged <24 years, approximately four firearm-related injuries are treated in hospital emergency departments. In 1992, the rate of nonfatal firearm injuries among adolescents aged 15--24 years was 119.5 per 100,000; for children aged 0--14 years, the rate was 6.7 per 100,000 (159). Persons with access to firearms can be at an increased risk for both homicide and suicide (160--162). The percentage of households with firearms varies across states, ranging from 12% to 41% in northeastern states and from 30% to 57% in the western states (163). In approximately 40% of homes with children and firearms, firearms are stored locked and unloaded (164,165). Although firearms in homes with children aged <18 years are more likely to be stored locked and unloaded than in homes without children, the likelihood of firearms being in the home does not differ with the presence or absence of children (163,164). In 1999, a total of 17% of high school students reported carrying a weapon (e.g., a gun, knife, or club), and approximately 5% reported carrying a firearm during the previous month (65). During the same period, 7% carried a weapon on school property (65). INJURY-PREVENTION STRATEGIESInjury-prevention interventions can target three different periods: before an injury-causing event (e.g., avoiding a motor-vehicle crash by not drinking and driving), during an injury-causing event (e.g., wearing a seat belt), or after an injury-causing event to lessen the severity of an injury (e.g., rapid emergency medical services) (166). Regardless of the period, effective injury-prevention efforts address several factors: the environment, individual behavior, products, social norms, legislation, and policy. Passive injury-prevention strategies that require little or no action on the part of individual persons are often most effective (167,168) but are not always achievable. Product modifications (e.g., integral firearm locking mechanisms), environmental changes (e.g., adding soft surfaces under playground equipment), and legislation (e.g., mandating bicycle helmet use) usually result in more protection to a population than strategies requiring voluntary, consistent, and frequent individual protective behaviors (e.g., unloading and placing firearms in a locked box and asking children to follow playground safety rules). However, behavioral change is a necessary component of even the most effective passive strategies (e.g., personal protective equipment must be used properly and depth and quality of playground surface materials must be maintained regularly) (169). Legislation must be supported by the public and enforced by local authorities (170). The most effective injury-prevention efforts use multiple approaches simultaneously. For example, legislation requiring use of bicycle helmets would be accompanied by an educational campaign for children and parents, police enforcement, and discounted sales of helmets by local merchants (171--173). RATIONALE FOR SCHOOL PROGRAMS TO PREVENT UNINTENTIONAL INJURY, VIOLENCE, AND SUICIDEAccording to the Council of Chief State School Officers, "Schools are society's vehicle for providing young people with the tools for successful adulthood. Perhaps no tool is more essential than good health" (174). Approximately 53 million young persons attend >114,000 schools every day (175). Combining students and adults, one fifth of the United States population can be found in schools (175). Therefore, school-based programs can efficiently reach a majority of the children, adolescents, and many adults in the United States. Schools have a responsibility to prevent injuries from occurring on school property and at school-sponsored events. In addition, schools can teach students the skills needed to promote safety and prevent unintentional injuries, violence, and suicide while at home, at work, at play, in the community, and throughout their lives. Coordinated School Health Programs Schools can promote the acquisition of lifelong unintentional injury, violence, and suicide-prevention skills through strategies that provide opportunities to practice and reinforce safe behaviors. However, educational interventions alone cannot produce major reductions in injury or injury risks. Effective school-based injury-prevention efforts address policies and procedures, staff development, the physical environment of the school, and the curriculum in a coordinated manner (176). School efforts to promote safety can be part of a coordinated school health program, which is "an integrated set of planned, sequential, and school-affiliated strategies, activities, and services designed to promote the optimal physical, emotional, social, and educational development of students. A coordinated school health program involves and is supportive of families and is determined by the local community based on community needs, resources, standards, and requirements. It is coordinated by a multidisciplinary team and accountable to the community for program quality and effectiveness" (5). Just as individual strategies cannot be implemented in isolation from each other, schools cannot effectively address unintentional injury, violence, and suicide problems in isolation. School personnel, students, families, community organizations and agencies, and businesses can collaborate to develop, implement, and evaluate injury-prevention efforts. Ideally, coordinated school health programs should include multiple components (e.g., comprehensive health education; physical education; school health services [school counseling, and psychological and social services]; school nutrition services; healthy and safe school environment; school-site health promotion for staff members; staff development; and family and community involvement (177). Coordinated school health programs can improve the health, safety, and educational prospects of students (4,178--184). HOW THE GUIDELINES WERE DEVELOPEDCDC reviewed published literature (i.e., peer-reviewed journal articles, books, private and government reports, and websites) to identify approximately 200 strategies that schools could implement to prevent unintentional injuries, violence, and suicide. Few strategies had been subjected to scientific evaluation, thus a consensus approach involving specialists in various disciplines was used to generate these guidelines. CDC convened a panel of specialists in unintentional injury, violence, and suicide prevention; school health; and mental health services. The panelists considered available evidence of effectiveness at each step of the development process and based many decisions on behavior change theory and best practices in unintentional injury, violence, and suicide prevention; health education; and public health. The panel employed a two-round Delphi technique (185,186) to reach a group decision regarding which recommendations to include in this report. The first-round questionnaire listed the 200 strategies, organized by coordinated school health program components, identified by the literature review. The panelists rated the extent to which evidence existed to support each strategy, the effectiveness of each strategy, and the feasibility for schools to implement each strategy. Panelists considered their ratings on evidence, effectiveness, and feasibility to arrive at a priority score for each strategy. In addition, panelists considered each strategy separately, rather than ranking strategies against each other. The second-round questionnaire listed the strategies that received the highest priority scores within each coordinated school health program component. Panelists considered the group results and their individual scoring on the first-round questionnaire to decide how to rank the strategies. Panelists ranked strategies within each component rather than across all strategies to ensure that all components of a coordinated school health program were addressed. The results of the second-round questionnaire were mailed to the panelists before a meeting of the panel in December 1999. At the meeting, the panel reviewed the resulting outline for the guidelines in this report. They reached consensus as to whether any strategies that were not included in the outline should be included and whether there were strategies that should be removed from the outline. In January 2001, national nongovernmental organizations representing state and local policy makers; educators; parents; specialists in unintentional injury, violence, and suicide prevention as well as other federal agencies involved in unintentional injury, violence, and suicide prevention; and representatives of state and local agencies reviewed a draft version of this report. The report was revised based on their review. SCHOOL HEALTH RECOMMENDATIONS TO PREVENT UNINTENTIONAL INJURIES, VIOLENCE, AND SUICIDEThis section describes eight broad recommendations for school health efforts to prevent unintentional injury, violence, and suicide (Box 1). The recommendations address school environment, instruction, services, and persons. Following this list are strategies for implementing the recommendations. The strategies are grouped by guiding principles that describe essential qualities of coordinated school health programs to prevent unintentional injury, violence, and suicide. The recommendations, guiding principles, and strategies are not prioritized. Instead, they represent the state-of-the-science in school-based unintentional injury, violence and suicide prevention. However, every recommendation is not appropriate or feasible for every school to implement, nor is it feasible to expect any school to implement all of the recommendations. Schools should determine which recommendations have the highest priority based on the needs of the school and available resources. As more resources become available, schools could implement additional recommendations. CDC and others are developing tools to help schools implement the recommendations and strategies included in this report. Recommendation 1: Establish a Social Environment That Promotes Safety and Prevents Unintentional Injuries, Violence, and Suicide.The social environment of a school encompasses the formal and informal policies, norms, climate, and mechanisms through which students, faculty, and staff members interact daily. A social environment can promote safety or contribute to increased risk for unintentional injuries, violence, and suicide (187). Schools can implement strategies to improve the social environment schoolwide (e.g., those designed to create a climate of caring and respect) as well as implement selected activities for students at higher risk (188--190). Not every strategy is appropriate for every school; even within schools, different approaches will be needed for different students. To promote safety and prevent unintentional injuries, violence, and suicide, schools can implement the following guiding principles (Box 2). Ensure High Academic Standards and Provide Faculty, Staff Members, and Students with the Support and Administrative Leadership to Promote the Academic Success, Health, and Safety of Students. Schools cannot accomplish their academic mission without addressing the health and safety needs of students and staff members. Students who are sick, scared, intimidated, anxious, or depressed will not be able to succeed (i.e., achieve academically), no matter how good the school (191). Engaging in injury-related risk behaviors is associated with poor performance on standardized tests, poor class grades, lower graduation rates, and behavioral problems at school (192). Conversely, academic success (i.e., academic achievement) is associated with a decreased likelihood of engaging in health risk behaviors (193,194). Health and academic success are reciprocal (195). Persons who have more years of education experience better health than those with fewer years of education (196). Similarly, persons who engage in health-promoting behaviors during adolescence achieve higher levels of education in adulthood (197). Schools can set standards that convey the expectation that all students will achieve academically. To do so, schools need supportive leaders who will promote the success of students and contribute to students' academic success by supporting safety strategies in school (198,199). An important step in providing administrative leadership to promote academic success is the establishment of a strong academic mission, developed in cooperation with students, faculty, families, and community members (199). Working together to create a mission statement can give all the members of the school community a common focus. The mission statement can recognize the need for healthy and safe students and a supportive and safe school environment to achieve the objective of providing a quality education. The mission statement also can identify and promote a set of core beliefs that support responsible, safe, and ethical behavior appropriate to each school's specific culture. Schools might post the mission statement throughout the school and communicate it to families at the beginning of each school year to reinforce the school's commitment to safety and academic success and to encourage family involvement. Schools can ensure that all students succeed through the implementation of programs designed to help students experiencing barriers to learning. The trauma associated with witnessing violence or being a victim of a serious unintentional injury (e.g., repetitive head injury) or violent event (e.g., child abuse) can have an adverse effect on the ability of students to learn (48--51,53,200). For students experiencing such barriers to learning, the effect on academic success can be critical. Students living in poverty, those with different learning styles, and those with special health-care needs also experience barriers to learning that might negatively affect their success in learning (50,201). Schools can employ several support mechanisms to address such barriers to learning (202). Academic support mechanisms include counseling, mentoring, tutoring, and assistance in the classroom. School-based activities and services to promote mental health also can reduce barriers to learning (203). Family and community members also can serve as support mechanisms to engage students. Students find success in various ways. Opportunities to experience and explore interests in areas such as athletics, drama, art, music, vocational education, and community service can provide avenues for students to experience success and become engaged with their school and community (193). Self-efficacy increases when successes are acknowledged and reinforced by the school, teachers, peers, families, and communities. Schools can develop relationships with communities to increase the range of experiences for students and to bring community resources into the school (198,199). Encourage Students' Feelings of Connectedness to School. Students who like their school and feel connected to their school are less likely to experience emotional distress and suicidal thoughts; are less likely to drink alcohol, carry weapons, or engage in other delinquent behaviors; and are more likely to wear seat belts and bicycle helmets and use prosocial skills (e.g., cooperation, conflict resolution, and helping others) (183,204--210). Students who are engaged in school also might be more likely to do well in school (201,207,211). To encourage connectedness, schools can
All members of the school community could be offered the opportunity to identify their concerns regarding unintentional injury, violence, and suicide and methods for addressing those concerns. When persons participate in decision making regarding their own lives and communities, they tend to be healthier and more productive (212). Schools can create mechanisms to increase faculty, staff member, family, student, and community member participation in making decisions concerning school unintentional injury, violence, and suicide-prevention policies and activities (213--216). This same broadbased involvement can extend to development and implementation of programs. Activities such as mentoring, tutoring, and advocacy groups (e.g., Students Against Destructive Decisions [SADD]) provide opportunities to prevent unintentional injuries, violence, and suicide; build leadership skills; and promote academic success. Designate a Person with Responsibility for Coordinating Safety Activities. A person at each school building and at the district level might be designated to have responsibility for coordinating safety activities. This could be the school health coordinator, a counselor, or the principal. Schools also can establish a committee that focuses on unintentional injury, violence, and suicide prevention within their school health council, school improvement team, or other existing group focused on improving the health, safety, and well-being of students and staff members (217,218). The committee can have representation from key school constituencies: students, faculty, staff members, families, and community members (219,220). Such committees can meet regularly to assess needs; consider and respond to student, family, or community concerns for safety; and oversee design, implementation, and evaluation of unintentional injury, violence, and suicide prevention and emergency preparedness policies, programs, and services (215). School safety committees or school health councils can strive to increase collaboration between schools and community agencies (e.g., local law enforcement, fire departments, EMS providers, public health agencies, social services, and mental health providers) (198,220). School safety committees or school health councils can also help schools compose effective responses to school safety concerns. Establish a Climate That Demonstrates Respect, Support, and Caring and That Does Not Tolerate Harassment or Bullying. Students are more likely to feel connected to school if they 1) believe that they are treated fairly, 2) feel safe, and 3) believe that teachers are supportive (221). Students who think that their teachers are supportive of them are less likely to drink alcohol and are more likely to wear seat belts and bicycle helmets than are students who think that their teachers are not supportive (183). School personnel can work together with students and families to create a school climate that is supportive and productive for all students (222--224). Schools also can identify components of the school climate (e.g., sexual harassment) or physical environment (e.g., poorly lighted areas) that might contribute to injuries, violence, and victimization at school and make changes as appropriate. Students who are at increased risk for unintentional injury, violence, and suicide and students who represent the diverse population of the school could be offered the option to be included in solving problems and making decisions. School norms for teachers, staff members, and students can support positive, prosocial, helping behaviors and discourage bullying, discrimination, intimidation, violence, or aggression (198,199,215,225). For example, adult supervisors on playgrounds and in the hallways can express disapproval of pushing, shoving, or sexual harassment. In approximately three fourths of school shootings studied by the U.S. Secret Service, attackers told someone their plans before the attack (226). Schools can create a climate in which students feel comfortable reporting violations of policies or warning signs of violent or suicidal behavior (226). Regardless of a child's ethnic, socioeconomic, religious, sexual orientation, or physical status, all children have a right to safety (224,227,228). When victimization through bullying, verbal abuse, and physical violence is prevalent in a school, the entire school community experiences the consequences. When abuse against a particular group is perceived as acceptable, intergroup hatreds can become established (229). Bullying is the repeated infliction or attempted infliction of injury, discomfort, or humiliation of a weaker student by one or more students with more power (224,230). Bullying is common in many U.S. schools. One out of ten (10.6%) U.S. students in grades 6 through 10 have reported being bullied, and 13% have reported bullying others (231). Appearance and social status are two main determinants of being the victim of bullying (230). In surveys of students in grades 8 through 12, and 4 through 8, the highest ranked reasons for being bullied among both boys and girls was that the victim "didn't fit in" (229,232). Students who are different from the majority of their classmates because of their race, ethnicity, sexual orientation, religion, or other personal characteristics are at increased risk for being bullied. Gay, lesbian, or bisexual students, and students perceived to be gay by their peers are often victims of repeated verbal abuse and physical assault (228,233--235). Students who are socially isolated and lack social skills also are likely to be victims of bullying (231). Students who are repeatedly victims of such abuse and assaults are at increased risk for mental health problems and suicidal ideation (233). Students who inflict such abuse suffer consequences as well. By middle childhood, the outcomes for extremely aggressive children include rejection by peers who behave better and academic failure; these outcomes set the foundation for delinquency in later childhood and adolescence (224,230). Schools can establish high expectations for and encourage prosocial behaviors. The entire school, especially the principal and other school leaders, can commit to good behavior (230). Schools can set high expectations for faculty and staff members, who can be role models of prosocial behaviors when they interact with each other and students (223). For example, faculty can be respectful and polite in their dealings with custodial and other support staff and with students. The standards can apply to families and students as well. School events and routine conferences with parents provide opportunities to highlight and support standards. For example, fair play and nonviolence can be emphasized at school sporting events. Members of the school community who meet these standards can receive positive reinforcement for their behaviors (198). Develop and Implement Written Policies Regarding Unintentional Injury, Violence, and Suicide Prevention. Written policies provide formal rules that guide schools in planning, implementing, and evaluating unintentional injury, violence, and suicide-prevention activities for students. School policies related to unintentional injury, violence, and suicide prevention should comply with federal, state, and local laws (236). Similarly, schools should consider recommendations and standards provided by national, state, and local agencies and organizations when establishing policies. Unintentional injury, violence, and suicide-prevention policies can be part of an overall school health policy. These policies can be based on assessments of local needs and input from the school and community and can include procedures for communicating the policy and enforcing it. In addition, these policies can be developed and written with input from persons who are specialists in pertinent disciplines, those who will be affected by the policy, and those who will be responsible for implementing the policy. Sources of model policies are included in this report (Appendix B). Unintentional injury, violence, and suicide-prevention policies could
Infuse Unintentional Injury, Violence, and Suicide Prevention into Multiple School Activities and Classes. Unintentional injury, violence, and suicide prevention can be infused into many aspects of the school. For example, several states require schools to issue employment certificates to students before they can begin employment (242). Schools can use the process of issuing employment certificates to foster communication between the school, the employer, the student, and the family regarding occupational safety and the relation between academic success and employment. Schools also can link permission to work to a student's educational performance and ensure that youth are engaged in work that is in compliance with child labor laws before issuing employment certificates (242). Schools can also infuse unintentional injury and violence prevention into academic classes. Although addressing unintentional injuries and violence as specific health concerns is important, these topics can also be infused into the other components of the curriculum (243--245). For example, an activities-based teacher's guide demonstrates how physics courses can explore the energy exchanges that occur in motor-vehicle or bicycle crashes and how seat belts and bicycle helmets absorb energy to prevent injuries (246). History courses could explore the causes and consequences of violence, using examples from events such as wars and civil disturbances. Similarly, principles of nonviolence and prosocial behavior could be infused into physical education and sports participation. The majority of adolescent risk behaviors are interrelated (136--139,247,248), so unintentional injury, violence, and suicide prevention also can be integrated into existing programs that address other risk behaviors (e.g., sexual risk, tobacco use, or alcohol abuse) and that promote social skill development (139,248). Unintentional injury, violence, and suicide prevention; and social skill development fit into programs and curricula that help students transition to the adult workforce (e.g., vocational education and school-to-work programs) (249). Establish Unambiguous Disciplinary Policies; Communicate Them to Students, Faculty, Staff Members, and Families; and Implement Them Consistently. Discipline is the process through which appropriate and safe behaviors are taught. Schools can emphasize increasing prosocial behaviors and skills (e.g., social competence, problem solving, autonomy, and role modeling) among faculty, staff members, and students. Disciplinary policies need to be stated unambiguously and implemented consistently to be effective. Prosocial behaviors exemplified by faculty, staff members, and students can be publicly acknowledged and rewarded. Disciplinary policies can explicitly describe codes of conduct for all members of the school community, focusing on prosocial behaviors, but can also include rules prohibiting unsafe or violent behavior (199,215). Policies can explicitly explain the consequences for breaking rules and provide for due process for persons accused of breaking rules (224,241). Humiliating, harassing, and physically aversive punishment intended to cause emotional or physical pain could be prohibited. Schools can establish a mechanism for involving students, families, faculty, and staff members to ensure that disciplinary practices are maintained in a consistent and appropriate fashion (e.g., student courts). Alternatives to expulsion that will improve student behavior and school climate could be considered (250). Alternatives that retain suspended or expelled students within an educational atmosphere (e.g., alternative schools or in-school suspension) are essential to maintaining the student's connection with school and academic work (188,198). However, simply referring students to alternative educational settings is not sufficient. These programs should be of high quality and should limit the potentially harmful effects of grouping students at high risk. Effective alternative programs can support students and provide them with opportunities to learn how to manage inappropriate behaviors (188,198). The Individuals with Disabilities Act (IDEA) requires states to provide students with disabilities a free and appropriate public education that meets their unique needs. This act prohibits expulsion or suspension of students based on their disabilities but does not prohibit expulsion or suspension for other reasons. However, a school seeking to expel or suspend a student receiving educational services under IDEA must comply with IDEA procedures, including parental involvement and endorsement. Assess Unintentional Injury, Violence, and Suicide-Prevention Strategies and Policies at Regular Intervals. Schools can regularly assess the fidelity with which they are implementing unintentional injury, violence, and suicide-prevention strategies and policies (239,251). To be effective, schools should consider collecting data on an ongoing basis to monitor progress and continuously improve school efforts (198,252). Many schools already collect information that can assist in monitoring their efforts. For example, over time, schools could examine changes in the environment (e.g., addition of safety features and improvements to playground equipment and surfacing), the school (e.g., rates of policy violations, expulsions, and absenteeism), and in students (e.g., knowledge, attitudes, skills, behaviors, and injuries). Assessment can be one role of the school safety coordinator or committee. Schools can use existing data sources (e.g., injury records, attendance records, maintenance reports, student discipline records, and expulsion records) to monitor several of these changes. For example, a school can track the number of injuries that occur on the playground before and after the installation of new surfacing material. All groups affected by the prevention strategies can be given the opportunity to provide input into the evaluation and to participate in making changes based on evaluation findings. However, schools must comply with all federal and state laws regarding information sharing (253,254). Schools can consult with evaluation specialists at universities, school districts, or the state departments of education and health to identify methods and materials for evaluating their efforts. Valid evaluations can improve the quality of school programs, increase family and community support, help schools reward faculty, staff members, and students for exceptional work, and support grant applications for enhancing activities. Recommendation 2: Provide a Physical Environment, Inside and Outside School Buildings, That Promotes Safety and Prevents Unintentional Injuries and Violence. The physical environment of a school (including campus walkways and grounds, playgrounds, sports fields, parking lots, driveways, school vehicles, gymnasiums, classrooms, shop and vocational education classrooms, cafeterias, corridors, and bathrooms, as well as other environments in which students engage in school activities) and the equipment used in these places can affect unintentional injuries and violence. Schools can implement a range of actions to ensure that the physical environment helps to prevent unintentional injuries and violence to the maximum extent possible. By creating a physical environment that promotes safety, schools also can model for students and families the importance and ease of maintaining a safe environment (Box 3). Conduct Regular Safety and Hazard Assessments. Schools should consider doing a comprehensive safety assessment at least annually (239). More frequent assessments (e.g., monthly) will be needed for some areas of the school, particularly playgrounds and sports fields (100). One person can be given the responsibility for identifying hazards and ensuring maintenance of the school environment. Procedures for reporting hazards to the responsible person could be developed and publicized. Sufficient funding will be necessary to support inspection, repair, and upgrades as needed. Maintain Structures, Playground and Other Equipment, School Buses and Other Vehicles, and Physical Grounds; Make Repairs Immediately Following Identification of Hazards. Facilities can be maintained and hazards repaired immediately after they are identified. Characteristics of safe environments include the following:
States should comply with Occupational Safety and Health Administration (OSHA) regulations regarding safe working conditions. Approximately one half of states have state level occupational safety and health agencies. Some state regulations protect employees, including school staff members and faculty, from hazards at their workplace. By establishing a safer environment, compliance with these regulations also offers some protection to students. OSHA regulation coverage ranges from general classroom conditions to machine guarding in industrial arts classes, to hazard communication for materials used in science and arts classes. CDC's National Institute for Occupational Safety and Health (NIOSH) has compiled a CD-ROM with information regarding applying OSHA regulations to schools (255). Schools should also consider National Highway Traffic Safety Administration (NHTSA) guidance regarding school transportation safety. NHTSA guidance addresses the identification, operation, and maintenance of buses used for carrying students; training of passengers, pedestrians, and bicycle riders; and administration of student transportation services (256,257). NHTSA also provides guidance on the proper use of child safety restraint systems in school buses (258). Properly located and working smoke alarms, sprinklers, and fire extinguishers are essential (245). Approximately 6,000 structure fires occur in schools each year, resulting in 139 injuries and direct property damage exceeding $63 million (259). Only one half of all reported fires in educational properties occur in schools with working smoke or fire alarms (259). Automatic sprinkler systems are present in only 23% of these schools where fires occur (259). Schools can check to ensure that their smoke alarms and fire extinguishers are properly positioned and working, and regularly test sprinkler systems as well. Faculty and staff members can be taught to use fire extinguishers. The safety of playground equipment and surfaces can be ensured by using standardized playground safety checklists and equipment guidelines (e.g., U.S. Consumer Product Safety Commission, National Program for Playground Safety, Consumer Federation of America) (260,261). Information regarding accessing these resources is included in this report (Appendix B). Schools can pay particular attention to:
Personal protective equipment (e.g., safety glasses, gloves, and earplugs) could be required in industrial arts, science, art, home economics, and other classes where students and staff members are exposed to potentially dangerous equipment. Schools can provide personal protective equipment and maintain its quality and hygiene (100,239,245). All machinery and other equipment used by students in these classes should be assessed regularly and maintained for safety (218). In particular, assessments should determine whether safety features have been removed or disabled and whether machinery and other equipment are being used properly. Damaged equipment should be replaced. All pedestrians, especially young children, can be offered special protection (263). Depending on the community, this special protection might include crossing guards, escorts, crosswalks, or other traffic calming measures (218,264). Safe bus and car loading zones should be located away from vehicular traffic and have appropriate traffic safety devices (e.g., speed bumps and curbs) (240,265). Pathways to and from playgrounds and fields should be safe and located away from vehicular traffic. Schools can work with the local community to ensure safe walking routes to school (264). Schools can assess injury risks for students and staff members with special health-care needs and act to prevent injuries by modifying the environment appropriately (266). Students and staff members with special health-care needs (e.g., those with temporary impairment or permanent disability) can be at increased risk for injuries (100). When students with special health-care needs enter or reenter the school, a thorough review of the school environment should be conducted to identify possible hazards, and the results should be incorporated into their health record (266). Plans should be developed for emergency evacuation of students and staff members with special health-care needs. Vocational education courses are often taken by students with special needs, including many students with learning disabilities. A safe environment is essential for developing vocational skills and learning lifelong safe work practices (267). School-sponsored events that take place off school property (e.g., field trips) can be conducted with optimal safety. Schools are responsible for promoting safety and preventing unintentional injuries and violence whenever students are in their care. Before such trips take place, schools can assess the physical safety of locations to which students will be brought and ensure access to telephones, emergency care, and first aid kits while they are away from school. Students need adequate supervision when they are away from school. Schools can develop a plan that includes student-supervisor ratios and procedures to follow if hazards are identified. Vehicles used to transport students off-site should comply with the NHTSA guidelines for student transportation safety (256). For overnight field trips, schools should consider selecting only hotels that are fully equipped with fire suppression sprinklers and that are in compliance with the Americans With Disabilities Act. Actively Supervise All Student Activities to Promote Safety and Prevent Unintentional Injuries and Violence. Supervision is critical to maintaining an environment that promotes safety and prevents unintentional injuries and violence. Schools can develop and enforce safety rules for physical activities and recreational activities. Staff members supervising physical activities and recreation should be trained in first aid and cardiopulmonary resuscitation (CPR). Schools can ensure active supervision, especially during recess, recreational time, games, physical education, and sporting events (100,176,239). Areas in need of supervision include halls, bathrooms, and playgrounds. In one study in New York, 63% of middle school students reported that the majority of bullying takes place in the hallways, but only 11% of staff members thought that hallways were an important location for bullying (268). Staff members and volunteers can be trained in how to supervise students so that they can be effective in protecting against potentially dangerous situations (268). Active supervision includes observation, listening to students, anticipating and effectively responding to unsafe situations, and promoting positive behaviors. Supervisors could be aware of the developmental appropriateness of each piece of playground equipment and ensure that students do not use inappropriate equipment. Schools might need to consider creative scheduling approaches to reduce the number of students in need of supervision at any one time (e.g., staggering grade level class changes). Students also need active supervision during shop and vocational education activities. A statewide study of shop-related injuries documented that equipment use was associated with 88% of injury incidents (103). Several types of equipment that students use during shop classes (e.g., power saws) are prohibited for use by children aged <18 years in the workplace. Schools can ensure that added protections have been established in classes where these types of equipment are in use. In addition to supervision, this added protection might include additional safety features, regular maintenance of equipment, student training, and matching equipment to student stature (103). Ensure That the School Environment, Including School Buses, is Free from Weapons. Schools can use various mechanisms to decrease the likelihood that weapons will be brought onto school property. Having a pleasant environment (e.g., one free from graffiti) raises expectations for safety. Schools can implement changes in policy, persons, technology, and the environment to improve safety and lessen the likelihood that weapons will be brought onto school property. School weapons policies should comply with the Gun Free Schools Act (GFSA). The GFSA, Part F of Title XIV of the Elementary and Secondary Education Act, requires that each state, as a condition of funding eligibility, have in effect a state law requiring local educational agencies to expel from school, for a period of not less than 1 year, any student who brings a firearm to school. However, each state's law also must allow the chief administering officer of the local educational agency to modify the expulsion requirement on a case-by-case basis. Schools might consider the circumstances of the incident and should exercise due process in determining whether to expel a student (250). In addition, under the GFSA, local educational agencies receiving Elementary and Secondary Education Act funds must adopt a policy requiring any student who brings a firearm to school to be referred to the criminal justice or juvenile delinquency system. The GFSA also states that nothing in the GFSA shall be construed to prevent a state from allowing a local educational agency that has expelled a student from the student's regular school setting from providing educational services to that student in an alternative setting. Many states require that alternative education be provided to students expelled for possessing a firearm on school property (269). Alternative education is essential to maintaining a student's academic work. To support weapons-related policies, schools can work together with families and communities. Schools can notify students, faculty, staff members, family, and the community that weapons will not be tolerated on school property through letters sent home and posted on signs. Schools might also employ volunteers from the community, school resource officers, or others to supervise students and monitor school property. Characteristics of the physical environment (e.g., graffiti and poor lighting) can increase the likelihood of crime and violence (270,271). Schools can make various environmental changes to improve the quality of the school environment (e.g., painting murals instead of graffiti, improving lighting, and planting flowers) and thereby reduce the risk for crime and violence (271,272). Schools also might consider various environmental changes to lessen the likelihood that weapons will be brought onto school property. Environmental changes could include perimeter fencing, sealing off or supervising secluded areas, or limiting the number of entrances into the school building (271). For some schools, security technologies (e.g., cameras or metal detectors) might help keep weapons off school property (273--275). Recommendation 3: Implement Health and Safety Education Curricula and Instruction That Help Students Develop the Knowledge, Attitudes, Behavioral Skills, and Confidence Needed to Adopt and Maintain Safe Lifestyles and to Advocate for Health and Safety. Health education curricula and instruction can be an important component of school efforts to prevent unintentional injuries, violence, and suicide. In 2000, a total of 75% of schools required students to receive instruction on unintentional-injury prevention; 80% required instruction on violence prevention; and 40% required instruction on suicide prevention (CDC School Health Policies and Programs Study, unpublished data, 2000). On average, schools spent a median of 4--5 hours teaching about unintentional injury or violence prevention in a required course (276). Schools can teach about unintentional injury and violence prevention using health education methods grounded in theory and with scientific evidence of effectiveness. In addition, schools can infuse such unintentional injury and violence prevention content into various disciplines, including family and consumer education, physical education, driver education, and vocational education (Box 4). Choose Prevention Programs and Curricula That Are Grounded in Theory or That Have Scientific Evidence of Effectiveness. Schools can select programs and curricula based on identified needs of the school and community, findings from evaluation research, behavior change and education theory, and examples of best practices, and provide training in these programs for school staff members (199,243). Programs and curricula that have been demonstrated not to work to prevent unintentional injuries, violence or suicide, as well as those that have been demonstrated to have negative effects might be discontinued. Guides are available in this report to help schools select violence prevention curricula and broader-based programs with scientific evidence of effectiveness (Appendix C). Although similar guides do not exist for unintentional injury or suicide-prevention programs or curricula, this report does include resources for identifying effective strategies to prevent unintentional injuries and suicide (Appendix C). Community-based specialists, from neighboring universities for example, might provide assistance in identifying effective programs and explaining to the school community the importance of using research-based, evaluated programs. Evaluations of suicide-prevention curricula that promote only awareness have demonstrated few positive and some negative effects (277). Rather than using curricula focused directly on suicide prevention, schools might target risk and protective factors (e.g., alcohol use, bullying, and school connectedness), educate students regarding the consequences of suicidal behavior, and focus on specific subpopulations that might be at higher risk (e.g., gay and lesbian students) (277). Implement Unintentional Injury and Violence-Prevention Curricula Consistent with National and State Standards for Health Education. According to the Joint Committee on National Health Education Standards, the health education curriculum offers students the knowledge and skills they need to "obtain, interpret, and understand basic health information and services and the competence to use such information and services in ways which enhance health" (278). The National Health Education Standards specify that, as a result of health education, students will be able to comprehend concepts related to health promotion and disease prevention; access valid health information and health-promoting products and services; practice health-enhancing behaviors and reduce health risks; analyze the influence of culture, media, technology, and other factors on health; use goal-setting and decision-making skills to enhance health; and advocate for personal, family, and community health. Schools can require comprehensive health education that includes planned and sequential instruction in unintentional injury and violence prevention for students in prekindergarten through grade 12 (278). Unintentional injury and violence prevention can be part of a comprehensive health education curriculum that focuses on understanding the relation between personal behavior, the environment, and health. A Healthy People 2010 objective is to increase the proportion of schools that provide such education (Appendix A). To achieve stable, positive changes in student behavior, adequate time can be allocated for unintentional injury and violence-prevention education and practice. Evidence from other areas of health education indicate that programs and curricula that devote more hours and take place over an extended period are more likely to be effective than shorter-term programs (279--281). Similarly, programs that involve schoolwide and communitywide change are more likely to be effective than those that take place only in the classroom (179). Programs and curricula can begin as early as preschool and be reinforced throughout the school years (225). Curricula can be sequential from preschool through secondary school, and attention should be focused on scope and sequence. Developmentally appropriate educational strategies can be used (225,243,282). Regardless of the amount and quality of teaching they receive, the youngest elementary school students might not fully understand abstract concepts or different perspectives; for example, young children might think a driver can see them and will stop just because they can see the car approaching them (263). Unintentional injury and violence prevention education for young students might focus on concrete experiences (e.g., practice in safely crossing a street or resolving conflicts) (263). More abstract associations among behaviors, environment, and injury risk become appropriate as students approach middle school. Although families still play an important role, peer pressure to engage in risky behaviors can be an even stronger motivator (283). By the time children enter middle school, they can understand and act on the connection between their behaviors and injury. During late adolescence, children prepare to make the transition to the adult world. Intimate relationships and work begin to take on increased importance (284). Therefore, unintentional injury and violence-prevention education for middle and high school students can focus on helping students assess the effect of behavior and environment on safety, setting goals for reducing risks for unintentional injury and violence, and advocating for safe behaviors with peers and younger students. Educational programs should be appropriate to the culture of the community in which they are located (243). Even within a school, students are likely to have diverse experiences, knowledge, attitudes, and behaviors. Rather than adopting a uniform approach, schools need to take these differences into account and use them to increase program effectiveness. Issues of social class, race, ethnicity, language, sexual orientation, and physical ability might be considered when choosing and implementing prevention strategies. Educational efforts might need to be tailored for students with special needs. Activities that promote tolerance and respect for differences are critical. Involving students in developing and implementing programs can help ensure their relevance (285,286). Obtaining input from student members of various cultural groups is essential. Educational activities can help students understand social influences on health- and safety-related behaviors and how to resist cultural, media, and peer pressure to make unsafe choices (278,287). Programs and curricula can focus on building skills students will need throughout their lives. Specific skills that can help prevent unintentional injuries, violence, and suicide include (199,214,222,225,243,288--296)
Young persons who are considering suicide often confide in peers (297--299). Students can learn how to recognize signs of depression, abuse, and distress in themselves and their peers and to respond by contacting helpful adults (e.g., school counselors or nurses) (238,299). Students can learn about effective unintentional injury, violence, and suicide-prevention strategies that affect individual behavior, the environment, injury-causing agents, social norms, legislation, and policy (243). Examples include seat belts, child safety seats, bicycle helmets, minimum drinking age legislation, graduated driver licensing legislation, smoke alarms, mentoring programs, and parenting education (47,140--144,170,296,300,301). Students can also learn the first aid and CPR skills needed to treat injuries and other emergencies (302). Schools can work with communities to increase availability of early childhood education for those at increased risk. Students who come to school lacking important social and emotional skills often fall behind their academically better prepared peers and are at increased risk for behavioral, emotional, academic, and social development problems (303). Early childhood education for children at risk has been demonstrated to decrease unintentional injury, violence and delinquency, and educational difficulties (216,304,305). Schools can teach students how to prevent injuries that can occur on school property and at home, at work, and in the community (239,245). Specific topics might include
Students can be taught developmentally appropriate basic emergency lifesaving skills (e.g., going for adult help, performing first aid and CPR), so they will be prepared to respond to various injury situations (302). Sources of materials that address these topics are included in this report (Appendix B). Use Active Learning Strategies, Interactive Teaching Methods, and Proactive Classroom Management to Encourage Student Involvement in Learning About Unintentional Injury and Violence Prevention. Active learning strategies encourage students' involvement in learning and help them develop the concepts, attitudes, and behavioral skills they need to engage in unintentional injury, violence, and suicide prevention (214,225,286,289,291,320). To engage students in active learning, teachers can use instructional strategies (e.g., supervised practice, discussion, cooperative learning, simulations, teacher and peer modeling, goal-setting, rehearsal, visualization, positive reinforcement, and booster sessions) (204,207,296,321--324). Students should have repeated opportunities to practice using protective devices and skills (e.g., wearing bicycle helmets, testing smoke alarms, testing hot water temperature, and resolving conflicts nonviolently). Schools can involve families, community members, and community resources in the learning process. Unintentional injury and violence-prevention skills can be incorporated into community-based programs (e.g., service learning, volunteering, and community development projects) (181). Parents and family members can be involved through family-based education strategies (e.g., family homework assignments) or through programs that bring adults into schools (e.g., mentoring) (214,296). Programs that focus on involving youth (e.g., mediation, tutoring, peer-led classroom activities, and advocacy groups (SADD; 4-H; and Family, Career, and Community Leaders of America) also can increase student involvement in unintentional injury, violence, and suicide prevention (217,325--329). Proactive classroom management techniques are designed to create calm, orderly classrooms. Techniques include reinforcing positive behaviors, monitoring classroom activity, and promoting cooperative and interactive learning (204,213,214,320,330). Older children are expected to take more responsibility for changing their behaviors than younger children. Proactive classroom management has been demonstrated to reduce problem behaviors in the classroom, aggressiveness, delinquency, and suspensions from school (213,214,320,330,331). Provide Adequate Staffing and Resources, Including Budget, Facilities, Staff Development, and Class Time to Provide Unintentional Injury and Violence-Prevention Education for All Students. Trained staff members, staff development, and adequate budget, facilities, and class time are essential for health education on unintentional injury, violence, and suicide prevention to be successful (278). Persons who teach health education can be trained in health education and unintentional injury and violence prevention and provided with ongoing staff development and support. Elementary schools could hire teachers trained to teach health education and middle and senior high schools could hire health education specialists. For various unintentional injury, violence, and suicide-prevention topics, community agencies and organizations (e.g., fire and rescue departments, and public and mental health agencies) can help teach lessons; however, teachers are usually more effective than outside sources because of their ongoing access to and knowledge of the learning styles and capabilities of their students. Schools can facilitate ongoing staff development to ensure that persons who teach health education have current knowledge of unintentional injury and violence prevention. Teacher-to-student ratios in health education could be comparable to those in other subject areas. Recommendation 4: Provide Safe Physical Education and Extracurricular Physical Activity Programs. Physical education and extracurricular physical activity programs offer many opportunities to teach the skills needed to facilitate lifelong safe participation in physical activity. Physical activity programs can also be positive alternatives to risky behaviors. However, along with increased physical activity participation comes an attendant increase in risk for physical activity-related injury (332). Both physical and social environments play an important role in fostering a sense of safety and enjoyment of physical activity (333,334). Schools can improve the safety of their physical education and other physical activity programs by developing and enforcing safety rules, promoting unintentional-injury prevention and nonviolence, requiring the use of protective equipment, ensuring the safety of the physical environment, and properly training all physical education staff members and volunteers (Box 5). Develop, Teach, Implement, and Enforce Safety Rules. Safe physical activity requires proper conditioning and use of appropriate protective equipment where needed. Dangerous behaviors (e.g., spearing in football, high sticking in hockey, throwing a bat in baseball, and use of alcohol and drugs by athletes) can be prohibited by establishing and enforcing rules (100,176,240). Trained staff members or volunteers should supervise all physical activity programs. To prevent injuries during structured physical activity for students, adult supervisors might
Promote Unintentional-Injury Prevention and Nonviolence Through Physical Education and Physical Activity Program Participation. Physical activity has important health and social benefits across the life span, so schools can prepare students to enjoy physical activity and participate in physical activities safely. Physical activity programs also provide alternatives to risk-taking behaviors that can lead to unintentional injury or violence. Students who participate in sports activities are less likely to engage in health risk behaviors than their peers (341). Schools can offer a range of developmentally appropriate, noncompetitive, and competitive physical activity experiences (339,342) and reward sportsmanship, effort, teamwork, and adherence to safety rules (343,344). Teachers, families, and coaches can model nonviolent behaviors, adhere to safety rules, and use protective equipment. Schools could protect students and others by strictly enforcing prohibitions against alcohol and drug use, and violence or aggression by spectators and other persons during school sporting events. Schools can promote the use of personal protective equipment inside and outside school-associated sports and recreation activities (114,345). Students could be provided with and required to use personal protective equipment appropriate to the type of physical activity (100,334). Personal protective gear (e.g., helmets, eye protection, face and mouth guards, pads, reflective gear for runners and bicyclists, and personal flotation devices) should fit well, be in good condition, and meet national standards (e.g., American National Standards Institute [ANSI], and American Society for Testing and Materials [ASTM]). Protective gear should be inspected frequently and replaced or reconditioned according to national guidelines if worn, damaged, or outdated. Coaches and physical education faculty can be trained in fitting and inspecting personal protective equipment. Schools might engage local physicians and dentists in donating and fitting protective equipment. Schools also can promote the use of personal protective equipment during nonschool-associated sports activities. For example, schools might require helmet use by students who ride bicycles, skateboards, in-line skates, or scooters on school property. Ensure That Spaces and Facilities for Physical Activity Meet or Exceed Recommended Safety Standards for Design, Installation, and Maintenance. Spaces and facilities for physical activity, including playing fields, playgrounds, gymnasiums, swimming pools, and exercise rooms, should be regularly inspected, and hazardous conditions should be corrected immediately (100,218,240,260,262,339,346). Playing surfaces are an important component of the environment where physical education and physical activity programs take place. Schools can ensure
Hire Physical Education Teachers, Coaches, Athletic Trainers, and Other Physical Activity Program Staff Members Who Are Trained in Injury Prevention, First Aid, and CPR and Provide Them with Ongoing Staff Development. Schools should consider hiring physical education teachers certified and trained in physical education and qualified persons to direct school physical activity programs and to coach students in sports and recreation programs (9). To minimize the potential for serious injuries in activities they teach, physical education teachers and physical activity program staff members could be skilled in developmentally appropriate activities and proper conditioning (336). They could be able to provide instruction on the biomechanics of motor skills and proper use of personal protective equipment, match participants according to size and ability, and adapt rules to eliminate unsafe practices, including aggression in sports. Adults, including volunteer coaches, supervising sports activities also should be trained in treating injuries, including first aid, CPR, and use of portable defibrillators. They should also have skills to appropriately triage injuries. Coaches and athletic trainers can be trained in criteria for establishing when students who have sustained injuries, including concussions, can return to play (100,176,239,340). Recommendation 5: Provide Health, Counseling, Psychological, and Social Services to Meet the Physical, Mental, Emotional, and Social Health Needs of Students. Students' risk for unintentional injury, violence, and suicide is affected by their physical, mental, emotional, and social health status. Only a small percentage of children in the United States receive the mental health treatment they need (352). For those children who do receive needed mental health services, schools are the primary providers (352). Schools can play an important role in linking students to community-based health, counseling, psychological, and social services. School-based health services that address physical, mental, emotional, and social health needs in an integrated approach can bring these services to students in need (Box 6). Coordinate School-Based Counseling, Psychological, Social, and Health Services; and the Educational Curriculum. Schools might have several counseling, psychological, social, health, and educational support services. To provide optimum care for students, these services can be coordinated with each other, with additional community-based services, and with families (203). Staff members from various school-based services will need to work together to prevent unintentional injuries, violence, and suicide. Representatives from all counseling, psychological, social, and health services can be included on the school safety committee or school health council and can act as resources for other school personnel. These services can work together to develop mechanisms to help all students feel safe expressing their feelings, not only those identified as being at risk for unintentional injury, violence or suicide (217,353). These services might include schoolwide efforts to reduce stigma associated with receiving counseling. Counseling, psychological, social, and health services staff members can play a substantial role in prevention activities. They might
Schools can employ a multidisciplinary approach to identify and assist students at increased risk for unintentional injury, violence, and suicide (188). Staff members from physical and mental health services can work toward early identification of students experiencing problems and connect these students and their families to school and community resources (189,353). Family members could be included in all aspects of interventions developed for their children. When a student has threatened suicide, school staff members need to focus on ensuring that the student is safe, assessing the level of risk, and referring the student to appropriate care (238). Even brief opportunities to talk with a caring adult might decrease suicide risk (354). Faculty, school nurses, and others might be trained to recognize signs of distress and increased risk for unintentional injury, violence, and suicide and to refer identified students to school and community services (277,282,355). Establish Strong Links with Community Resources and Identify Providers to Bring Services into the Schools. Counseling, psychological, social, and health services could be available to students on an ongoing basis and could be available for primary prevention. Many schools provide on-site health, counseling, psychological, and social services; other schools rely exclusively on community-based resources; and still others employ some combination of school- and community-based services. Mechanisms can be established for referring, monitoring, and tracking students and families. These mechanisms might include procedures for maintaining confidentiality for students (356) and for assisting families with securing funding for these services. Even when a school provides services, linkages can be established with community resources to strengthen services for students (217). School mental health services can be an important source of information for families seeking help for their children. School support services staff members can refer a student or family to social services for child abuse or neglect and know how to follow up with agency staff members (353). Schools can establish communications with community-based agencies that they will need to contact after a student suicide threat or attempt (238). Similarly, school staff members can have mechanisms established for referring students to community-based domestic violence, sexual assault, depression, and anger management services. Counselors and vocational education faculty can support students in making the transition to adult life and the workforce by ensuring that they are aware of laws governing teenage employment, risks associated with different types of jobs, and strategies to help prevent injuries on the job. Schools have a responsibility to ensure that school-sponsored internships, school-to-work assignments, and other work placements are safe (242,249). Schools might provide counseling or training programs to support youth who feel pressured to undertake dangerous work tasks or who want support in refusing these tasks or getting reassigned. Schools also can help students understand how to access quality physical and mental health services, both as adolescents and adults. A substantial proportion of young adults lack health insurance. Schools could help student learn whether they qualify for programs such as Medicaid or the State Child Health Insurance Program (SCHIP), and how to obtain private insurance through their employers. Identify and Provide Assistance to Students Who Have Been Seriously Injured, Who Have Witnessed Violence, Who Have Been the Victims of Violence or Harassment, and Who Are Being Victimized or Harassed. Students who have been victims of child abuse, dating violence, sexual assault, bullying, harassment, or other forms of violence and those who have observed violence in their families usually need intervention and assistance as well as students who have witnessed violence in their homes, schools, or communities. Survivors of serious unintentional injuries (e.g., a motor- vehicle crash or house fire) are also at increased risk for similar posttraumatic experiences. Schools can have 1) systems established for identifying behavioral changes that point to violence or trauma and 2) explicitly defined protocols for intervention, including referral to community-based resources. For example, teachers and school staff members can be taught to recognize behavioral changes. School psychologists, counselors, and nurses can be aware of community-based resources (e.g., local clinical psychologists and public mental health services) and can refer families to these resources. Not all students who are at increased risk for unintentional injury, violence, and suicide are readily identified. Large schools especially might need to take additional steps to ensure that teachers and school staff members identify special needs of marginalized students. Training and assistance for teachers and school staff members, including school nurses, can help them identify signs of trauma and suicide risk among students, especially among developmentally challenged students, whose responses are often more muted or more difficult to discern. Recent research indicates that students with learning and emotional disabilities and those with mobility impairments are at a substantially increased risk for attempting suicide than their peers (357). Schools can have confidential and nonjudgmental mechanisms in place for students to report when they have been victimized, abused, harassed, or injured by a member of the school community. Schools can identify students at increased risk for engaging in injury-risk behaviors and ensure that they receive targeted prevention programs and services. No easy methods or tools exist for identifying students at increased risk for engaging in unintentional injury or violence risk behaviors. Community, family, and school characteristics (e.g., poverty, domestic violence, and lax school policies) can increase the risk for unintentional injury, violence, and suicide. Students might be considered to be at higher risk for being the victims of violence based on their previous experiences and on characteristics of the communities in which they live (e.g., high rates of dropout, suspension, or expulsion; high levels of calls to police; and neighborhood vandalism). Students who have been bullied, those who have witnessed violence, and those who have been the victims of serious violence are at increased risk for engaging in violence themselves (226,235). Students at risk for school failure and dropout might also be at increased risk for suicide (354). Students who engage in other health risk behaviors (e.g., alcohol and drug use) are at increased risk for engaging in violence and unintentional injury risk behaviors. Students who drive after drinking alcohol or who do not use seat belts also are more likely to carry weapons, engage in physical fights, or consider suicide (136--139). In addition, students who have previously committed acts of violence or attempted suicide are at increased risk for repeating the same behavior in the future (189). Younger students who have been victims of violence are at increased risk for engaging in delinquent and aggressive behaviors in adolescence (60). Gay, lesbian, and bisexual students are at increased risk for attempting suicide (358). Students with special health-care needs are at increased risk for suicide, victimization and unintentional injury (357,359). Schools can implement prevention programs for selected groups of students at higher risk for injury or violence than the general school population (189,190). Resources for identifying such prevention programs are included in this report (Appendix C). Imminent risk for violent or injurious behavior can occur in a smaller group of students (e.g., those returning to school after committing a violent offense or those who have previously attempted suicide) (189). Schools might need to refer these students to community-based prevention and treatment programs. Schools can link students who are at increased risk with school and community services without labeling the students. Schools can work with families, health-care providers, and EMS providers to develop a comprehensive plan and program for those students who are at highest risk for injuries (e.g., students with special health care needs, mental and emotional health problems, or developmental challenges). Schools can link students at increased risk for unintentional injury, violence, and suicide to services addressing a range of health problems. For example, students might need assistance getting eyeglasses or occupational therapy and could be linked to those community services. Students could be linked to health insurance through schools. For students who exhibit behavioral problems or who need tailored interventions, schools might use problem-solving or student assistance teams that can facilitate early identification, intervention, and referral of students to academic, social, or skills-building services (198). Assess the Extent to Which Injuries Occur on School Property. Schools can systematically collect, review, and report on injuries that occur on school property (including school buses) or that are associated with school-sponsored events. To ensure full reporting, methods must not be burdensome to school staff members. Data collection can help schools identify problems, track program effectiveness, and eliminate hazards, thus, potentially reducing liability (218). Data might be collected regarding injuries that occur to students, staff members, and visitors to school property. Some states and school districts have policies requiring that injury data be reported and might also have forms for reporting injury data. Examples of reporting forms are included in the Children's Safety Network at Education Development Center (CSN)(239) and the Utah Department of Health Violence and Injury Prevention Program (360). States, districts, and schools often have different requirements for injury reporting. Staff members can be provided with standardized definitions of injuries that should be recorded and reported. Schools could collect data regarding injuries to students that occur on school property (including school transportation [e.g., school buses]) or at a school-sponsored event. To be more inclusive of injuries, schools might collect information regarding injuries that occur on the way to or from school (not necessarily by school transportation), or on the way to or from a school-sponsored event (not necessarily by school transportation), or those that occur to staff members and visitors to school property. In addition to location, whether injuries are reportable might be determined based on severity (e.g., loss of one half day or more of school) or required medical attention and treatment (i.e., by a school nurse, an athletic trainer, a physician, EMS, an emergency room visit, or hospitalization). Information collected might include
Data can be reviewed to identify patterns and risks for each type of injury. Injury information could be reviewed monthly and a report provided to the school safety committee or school health council (100,218,239). When a data collection system is established, the number of injuries associated with the school might appear to increase temporarily. Typically, this increase is an artifact of better reporting, not an actual increase in incidents. Data are sometimes used to make comparisons among schools, and schools should not be penalized for instituting effective reporting systems. Health services staff members and the school safety committee or school health council can use assessment findings to correct hazards and improve safety in school, thereby potentially protecting students and staff members and reducing liability (360). Develop and Implement Emergency Plans for Assessing, Managing, and Referring Injured Students and Staff Members to Appropriate Levels of Care. In a study of serious injuries to children at school, approximately one out of six children (16%) were sent home rather than sent to receive immediate medical attention, despite the occurrence of injuries that were sometimes serious (e.g., fractures and penetrating wounds) (100). Schools could establish emergency plans for assessing, managing, and referring injured students and staff members to appropriate care (100,218,361). Emergency plans could be developed by school health services staff members and school administrators in collaboration with local emergency medical services (218,266) and could cover potential injuries that might occur throughout the school property and at school-sponsored events off school property. Emergency plans could include provisions for obtaining parental consent for transport in the event that referral for immediate treatment is required. Emergency plans can list health services and other school staff members and their assignments, including at least one qualified person who will assess injured persons and manage immediate care; one person who will call the EMS; persons who will provide control of other students in the area; and one person who will direct community EMS to the location of the injured. This plan is particularly important if health services staff members are not present during all school hours and at school-sponsored events (218,266). To help staff members respond to an injury, emergency plans might include
Emergency plans could be practiced annually, analyzed for effectiveness, and revised as necessary. Resources regarding emergency planning are included in this report (Appendix B). Recommendation 6: Establish Mechanisms for Short- and Long-term Responses to Crises, Disasters, and Injuries That Affect the School Community. Schools need to be responsive to crises and disasters that could affect the school community, including environmental disasters (e.g., fires, floods, tornadoes, blizzards, and earthquakes); death or serious injury of a student or staff member in a car or bus crash, suicide, or a violent event at school; a suicide attempt; terrorism, including bioterrorism; hazardous chemical spills; explosions; radiation; mass illness or injury; or other situations that threaten the safety of persons in the school or community. The school plan can be comprehensive, addressing response needs for multiple types of crises, disasters, and emergencies. Responses should include both short- and long-term services (Box 7). Establish a Written Plan for Responding to Crises, Disasters, and Associated Injuries. Many states require districts and schools to have crisis response plans. Schools should review district and state crisis intervention manuals and adapt them to address local needs. The school plan could include the development of a crisis response team with a designated contact person to coordinate the school's response (362,363). The plan and team could be developed with input from key members of the local community, including school administrators; law enforcement; fire and rescue departments; EMS; mental health agencies; parent-teacher organizations; hospitals; domestic violence shelters; health, social service, and emergency management agencies; rape crisis shelters; the faith community; teachers unions; and organizations such as the Red Cross. Crisis plans can
A communication system could provide for communicating internally as well as for contacting community resources (e.g., law enforcement) and families in the event of an emergency. Schools can communicate basic emergency procedures to families so they will know where to report or call for information in the event of a crisis. A communication system can also include methods for families, community members and agencies, students, and others to communicate potential crises to the school. Floor plans might be shared with local law enforcement, fire and rescue, and EMS agencies (362). Crisis plans can be produced in writing and copies given to all school staff members and all relevant community organizations, even if they do not participate in developing the plan. The plan could be updated annually. Schools can train faculty, staff members, students, and community organization and agency staff members and the crisis response team regarding the crisis response plan and their individual roles and responsibilities in a crisis. Plans should be practiced regularly and whenever updates are incorporated. Prepare to Implement the School's Plan in the Event of a Crisis. Responsiveness during a crisis depends on preparation. In addition to the crisis response plan, schools could have a current list of personnel who are trained and certified to administer first aid and CPR; a phone tree for expediting communication to school staff members and families; clothing or badges to signify members of the crisis response team; fact sheets and letters for distributing information regarding the school to the media; an emergency contact list; and a "go box" (362,363). The go box contains tools and information to be taken to the crisis response post (362) and could include the phone numbers, current lists, and items described previously as well as a bull horn, a complete list of students, and a map and a floor plan, including locations of power and utility connections. A lap top computer and a cell phone or walkie talkie system could also be made available. The contents of the go box might be reviewed and updated at least annually. Several persons should have access to the go box and know how to use it. Resources regarding crisis planning are included in this report (Appendix B). Schools should establish evacuation procedures for moving students to safety, making appropriate provisions for persons with special needs (218). Adequate transportation should be available to move students to the preestablished safe location, taking into account transportation requirements for students with special needs. Reunion areas should be established for students and families to meet each other. Assigned staff members can manage a standardized procedure for releasing students to family members. This procedure could include keeping records of when each student left school grounds and with whom they left. Schools can anticipate demands from the media and be proactive in delivering the information that the school wants released to the media (363). For example, schools can decide in advance what types of information will be released during a crisis and have templates of press releases already assembled. When a crisis occurs, schools can then control the message that will be released to the media. A school official trained in providing information through the media could be designated to speak to the media (365). A specific location for media contacts can be assigned. This location and the name of the media contact can be communicated to local media outlets when releasing the school crisis response plan. In the case of a death by suicide, schools can help media representatives understand that dramatizing the effect of suicide by showing grieving students or memorials might increase the suicide risk for other vulnerable students and community members (366). Have Short-Term Responses and Services Established After a Crisis. Schools should consider reopening as quickly as possible after a crisis has ended. School personnel can be a substantial source of assistance to students. Developmentally appropriate and culturally competent mechanisms are essential for dealing with the psychological consequences of traumatic events in counseling centers, classrooms, and assemblies. Depending on the situation, these mechanisms might involve teachers, administrators, counselors, families, and local safety professionals (e.g., fire fighters after a fire). After a crisis, grief counselors could be made available to students and staff members on both group and individual levels (52,362,363). The school can communicate with students, families, and staff members regarding recognizing and treating posttraumatic stress disorder. Depending on the scope of the crisis, all or some of the students and staff members might not be able to return immediately to routine class schedules. Community resources might need to be sought for counseling and psychological services. A listing of organizations that are resources for contacting trained counselors to assist with debriefing victims and witnesses is included in this report (Appendix B). In the event of a death, students, families, and staff members should be allowed to grieve their losses (363,367). Gatherings or other tributes might be appropriate, except in the case of suicide where public tributes might increase the risk for copycat suicide attempts (367,368). Schools could be proactive in identifying and assisting students who want or need to discuss their feelings. In addition, schools can continue to work with the media so that students and staff members can return to school without disruption and to ensure that the media and the public receive the information they need. Have Long-Term Responses and Services Established After a Crisis. Crises have long-term consequences and should be treated over the long-term. Some students might require ongoing counseling and psychological services (52,363). Schools can anticipate anniversary dates and other occasions that might be painful for members of the school community, which are times when additional services might need to be provided (365). Continue to communicate with students, families and staff members to recognize and treat posttraumatic stress disorder and depression. Schools can teach students coping and grieving strategies they can use throughout their lifetimes. Schools can learn from crises. After a crisis affects the school or community, the school crisis response team might meet to analyze the school's response, consider revisions to the crisis response plan, assess how to prevent future recurrences, and make necessary changes based on lessons learned (218). Recommendation 7: Integrate School, Family, and Community Efforts to Prevent Unintentional Injuries, Violence, and Suicide. Schools cannot prevent unintentional injuries, violence, and suicide in isolation from the communities and families they serve. Schools, communities, and families can provide each other with reciprocal benefits (369). Teachers and law enforcement officials believe that a lack of family involvement in school is a major contributor to school violence (370). When parents are involved in school, violent and antisocial behavior decreases (369). Family members can be invited to participate in all areas of education; and unintentional injury, violence, and suicide prevention training could be offered to families. Schools might invite community representatives to participate regularly in the school safety committee or school health council (220). Community agencies and organizations can use their resources to support extracurricular programming to prevent unintentional injuries, violence, and suicide (198). A broad range of public health, mental health, social service, and public safety agencies; and youth-serving organizations could be encouraged to provide services and education in the school (Box 8). Involve Parents, Students, and Other Family Members in All Aspects of School Life, Including Planning and Implementing Unintentional Injury, Violence, and Suicide-Prevention Programs and Policies. Family members can be encouraged to participate in all aspects of school life (214,215,238,305,369). Responsible adult supervision is essential for safety in the school, on school playgrounds, and for other school activities (e.g., field trips and school-to-work assignments) (369). Volunteer assistance can be useful for the majority of schools that are working to improve the safety of their playgrounds. Family members could be active participants on the school safety committee and on problem-solving teams (305,369). Family members could advocate for quality schools that are safe and provide a range of services necessary for healthy development. Involving families in school might strengthen connections between students and their families. Schools can support and encourage communication and collaboration between family members and school personnel. Many mechanisms (e.g., electronic mail, Internet sites, voice mail, newsletters, cable television, and teacher/parent conferences) are available to improve family member involvement in education. These mechanisms can work to facilitate two-way communication (305,369). Families can be encouraged to make school personnel aware of life-changing events that affect their children (e.g., divorce and death). Family-based education strategies (e.g., homework assignments that involve family participation) also can increase communication and collaboration between family members and school personnel (223,369). Family members are role models, and students who have positive adult role models are less likely to engage in bullying behaviors (371). Family members can serve as mentors for their children and others. They can supervise their children and pay attention to their behavior. They can model healthy relationships within their families and with others they meet in the community. Family members can teach students that aggressive and violent behaviors are not tolerated and that respect and tolerance for others are expected. Educate, Support, and Involve Family Members in Child and Adolescent Unintentional Injury, Violence, and Suicide Prevention. Various methods can be used to reach out to family members. Regular family seminars, newsletters, local access television, public television, Internet sites, religious organizations, and other community organization activities could be useful to engage and educate families. Students also can educate their families regarding safe behaviors they learn in school (e.g., the importance of using seat belts) (245). Schools can teach family members about
Schools can help families secure the assistance they need to prevent unintentional injuries, violence, and suicide by
Coordinate School and Community Services. To build partnerships between school and community, schools could make school facilities available for extracurricular activities, community-sponsored leagues and community events (e.g., sports leagues and community service group meetings). Community-based injury-prevention programs and organizations (e.g., Mothers Against Drunk Driving (MADD) and Boys and Girls Clubs of America) could be provided access to school facilities on afternoons, evenings, weekends, and during school breaks. Schools can increase availability of supervised after-school activities and programs (216,373,374). After-school hours are peak times for violence and crime. Adolescents are at the highest risk for being victims of crime and violence in the 4 hours after the end of the school day (375). Many elementary school students as well as adolescents are home alone after school. The majority of these students exhibit anxiety, fears concerning staying home alone, loneliness, and boredom (324). Young adolescents who spend a substantial amount of time without adults are more likely to engage in bullying behavior (371). Unsupervised children are at an increased risk for both unintentional injury (324) and involvement in violence and crime (373,375). After-school activities could be supervised, developmentally appropriate, and follow the same recommendations for safety addressed throughout this document. Schools can work with local government and community organizations to promote safer schools, workplaces, and communities through policies, programs, and services (198,305). Students, parents, and staff members might be encouraged to support and participate in community efforts to prevent unintentional injury, violence, and suicide. Students can carry out service projects in their communities (e.g., graffiti removal, planting gardens, and volunteering in a nursing home or day care center) (181). Involvement in service learning activities can prevent violence and delinquency (376). Schools can help community organizations and agencies involve families in educational and other activities designed to reduce unintentional injury, violence, and suicide (e.g., to encourage home fire drill planning and practice, to restrict unsupervised access to alcohol, drugs, and firearms for children and adolescents, to educate community members concerning handguns in the home, and to establish safe walking and bicycling paths) (216). Schools can also participate in communitywide coalitions addressing unintentional injury, violence, and suicide prevention. Recommendation 8: For All School Personnel, Provide Regular Staff Development Opportunities That Impart the Knowledge, Skills, and Confidence to Effectively Promote Safety and Prevent Unintentional Injury, Violence, and Suicide, and Support Students in Their Efforts to Do the Same. Trained staff members are essential to implementing a coordinated school program to prevent unintentional injury, violence, and suicide. Staff members who understand how to prevent unintentional injury, violence, and suicide for students and for themselves can transmit this information to students. Staff members who act to prevent unintentional injuries, violence, and suicide for themselves and others can be positive role models for students (Box 9). Ensure That Staff Members are Knowledgeable About Unintentional Injury, Violence, and Suicide Prevention and Have the Skills Needed to Prevent Injuries and Violence at School, at Home, and in the Community. Preservice education regarding unintentional injury, violence, and suicide prevention for school administrators, faculty, and staff members could be strengthened (217). Preservice education could integrate concepts and methods of unintentional injury, violence, and suicide prevention (e.g., environmental change, and conflict resolution) into academic subject areas, especially health education. Specifically, preservice education might include information and skill-building regarding the causes, epidemiology, and prevention of unintentional injury, violence, and suicide. Faculty could receive professional staff development on developing and maintaining safe learning environments. Effective educational techniques for creating safe learning environments include proactive classroom management techniques, cooperative learning methods, social skills training, promoting interactive learning, and environmental modification (201,213,214,320,330). Staff development in behavior management and effective teaching might be provided to teachers with high rates of office referral, or to teachers who have experienced high rates of behavioral problems in the classroom (198). Injury-prevention training for faculty could include identification and elimination of injury hazards, use of safety gear and safety rules, identification of students at risk for suicide and violence, child abuse reporting requirements, conflict resolution techniques, first aid and CPR, and methods for teaching injury-prevention skills to students (100). Schools might provide incentives (e.g., continuing education credits) for participating in staff development opportunities. Faculty could receive staff development whenever new or revised unintentional injury, violence, or suicide-prevention curricula, policies, or equipment are introduced (217). Trained teachers are more likely to implement programs and more likely to affect student outcomes than untrained teachers (377--379). Schools can provide program-specific training, including the underlying theoretical and conceptual framework for the program. Training could address both the content and teaching strategies for behavior change but focus on the latter. Program activities could be modeled and teachers provided with opportunities to practice. All school staff members might receive some staff development on unintentional injury, violence, and suicide prevention. School staff members other than faculty can also play an important role in preventing unintentional injury, violence, and suicide. Bus drivers, security personnel, grounds and custodial staff members, and others might be provided with training on unintentional injury, violence, and suicide prevention and first aid and CPR (198). Staff members could be trained to identify and respond to students who might be considering suicide (277,282,295) and to students who might be victims of physical or sexual abuse (380). Other skills could include proper use of protective gear, knowledge and implementation of safety rules and prevention procedures, emergency first aid and CPR, sexual-harassment prevention, methods for responding to observed bullying, and use of nonviolent conflict resolution methods. Schools can work with local mental health, public health, and other professionals to develop training, backup, and formal mechanisms for referral (282). Schools can encourage collaboration across disciplines and between faculty and other school staff members. For example, teachers could know whom to contact for assistance when a student reports that they are being abused; bus drivers could have a mechanism for reporting bullying behavior, weapons, or alcohol and drug use on the school bus; and teachers and nurses could refer students at increased risk for suicide to counselors. Train and Support All Personnel to Be Positive Role Models for a Healthy and Safe Lifestyle. Adults in the school can role model prosocial and safe behaviors (245) (e.g., coaches can treat students respectfully; teachers can intervene when they observe student-to-student harassment; custodial staff members can model safe use and storage of caustic chemicals; bus drivers can wear seat belts; and industrial arts teachers can use eye protection and other safety equipment). All school staff members, including grounds and custodial staff members, bus drivers, administrators, faculty, and other staff members could be trained and supported in their efforts to model safety and respect. Schools can support positive role modeling by providing health promotion programs that include unintentional injury, violence, and suicide prevention and first aid and CPR education for staff members. Schools also could encourage staff members to use community programs (e.g., programs designed to reduce stress and strengthen coping mechanisms). In addition, schools can provide staff members information concerning programs and other resources available in the community and monitor the use of school and community programs and resources. CONCLUSIONSTo ensure a safe and healthy future for students in the United States, school-based unintentional injury, violence, and suicide-prevention programs should become a national priority. These programs could be part of coordinated school health programs and reach students from preschool through secondary school. School leaders, community leaders, and families can commit to implementing and sustaining unintentional injury, violence, and suicide prevention within the schools. Such support is crucial to promoting safety and a healthy academic environment. The eight recommendations for school-based unintentional injury, violence, and suicide prevention presented in this report provide the framework for establishing such schoolwide strategies. By adopting these recommendations, schools can help ensure that all school-aged youth attain their maximum educational potential and good health. The resources listed in Appendices B and C, and the additional tools being developed by CDC and others, can assist schools in reaching this goal. References
Table 1 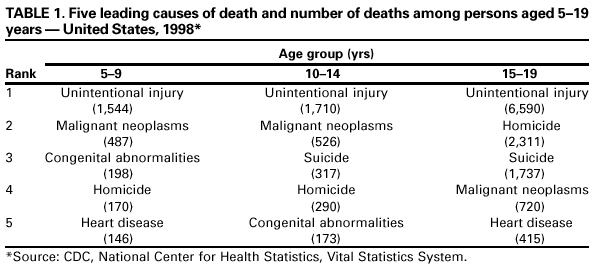 Return to top. Box 1 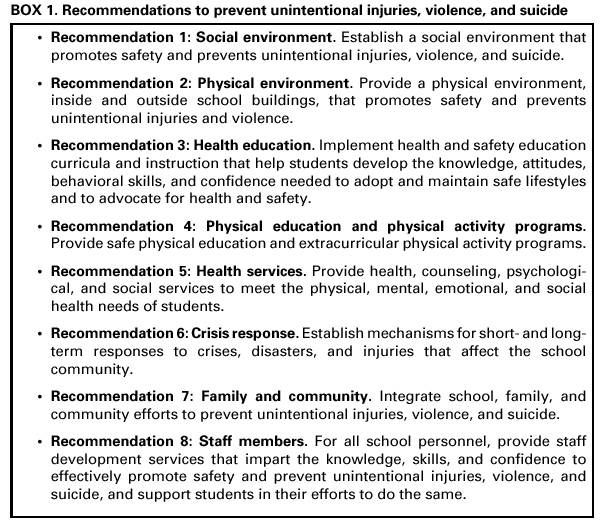 Return to top. Table 2 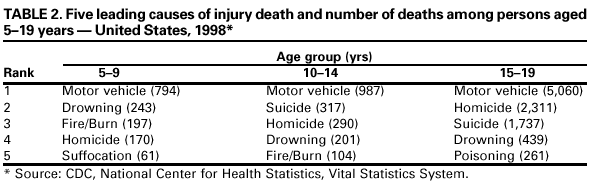 Return to top. Box 2 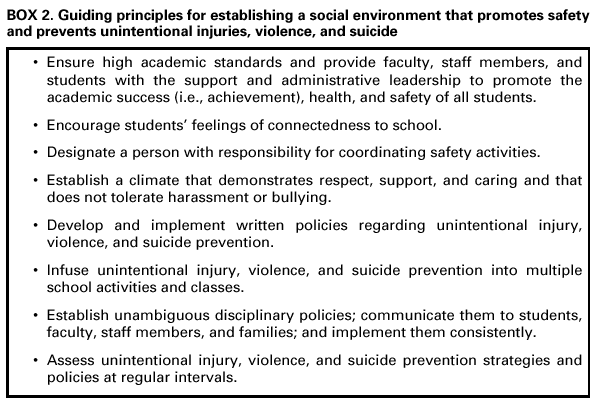 Return to top. Box 3 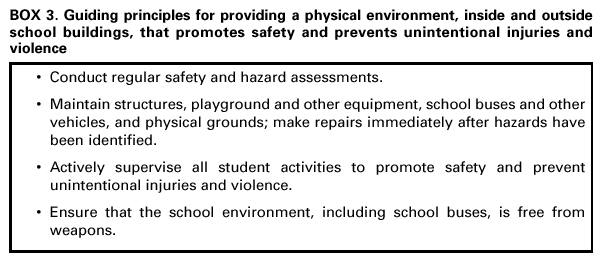 Return to top. Box 4  Return to top. Box 5 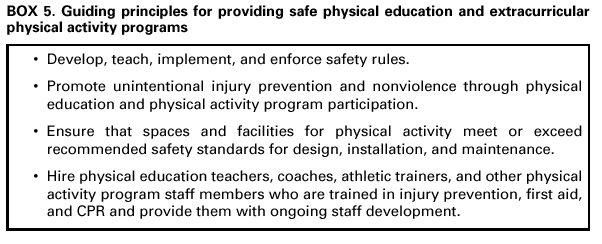 Return to top. Box 6 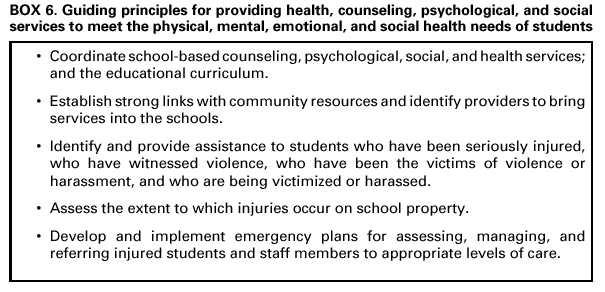 Return to top. Box 7  Return to top. Box 8  Return to top. Box 9  Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 12/4/2001 |
|||||||||
This page last reviewed 12/4/2001
|