 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Informatics and Public Health at CDCScott J. N. McNabb, PhD,1 D. Koo,
MD,2 R. Pinner, MD,3 J. Seligman,
MS4
Corresponding author: Scott J. N. McNabb, PhD, Division of Integrated Surveillance Systems and Services, National Center for Public Health Informatics, CDC, 2500 Century Parkway, MS E-91, Atlanta, GA 30345. Telephone: 404-498-6427; Fax: 404-498-6144; E-mail: smcnabb@cdc.gov. Since CDC acquired its first mainframe computer in 1964, the use of information technology in public health practice has grown steadily and, during the past 2 decades, dramatically (Table 1). Public health informatics (PHI) arrived on the scene during the 1990s after medical informatics (intersecting information technology, medicine, and health care) and bioinformatics (intersecting mathematics, statistics, computer science, and molecular biology). Similarly, PHI merged the disciplines of information science and computer science to public health practice, research, and learning (2--5). Using strategies and standards, practitioners employ PHI tools and training to maximize health impacts at local, state, and national levels. They develop and deploy information technology solutions that provide accurate, timely, and secure information to guide public health action. Early PHI ApplicationsAdvances in PHI resulted in public health innovations and added value to interventions by providing the capability for more timely detection of health threats and more complete and efficient health communications. Early PHI initiatives at CDC assisted the collection and analysis of data. Epi Info™ showed that combining questionnaire development with data base creation and specialized analytic tools gave greater facility during surveillance and outbreak investigations (6,7). When Internet use became common, the CDC PHI initiatives linked users and incorporated integrative and open-networked architecture. In this new, integrated environment, CDC PHI initiatives shifted to serve the broader public health community through development of enterprise architecture, standards, systems, and interoperability. Evolving from the Enhanced Surveillance Project in four states, the National Electronic Telecommunications System for Surveillance (NETSS) began in 1990 (8). NETSS (which supports the National Notifiable Diseases Surveillance System) provided a standard record and variables for reporting all individual cases of disease, without requiring a specific software solution. Early on, NETSS data were communicated by dial-up modem each week from state health departments to CDC. This improved the timeliness of public health surveillance. In 1990, CDC released the Wide-ranging OnLine Data for Epidemiologic Research (WONDER) (9,10). This tool provided access to data on the CDC mainframe for analyses by CDC epidemiologists. WONDER/PC---released to the broader public health community in 1992---included access to e-mail for practitioners from local and state health departments, private bulletin boards, and searchable CDC document libraries plus the capability to download data in CDC surveillance programs while maintaining data security and patient confidentiality. PHI CrossroadsBy the early 1990s, CDC and its partners recognized both the costliness of systems specific to categorical diseases and health conditions and the capability of the Internet to permit more efficient approaches to data collection and analyses. In 1993, CDC launched a plan with partners to conceive and develop integrated surveillance (11). Furthermore, in 1993, the Information Network for Public Health Officials (INPHO) initiative began to enhance broader access to CDC information technology, networking, and software systems by users (12,13). These initiatives marked a PHI milestone for CDC: movement from stand-alone solutions for individual problems to networked, integrated solutions and standards-based data exchange. Six current CDC PHI initiatives reflect this vision and highlight the critical role of PHI in transforming public health practice: PulseNet USA (14); the National Electronic Disease Surveillance System (NEDSS) (15); the Epidemic Information Exchange (Epi-X); the Health Alert Network (HAN) (16,17); BioSense (18); and the Public Health Information Network (PHIN) (19). In 1993, a large outbreak of foodborne illness occurred in the western United States (20). Laboratory scientists performed DNA "fingerprinting" and determined the strain of Escherichia coli O157:H7 found in patients had the same pattern as that found in hamburger patties served at a large chain of regional fast-food restaurants. Prompt recognition of this outbreak and its cause might have prevented as many as 800 illnesses. As a result, CDC created PulseNet USA, the molecular surveillance network for foodborne infections in the United States and an indispensable tool for early detection of foodborne disease outbreaks (14). In 1999, CDC launched NEDSS. With the goal of integrating public health surveillance through case reporting of approximately 100 diseases using a standards-based data interchange, NEDSS enabled new electronic data feeds from clinical laboratories and substantially reduced the latency of data transmission, improved completeness of reporting, and decreased data-reporting burdens (15). Created in 2000, Epi-X is the CDC secure communications solution for practitioners to access and share information. Recently, an epidemiologist in Colorado noted an unusual bacterial infection, Burkholderia cepacia, in patients who had sinus surgery. This information was posted on Epi-X. After further investigation, a common epidemiologic link was found: the use of a particular nasal spray of the same lot, made by the same company. Epi-X's notice informed officials that this lot most likely was contaminated, and through this alert, the Food and Drug Administration and the company intervened to recall that lot of nasal spray. Also launched in 2000, HAN was developed to improve public health interconnectivity through a statewide and a national alert system. In response to the increased threat of bioterrorism, in 2003, CDC launched BioSense to improve the nation's capabilities for real-time biosurveillance and situational awareness. BioSense maintains patient confidentiality and uses secure methods to receive health data from sources such as hospitals and health-care systems in major metropolitan areas. BioSense connects existing health information to public health and will enable simultaneous access to data analytic and visualization tools by authorized users at all jurisdictional levels. Balanced with secure protection from misuse, CDC's vision for interoperable and integrated networking is embodied in PHIN. Initiated in 2004, PHIN promotes standards and, in some cases, software solutions to enable real-time data flow, computer-assisted analyses, decision support, professional collaboration, and rapid dissemination of information (Box). These PHI initiatives and others reflect CDC's ongoing commitment to make evidence-based decisions and maximize health impacts. They support PHI tools that will effectively monitor the health of communities, identify causes of disease, and provide the tracking and management capabilities necessary to respond to and contain outbreaks. They also help evaluate the performance and measure the costs of health information systems (21). Furthermore, they connect public health systems to clinical-care systems (e.g., electronic medical records). PHI Training at CDCAlthough a workforce trained in PHI is essential, the supply of informaticians is not sufficient to meet national needs (17). To address this, CDC initiated a 2-year PHI fellowship program in 1996, which has graduated 51 fellows. These fellows have contributed to standards development, enabled agencywide knowledge management, and performed research. During the responses to hurricanes Katrina and Rita in 2005, three PHI fellows deployed to Texas and Louisiana to support integration of surveillance and develop electronic-based surveillance tools, and two were assigned to the CDC Director's Emergency Operations Center to manage surveillance data. CDC recently initiated a plan to define competencies for public health informaticians. The Future of PHIRecognizing the growing importance of PHI across the agency, CDC created the National Center for Public Health Informatics (NCPHI) in 2005 to provide leadership and coordination of shared systems and services. NCPHI's mission is to protect and improve the public's health through PHI discovery, innovation, and service. NCPHI is developing a national PHI research agenda and advancing the state-of-the-science through a grant program with academic institutions and state and local health departments. NCPHI has funded five Centers of Excellence in PHI and has awarded additional research grants to support the BioSense program to further the science of early detection and analyses. Collectively, these projects reflect CDC's ongoing efforts to build and support a national network of integrated, standards-based, and interoperable public health information systems that will enhance its partners' capabilities to detect, register, confirm, report, analyze, provide feedback and alerts, and communicate to drive evidence-based decisions that make health impacts. One challenge now facing PHI is to facilitate the development of electronic medical and personal health records that both protect patient privacy and confidentiality and serve legitimate clinical and public health needs. With U.S. health-care costs steadily rising---now representing approximately 16% of the gross domestic product---and the increase of acute and chronic health threats, PHI must help meet these challenges through more efficient and effective disease prevention (e.g., better detection, communication, public health action, and health protection). These benefits, combined with the increasing expectation of (and requirements for) instantaneous access to public health data, make the potential contribution of PHI to public health practice even more promising and urgent. PHI is now positioned to accelerate, building from the substantial increase in information technology invested in health care and capitalizing on major trends toward electronic medical and personal health records. Future PHI systems will include innovative solutions extending the reach of public health practice to more efficiently and effectively impact health. Acknowledgments The authors thank the following persons---listed in alphabetic order---for their contribution to this article: Andrew Autry, PhD; Claire Broome, MD; Scott Danos, MPH; Sigrid Economou; Robert Fagan; Lynn Gibbs Scharf, MPH; Mary Lerchen, DrPh; Timothy Morris; Tony Moulton, PhD; Dale Nordenberg, MD; Joseph Reid, PhD; Barry Rhodes, PhD; Henry Rolka, MS; David Ross, ScD; Thomas Savel, MD; Jerome Tokars, MD; Herman Tolentino, MD; and John Ward, MD. References
Table 1  Return to top. Box 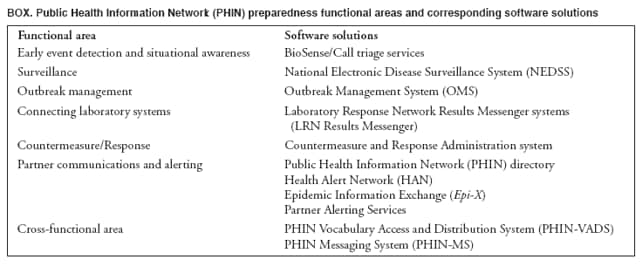 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Date last reviewed: 12/18/2006 |
|||||||||
|