 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Self-Reported Asthma Prevalence Among Adults ---United States, 2000Asthma is a chronic inflammatory disorder of the airways characterized by episodes of wheezing, shortness of breath, chest tightness, and cough and is among the most common chronic diseases in the United States, affecting approximately 10.2 million adults during 1996 (1). Direct and indirect costs associated with asthma during 1998 were an estimated $12.7 billion (2). Despite the prevalence and associated costs of asthma, state-specific data have not been available (3,4). This report summarizes state asthma prevalence data collected from the 2000 Behavioral Risk Factor Surveillance System (BRFSS) survey, which indicated that approximately 7.2% of adults residing in the United States reported having asthma. This is the first state-specific asthma prevalence data available for all 50 states. Continued use of the BRFSS asthma questions will allow state health departments to monitor trends in asthma prevalence and to provide data to direct asthma management. BRFSS is a state-based, random-digit--dialed survey of the noninstitutionalized U.S. population aged >18 years; the survey collects information about modifiable risk factors for chronic diseases and other leading causes of death (5). CDC and state and territorial departments of health use the system to monitor trends that affect public health decisions. During 1999, the first optional two-item module on asthma was added to the BRFSS questionnaire. During 2000, the asthma questions were used in the 50 states, Puerto Rico, and the District of Columbia. Two asthma case definitions were constructed. Lifetime asthma was defined as answering "yes" to "Have you ever been told by a doctor that you have asthma?" Current asthma was defined as answering "yes" to "Have you ever been told by a doctor that you have asthma?" and "Do you still have asthma?" Weighted prevalence estimates and 95% confidence intervals were calculated using SUDAAN to account for the complex survey design (6). The median response rate was 51.3% (from 33.4% in New Jersey to 75.5% in Minnesota). On the basis of answers from 182,293 respondents, the overall prevalence of lifetime asthma was 10.5%. The median rate of lifetime asthma from the 52 reporting areas was also 10.5% (from 8.0% in Louisiana to 15.9% in Puerto Rico) (Table 1). During 2000, an estimated 14.6 million adults had current asthma; the overall prevalence of current asthma was 7.2%. The median rate of current asthma from the 52 reporting areas was 7.3% (from 5.0% in Louisiana to 8.9% in Maine) (Table 1). Current asthma was higher among blacks (8.5%) than whites (7.1%) and persons of other race/ethnicity (5.6%). The prevalence of current asthma decreased with increasing family income (from 9.8% among persons with family incomes of <$15,000 to 5.9% among persons with family incomes of >$75,000). Women had higher rates of current asthma than men both overall (9.1% versus 5.1%) and in each reporting area (Table 2). Reported by the following BRFSS coordinators: S Reese, Alabama; P Owen, Alaska; R Weyant, Arizona; B Woodson, Arkansas; B Davis, California; M Leff, Colorado; M Adams, Connecticut; F Breukelman, Delaware; I Bullo, District of Columbia; S Oba, Florida; L Martin, Georgia; F Reyes-Salvail, Hawaii; J Aydelotte, Idaho; B Steiner, Illinois; L Stemnock, Indiana; J Davila, Iowa; C Hunt, Kansas; T Sparks, Kentucky; B Bates, Louisiana; D Maines, Maine; A Weinstein, Maryland; D Brook, Massachusetts; H McGee, Michigan; N Salem, Minnesota; D Johnson, Mississippi; J Jackson, Missouri; P Feigley, Montana; L Andelt, Nebraska; E DeJan, Nevada; J Taylor, New Hampshire; G Boeselager, New Jersey; W Honey, New Mexico; C Baker, New York; Z Gizlice, North Carolina; L Shireley, North Dakota; P Coss, Ohio; K Baker, Oklahoma; K Pickle, Oregon; L Mann, Pennsylvania; Y Cintron, Puerto Rico; J Hesser, Rhode Island; M Wu, South Carolina; M Gildemaster, South Dakota; D Ridings, Tennessee; K Condon, Texas; K Marti, Utah; C Roe, Vermont; J Hicks, Virginia; K Wynkoop-Simmons, Washington; F King, West Virginia; K Pearson, Wisconsin; M Futa, Wyoming. Air Pollution and Respiratory Health Br, Div of Environmental Hazards and Health Effects, National Center for Environmental Health; and an EIS Officer, CDC. Editorial Note:This report provides the first estimates of self-reported asthma in U.S. adults collected and reported at the state level. Previous state estimates were calculated using National Health Interview Survey regional data and demographic data from the states. In 1998, national prevalence of current asthma among adults and children was 6.4% (from 5.8% in Florida, Oklahoma, and West Virginia to 7.2% in Nevada) (7). BRFSS data indicate no consistent regional pattern and some variability among the states. Possible reasons for this variability include demographic, socioeconomic (e.g., income and education levels) and environmental factors (e.g., outdoor air pollution and climate), physician diagnostic procedures, or response rates. Asthma rates consistently were higher among women than men. Higher rates among women have been described for both prevalence and other measures of asthma (e.g., hospitalization and mortality) (3) and may be associated with hormones, obesity, or other factors (8,9). It is unclear whether variability in rates reflects a true difference in prevalence, differences in reporting, or other factors. The findings in this report are subject to at least three limitations. First, the median response rate for the survey was only 51.3%. Second, BRFSS does not measure asthma prevalence in institutionalized adults, persons aged <18 years, and residents without telephones; the percentage of households with telephones ranges from 87% (Mississippi) to 98% (Massachusetts) (6). Third, the validity of self-reported asthma status in BRFSS is unknown. BRFSS case definitions include respondents who have been told by a physician that they have asthma; either the physician's diagnosis or the subjects' recall of that diagnosis may be inaccurate. A 1998 review of asthma questionnaires reported a mean sensitivity of 68% (range: 48%--100%) and a mean specificity of 94% (range: 78%--100%) when self-reported asthma was compared with a clinical diagnosis of asthma (10). The continued use of the BRFSS asthma questions will allow state health departments to monitor trends in asthma prevalence and to provide data to direct asthma management. In addition, the data will provide state-specific information on asthma prevalence by age, race/ethnicity, education level, and family income. References*
*All MMWR references are available on the Internet at <http://www.cdc.gov/mmwr>. Use the search function to find specific articles. Table 1  Return to top. Table 2 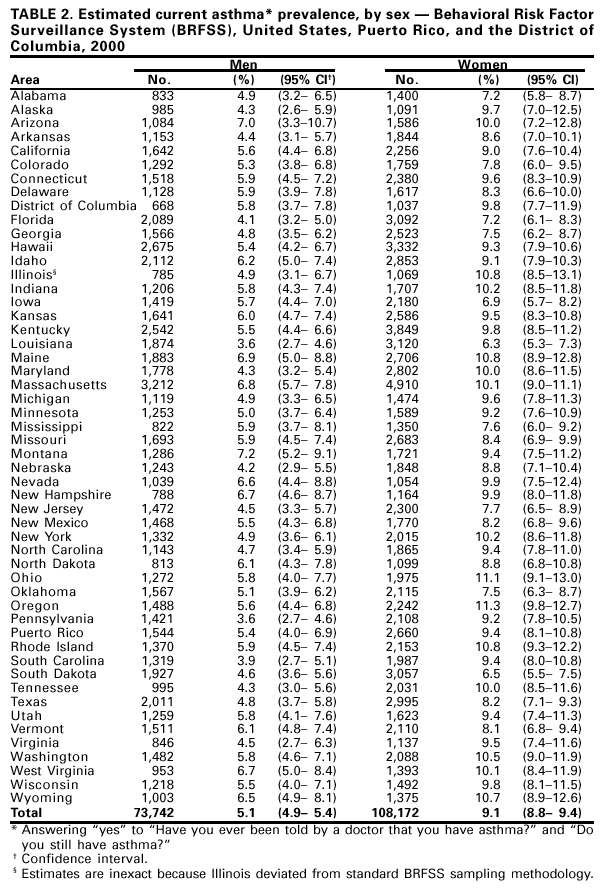 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 8/24/2001 |
|||||||||
This page last reviewed 8/24/2001
|