 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Global Youth Tobacco Surveillance, 2000--2007Charles W. Warren, PhD,1 Nathan R. Jones,
PhD,1 Armando Peruga, MD,2 James Chauvin,
MSc,3
Jean-Pierre Baptiste, PhD,4 Vera Costa de Silva,
MD,5 Fatimah el Awa, PhD,6 Agis Tsouros,
PhD,7
Khalil Rahman, PhD,8 Burke Fishburn,
MPP,9 Douglas W. Bettcher,
MD,2 Samira Asma, DDS1
Corresponding author: Charles W. Warren, PhD, Office on Smoking and Health, National Center for Chronic Disease Prevention and Health Promotion, 4770 Buford Highway, N.E., MS K-50, Atlanta, GA 30341; Telephone: 770-488-5739; Fax: 770-488-5939; E-mail: wcw1@cdc.gov. AbstractProblem: Tobacco use is a major contributor to deaths from chronic diseases. The findings from the Global Youth Tobacco Survey (GYTS) suggest that the estimate of a doubling of deaths from smoking (from 5 million per year to approximately 10 million per year by 2020) might be an underestimate because of the increase in smoking among young girls compared with adult females, the high susceptibility of smoking among never smokers, high levels of exposure to secondhand smoke, and protobacco indirect advertising. Reporting Period Covered: This report includes GYTS data collected during 2000--2007 from 140 World Health Organization (WHO) member states, six territories (American Samoa, British Virgin Islands, Guam, Montserrat, Puerto Rico, and the U.S. Virgin Islands), two geographic regions (Gaza Strip and West Bank), one United Nations administered province (Kosovo), one special administrative region (Macau), and one Commonwealth (Northern Mariana Islands). For countries that have repeated GYTS, only the most recent data are included. For countries with multiple survey sites, only data from the capital or largest city are presented. Description of System: GYTS is a school-based survey of a defined geographic site that can be a country, a province, a city, or any other geographic entity. GYTS uses a standardized methodology for constructing sampling frames, selecting schools and classes, preparing questionnaires, conducting field procedures, and processing data. GYTS standard sampling methodology uses a two-stage cluster sample design that produces samples of students in grades associated with students aged 13--15 years. Each sampling frame includes all schools (usually public and private) in a geographically defined area containing any of the identified grades. In the first stage, the probability of schools being selected is proportional to the number of students enrolled in the specified grades. In the second sampling stage, classes within the selected schools are selected randomly. All students in selected classes attending school the day the survey is administered are eligible to participate. Student participation is voluntary and anonymous using self-administered data collection procedures. The GYTS sample design produces independent, cross-sectional estimates that are representative of each site. Results: The findings in this report indicate that the level of cigarette smoking between boys and girls is similar in many sites; the prevalence of cigarette smoking and use of other tobacco products is similar; and susceptibility to initiate smoking among never smokers is similar among boys and girls and is higher than cigarette smoking in the majority of sites. Approximately half of the students reported that they were exposed to secondhand smoke in public places during the week preceding the survey. Approximately eight in 10 favor a ban on smoking in public places. Approximately two in 10 students own an object with a cigarette brand logo on it, and one in 10 students have been offered free cigarettes by a tobacco company representative. Approximately seven in 10 students who smoke reported that they wanted to stop smoking. Approximately seven in 10 students who smoked were not refused purchase of cigarettes from a store during the month preceding the survey. Finally, approximately six in 10 students reported having been taught in school about the harmful effects of smoking during the year preceding the survey. Interpretation: The findings in this report suggest that interventions that decrease tobacco use among youth (e.g., increasing excise taxes, media campaigns, school programs in conjunction with community interventions, and community interventions that decrease minors' access to tobacco) must be broad-based, focused on boys and girls, and have components directed toward prevention and cessation. If effective programs are not developed and implemented soon, future morbidity and mortality attributed to tobacco probably will increase. Public Health Action: The synergy between countries in passing tobacco-control laws, regulations, or decrees; ratifying the WHO Framework Convention on Tobacco Control; and conducting GYTS offers a unique opportunity to develop, implement, and evaluate comprehensive tobacco-control policy that can be helpful to each country. The challenge for each country is to develop, implement, and evaluate a tobacco-control program and make changes where necessary. IntroductionTobacco use is one of the major preventable causes of premature death and disease in the world (1). A disproportionate share of the global tobacco burden falls on developing countries, where 84% of 1.3 billion current smokers reside (1). The World Health Organization (WHO) attributes approximately 5 million deaths a year to tobacco. The number is expected to exceed 10 million deaths by 2020, with approximately 70% of these deaths occurring in developing countries (2). In July 1998, WHO established the Tobacco Free Initiative (TFI) to focus international attention, resources, and action on the global tobacco epidemic. One of the primary objectives of TFI was to promote ratification of the WHO Framework Convention on Tobacco Control (WHO FCTC), the first international public health treaty on tobacco control (3). The treaty urges countries to develop action plans for public policies (e.g., banning direct and indirect tobacco advertising, instituting tobacco tax and price increases, promoting smoke-free public places and workplaces, and placing health messages on tobacco packaging). WHO FCTC was initiated on February 27, 2005, and 149 countries were parties to the treaty as of August 2007. In addition to WHO FCTC, certain WHO Regional Offices have developed and implemented regional tobacco-control action plans (4--9). All of these efforts in tobacco control recognize the need for countries to establish surveillance efforts as stated in the WHO FCTC Article 20: The Parties shall establish, as appropriate, programmes for national, regional and global surveillance of the magnitude, patterns, determinants, and consequences of tobacco consumption and exposure to tobacco smoke. Towards this end, the Parties should integrate tobacco surveillance programmes into national, regional and global health surveillance programmes so that data are comparable and can be analysed at the regional and international levels, as appropriate (3). In December 1998, WHO, CDC, and the Canadian Public Health Association (CPHA) developed the Global Tobacco Surveillance System (GTSS) to assist countries in establishing tobacco-control surveillance and monitoring programs (10,11). GTSS includes collection of data through four surveys: the Global Youth Tobacco Survey (GYTS) for youth, the Global School Personnel Survey, the Global Health Professions Student Survey, and the Global Adult Tobacco Survey for adults. This report focuses on data from GYTS, which countries use to enhance their capacity to monitor tobacco use among youth; guide national tobacco prevention and control programs; and facilitate comparison of tobacco-related data at the national, regional, and global levels. In 9 years, GYTS has achieved broad global coverage, especially in low- and middle-income countries where few surveillance activities had been conducted. Since 1999, GYTS has been conducted in 140 countries and 11 territories and across all six WHO regions. Participating countries are repeating the survey every 4--5 years (Appendix A). GYTS follows the standard public health definition of surveillance (12) and has become the most comprehensive youth tobacco surveillance system ever developed, implemented, and maintained. MethodsGYTS is a school-based survey of a defined geographic site that can be a country, a province, a city, or any other geographic entity. GYTS uses a standardized methodology for constructing sampling frames, selecting schools and classes, preparing questionnaires, conducting field procedures, and processing data. The survey includes questions on tobacco use, knowledge and attitudes regarding tobacco, secondhand smoke (SHS) exposure, pro- and antitobacco media and advertising exposure, desire for cessation, access and availability to obtain tobacco products, and having been taught in school about the harmful effects of tobacco use. Sample DesignWithin each country, the scope of GYTS is defined through consultation among the country GYTS research coordinator, WHO TFI regional advisors, and CDC technical advisors. Depending on data requirements of the country, resources available, and safety concerns, the scope of GYTS can be national, regional, or focused on specific urban or rural areas. In addition, certain samples are designed to yield information that is representative of country geographic regions but can be pooled to yield nationally representative estimates. After the sampling frames are defined, the GYTS research coordinator provides CDC with school enrollment information, and the samples are drawn using a standard protocol and software developed by CDC. GYTS standard sampling methodology uses a two-stage cluster sample design that produces samples of students in grades associated with students aged 13--15 years. Each sampling frame includes all schools (usually public and private) in a geographically defined area containing any of the identified grades. At the first stage, the probability of schools being selected is proportional to the number of students enrolled in the specified grades. At the second sampling stage, classes within the selected schools are randomly selected. All enrolled students in selected classes the day the survey is administered are eligible to participate. Student participation is voluntary and anonymous using self-administered data collection procedures. The GYTS sample design produces representative, independent, cross-sectional estimates for each sampling frame. Data AnalysisA weighting factor is applied to each student record to adjust for nonresponse (by school, class, and student) and variation in the probability of selection at the school and class levels. A final adjustment sums the weights by grade and sex to the population of school children in the selected grades in each sample site. The weighting factor consisted of the following formula: W = W1 * W2 * f1 * f2 * f3 * f4 where W1 = the inverse of the probability of selection for each school. W2 = the inverse of the probability of selection of each classroom within each selected school. f1 = a school level, nonresponse adjustment calculated by school enrollment size category (small, medium, or large); school nonresponse is calculated within each tertile. f2 = a class level, nonresponse adjustment factor calculated for each school. f3 = a student level, nonresponse adjustment factor calculated by class. f4 = a poststratification adjustment factor calculated by sex and grade. SUDAAN, a software package for statistical analysis of correlated data, was used to calculate weighted prevalence estimates and standard errors (SE) of the estimates (95% confidence intervals [CI] were calculated from SEs) (13). Differences in proportions are considered statistically significant at the p<0.05 level. QuestionnaireThe core 2007 GYTS questionnaire includes 54 questions covering seven categories: tobacco use, knowledge and attitudes regarding tobacco, SHS exposure, pro- and antitobacco media and advertising exposure, desire for cessation, access and availability to obtain tobacco, and having been taught in school about the harmful effects of tobacco use (Appendix B). To maintain maximum comparability across countries that conduct GYTS, research coordinators are discouraged from altering core questions. Changes to the core are accepted for content that is not relevant to the country. Research coordinators are encouraged to develop and add questions to the core questionnaire to gather information important to their country or WHO region. The final country questionnaires are translated into local languages as needed and back-translated to check for accuracy. GYTS country research coordinators conduct focus groups of students aged 13--15 years to further test the accuracy of the translation and student comprehension of the questions. This report includes the following key indicators related to prevalence of tobacco use among adolescents and components of comprehensive tobacco-control programs: current cigarette smoking, current use of tobacco products other than cigarettes, and susceptibility of never smokers to smoking initiation (14). In addition, several factors that influence tobacco use are reported, including exposure to SHS, exposure to indirect protobacco advertising, desire to stop smoking, access to tobacco products, and teaching about the dangers of tobacco use in school (Table 1). CoverageIn 1999, a total of 12 countries successfully pilot-tested GYTS (Barbados, China, Costa Rica, Fiji, Jordan, Poland, Russian Federation, South Africa, Sri Lanka, Ukraine, Venezuela, and Zimbabwe) representing each of the six WHO regions. WHO regions include the African Region (AFR), Region of the Americas (AMR), Eastern Mediterranean Region (EMR), European Region (EUR), South-East Asia Region (SEAR), and Western Pacific Region (WPR). Following the initial success, GYTS expanded rapidly among WHO member states in all regions, territories, and other geographic regions. GYTS has been completed in 140 WHO member states, six territories (American Samoa, U.S. Virgin Islands, British Virgin Islands, Guam, Montserrat, and Puerto Rico), two geographic regions (Gaza Strip and West Bank), one United Nations administered province (Kosovo), one special administrative region (Macau), and one commonwealth (Northern Mariana Islands) (Table 2). GYTS has been repeated in 66 countries; by the end of 2008, a total of 48 other countries will conduct repeat surveys, and 26 new countries will complete their initial GYTS. Repeat surveys have been conducted in 4- or 5-year intervals. For the 66 countries that have repeated GYTS, only the most recent data are included in this report (Appendix C) and, for countries with multiple survey sites that cannot be pooled into a national estimate, only data from the capital or largest city are presented. For this report, the 140 WHO member states and 11 other populations will be referred to as "sites." The GYTS data in this report include 29 member states in AFR (19 national and 10 subnational); 34 member states and four territories in AMR (25 national and 13 subnational); 21 member states and two geographic regions in EMR (17 national and six subnational); 28 member states and one United Nations administered province in EUR (28 national and one subnational); 10 member states in SEAR (eight national and two subnational), and 18 member states, two territories, one special administrative region, and one commonwealth in WPR (19 national and three subnational). The school response rate is calculated as the number of participating schools divided by the number of selected schools. The class response rate is calculated as the number of participating classes divided by the number of selected classes. The student response rate is calculated as the number of participating students divided by the number of students enrolled in the class. The overall response rate is calculated as the product of the school response rate, the class response rate, and the student response rate. Of the 151 sites, five had school response rates below 80%; 84 had 100% school response rates (Table 3). Of the 151 sites, four had class response rates lower than 100%. The student response rate was <80% in 17 sites (with a low of 53.2% in Samoa); the overall response rate was >80% in 119 sites and <60% in eight sites. ResultsPrevalenceOverall, 9.5% of students currently smoked cigarettes. The rate was highest in EUR (19.2%) and lowest in EMR (4.9%) (Table 4). Approximately 15% of students smoked cigarettes in four of the 29 sites in AFR, 13 of the 38 sites in AMR, one of the 23 sites in EMR, 15 of the 29 sites in EUR, one of the 10 sites in SEAR, and 13 of the 22 sites in WPR. Current cigarette smoking was >30% in Bulgaria, Chile (Santiago), Colombia (Bogota), Cook Islands, Czech Republic, East Timor, Latvia, and Papua New Guinea. Boys were significantly more likely than girls to smoke cigarettes in AFR, EMR, SEAR, and WPR; no significant differences were observed by sex in AMR and EUR. Of the 151 sites, no sex differences were observed in 87 sites, boys were significantly more likely than girls to smoke cigarettes in 59 sites, and girls were significantly more likely than boys to smoke in five sites. One in 10 (10.1%) students currently used tobacco products other than cigarettes (e.g., pipes, water pipes, smokeless tobacco, and bidis), with the rate highest in EMR (12.0%) and lowest in WPR (6.6%) (Table 4). Approximately 15% of students used other tobacco products in five of the 28 sites in AFR, none of the 38 sites in AMR, six of the 23 sites in EMR, one of the 29 sites in EUR, one of the 10 sites in SEAR, and six of the 19 sites in WPR. Current use of other tobacco products was >30% in Latvia, Lebanon, Micronesia, and the Northern Mariana Islands. Boys were significantly more likely than girls to use other tobacco products overall and in AMR, EUR, and SEAR; no significant differences were reported by sex in the other regions. Of the 147 sites where data could be reported, no sex differences were reported in 98 sites, boys were significantly more likely than girls to use other tobacco products in 49 sites, and in no site were girls significantly more likely than boys to use other tobacco products. Among students who had never smoked cigarettes, 19.1% indicated they were susceptible to initiate smoking during the next year. The rate was highest in EUR (29.8%) and lowest in WPR (13.4%) (Table 4). Approximately 15% of students reported they were susceptible to initiating smoking in the next year in 12 of the 29 sites in AFR, 26 of the 38 sites in AMR, 13 of the 22 sites in EMR, 22 of the 24 sites in EUR, three of the nine sites in SEAR, and 14 of the 22 sites in WPR. No significant differences were reported by sex in any region. Of the 144 sites where data could be reported, no sex differences in susceptibility were reported in 122 sites, boys were significantly more likely than girls in 16 sites, and girls were significantly more likely than boys in six sites. Cigarette smoking was significantly higher than other tobacco use in AMR, EUR, and WPR; other tobacco use was significantly higher than cigarette smoking in EMR and SEAR; and no differences in AFR or overall were reported across all sites. Susceptibility was significantly higher than current cigarette smoking overall and in every region except WPR, where no difference was reported. Factors Influencing Tobacco UseExposure to Secondhand Smoke Overall, approximately four in 10 students (42.5%) were exposed to smoke in their home during the week preceding the survey (Table 5). Among the six regions, exposure to SHS at home was highest in EUR (77.8%) and lowest in AFR (27.6%). In the other four regions, exposure to SHS at home ranged from 50.6% (WPR) to 34.3% (SEAR). Approximately half of the students were exposed to SHS at home in one of the 29 sites in AFR, five of 38 sites in AMR, five of 23 sites in EMR, 27 of 29 sites in EUR, four of 10 sites in SEAR, and 13 of 22 sites in WPR. Approximately half (55.1%) of all students were exposed to SHS in public places during the week preceding the survey (Table 5). Exposure to SHS in public places was highest in EUR (86.1%). For the other five regions, exposure to SHS in public places ranged from 64.1% (WPR) to 43.7% (AFR). Across all regions, approximately 50% of students were exposed to SHS in public places in 13 of the 29 sites in AFR, 25 of 38 sites in AMR, six of 23 sites in EMR, all 29 sites in EUR, seven of 10 sites in SEAR, and 18 of 21 sites in WPR. More than three fourths (78.3%) of students in all regions thought smoking should be banned in all public places (Table 5). Six in 10 students (58.9%) in AFR thought smoking should be banned in public places, compared with more than seven in 10 students in SEAR (77.5%) and more than eight in 10 students in the other four regions. Approximately 80% of students support smoke-free public places in seven of 29 sites in AFR, 18 of 35 sites in AMR, 13 of 23 sites in EMR, 17 of 29 sites in EUR, six of 10 sites in SEAR, and seven of 16 sites in WPR. Indirect Pro-Tobacco Advertising Overall, 14.9% of students owned an object with a cigarette brand logo on it. The rate was highest in AFR and EUR (18.0% and 17.8%, respectively) and lowest in SEAR (9.2%) (Table 5). Across all regions, approximately 20% of students owned an object with a cigarette brand logo on it in 11 of 28 sites in AFR, two of 38 sites in AMR, three of 23 sites in EMR, 13 of 29 sites in EUR, two of 9 sites in SEAR, and six of 18 sites in WPR. Overall, one in 10 students (10.0%) had been offered free cigarettes by a tobacco company representative. The rate was highest in AFR (12.2%) and lowest in WPR (8.0%) (Table 5). Across all regions, approximately 15% of students had been offered free cigarettes by a tobacco company representative in three of 27 sites in AFR, two of 35 sites in AMR, two of 23 sites in EMR, five of 29 sites in EUR, three of 10 sites in SEAR, and one of 16 sites in WPR. Cessation Overall, 68.7% of students who currently smoke cigarettes reported that they desired to stop smoking (Table 6). The desire to stop smoking was highest in WPR (80.7%) and lowest in AMR (53.3%). Across all regions, approximately 80% of students who currently smoked desired to stop smoking in eight of 21 sites in AFR, three of 30 sites in AMR, two of 17 sites in EMR, one of 28 sites in EUR, two of 8 sites in SEAR, and 11 of 19 sites in WPR. Access and Availability Overall, five in 10 (46.7%) students who currently smoke cigarettes usually purchased their cigarettes in stores (Table 6). The rate was highest in EUR (61.7%) and lowest in AMR (20.2%). Across all regions, approximately 50% of students who currently smoke cigarettes usually bought their cigarettes in a store in three of 25 sites in AFR, nine of 35 sites in AMR, one of 20 sites in EMR, 20 of 28 sites in EUR, five of eight sites in SEAR, and four of 19 sites in WPR. Seven in 10 (70.5%) students who bought cigarettes in a store were not refused purchase of cigarettes during the month preceding the survey because of their age (Table 6). The rate was lowest in WPR (47.9%) and approximately 70% in EUR, EMR, and AMR. Across all regions, approximately 75% who smoked were not refused purchase of cigarettes from a store during the month preceding the survey because of their age in three of 13 sites in AFR, 16 of 21 sites in AMR, nine of 12 sites in EMR, 20 of 27 sites in EUR, three of seven sites in SEAR, and two of 10 sites in WPR. School Curriculum Overall, more than half of the students (57.6%) reported having been taught in school about the dangers of tobacco during the preceding school year (Table 6). The rate was highest in WPR (68.8%) and lowest in EMR (47.5%). Across all regions, approximately 60% of students had been taught about the dangers of tobacco in seven of 29 sites in AFR, eight of 38 sites in AMR, three of 23 sites in EMR, 15 of 28 sites in EUR, four of 10 sites in SEAR, and 12 of 21 sites in WPR. DiscussionThis report includes tobacco surveillance data from 151 sites. Despite variation among individual sites and WHO regions in students' tobacco use prevalence and factors associated with tobacco use, several patterns emerge that have substantial implications for global tobacco control. Within the 151 sites, no difference was observed in smoking prevalence between boys and girls in 87 sites; boys had higher rates than girls in 59 sites, and girls had higher rates than boys in five sites. Other reports have indicated that the prevalence of cigarette smoking among girls aged 13--15 years in GYTS exceeds that of adult females in 60 of the 117 countries where comparisons can be made (15). Furthermore, the proportion of never smokers susceptible to initiating smoking is similar among boys and girls in 122 sites and is higher than current cigarette smoking in all regions except WPR. These findings suggest that cigarette smoking is high among girls compared with rates observed among adult females in other studies. Two reasons have been identified in support of this contention (16--17). First, for decades the tobacco industry has targeted females and continues to expand this market (18--19). The tobacco industry targets women through advertisements showing smoking associated with independence, stylishness, weight control, sophistication, and power (20). In addition, sex-neutral brands such as Marlboro are marketed to women using independent and fun-loving imagery. Second, although smoking rates among adult females might be low compared with adult males, millions of women smoke. This might be contributing to a change in cultural traditions and social influences, making smoking among women and young girls more acceptable (21). The findings in this report also indicate that efforts are needed to reduce the impact of the factors that have the most influence on tobacco use among adolescents. Approximately half of the students reported they were exposed to SHS in public places during the week preceding the survey, although approximately eight in 10 favor a ban on smoking in public places. Approximately two in 10 students own an object with a cigarette brand logo on it, and one in 10 students have been offered free cigarettes by a tobacco company representative. Despite extensive marketing by the tobacco industry, approximately seven in 10 students who currently smoked reported that they wanted to stop smoking. Although some countries have laws or regulations banning the sale of tobacco products to adolescents, GYTS results indicate that approximately seven in 10 students who smoked were not refused purchase from a store. Finally, only six in 10 students reported learning about the harmful effects of smoking in school during the year preceding the survey. On February 27, 2005, WHO FCTC was initiated, and parties to the treaty agreed to strong obligations to improve tobacco control. The 149 countries that have ratified WHO FCTC are required to enact comprehensive legislation to restrict advertising, require a higher standard of health warnings on product packaging, reduce SHS exposure by prohibiting smoking in public places, raise tobacco taxes to increase prices, reduce cigarette smuggling, and diversify agriculture away from tobacco (3). To support WHO FCTC, WHO regional offices are developing tobacco-control action plans to provide clear strategies to countries for reducing and controlling tobacco use (4--9). These efforts call on countries to develop, implement, and enforce comprehensive tobacco-control programs to improve the health of the population by encouraging smokers to quit, eliminating exposure to SHS, and discouraging nonsmokers from initiating tobacco use. Comprehensive tobacco-control programs generally include public education campaigns to counteract tobacco advertising, community-based programs to reduce tobacco use, cessation-assistance programs, school-based programs, enforcement of existing tobacco restrictions, monitoring and evaluation of the control program, and related policy efforts to support the program (e.g., increased excise taxes, chronic disease programs targeting tobacco-related health problems, and environmental tobacco smoke restrictions) (1,22,23). Data from GYTS can provide countries with valuable feedback to monitor and evaluate tobacco-control action plans and to develop plans where none exist. WHO FCTC and GYTS are part of the same goal of developing, implementing, and evaluating effective tobacco-control programs. WHO FCTC contributes to the strengthening of tobacco control in countries, both in terms of public health advocacy and with respect to collaboration between governmental and nongovernmental agencies. GYTS measures certain factors that WHO FCTC asks countries to monitor among youth (Table 7) and provides indicators to measure progress towards achieving seven WHO FCTC articles. WHO FCTC calls for countries to use consistent methods and procedures in their surveillance efforts. GYTS provides a globally implemented and consistent framework for conducting surveillance, including standard sampling procedures, core questionnaire items, training in field procedures, and analysis of data consistent across all GYTS sites. GYTS also enhances the role of the nongovernmental sector by supporting participation by civil society agencies in surveillance, monitoring, and policy and program development. LimitationsThe findings in this report are subject to at least four limitations. First, because GYTS is limited to students, the survey is not representative of all youths aged 13--15 years from participating countries. However, in the majority of countries, the majority of persons in this age group attend regular, private, or technical schools (24). Second, these data apply only to youths who were in school on the day of the survey and who completed the survey. However, student response rates were high (146 of the 151 sites had student response rates of >80%), suggesting that bias attributable to absence or nonresponse was limited. Third, GYTS has not been completed in countries in Western Europe, Canada, Australia, Japan, and certain central African countries. Seventeen central African countries plan to implement GYTS in 2008. Finally, data were based on the self-report of students, who might underreport or overreport their behaviors or attitudes. The extent of this bias cannot be determined from these data; however, reliability studies in the United States have indicated good test-retest results for similar tobacco-related questions (25). Although GYTS has achieved broad geographic coverage in a short time, future expansion of GYTS should focus on two goals. First, countries that have not conducted GYTS should be encouraged to implement the survey. AFR and EUR are planning to expand GYTS in 2008 to include 21 new countries. Second, countries that have completed subnational surveys should be encouraged to expand coverage to the national level. ConclusionThe findings in this report suggest that interventions that decrease tobacco use among youth (e.g., increasing excise taxes, media campaigns, school programs in conjunction with community interventions, and community interventions that decrease minors' access to tobacco) must be broad-based, focused on boys and girls, and have components directed toward prevention and cessation. If effective programs are not developed and implemented soon, future morbidity and mortality attributed to tobacco probably will increase. WHO FCTC, WHO regional tobacco-control action plans, and country tobacco-control action plans provide useful frameworks for implementing such a comprehensive approach. The synergy between countries passing tobacco control laws, regulations or decrees; ratifying and complying WHO FCTC; and conducting GYTS offers a unique opportunity to develop, implement and evaluate comprehensive tobacco control policy that can be helpful to each country. References
GYTS Regional Coordinators WHO Regional Offices: African Region, Nivo Ramanandraibe; Region of the Americas, Kerstin Schotte; South-East Asia Region, Dhirendra N. Sinha; Western Pacific Region, Jonathan Santos. African Region: Djamel Zoughailech (Algeria); Filomena Wilson (Angola); Victor Hounkonnou (Benin); Tebogo Maule, Tuduetso Ramokate, Eprhaim Rapalai (Botswana); Larda Theodore Kangoye, Mathias Some, Drabo Maxime, Vitalien Kpdoa, Arouna Ouedraogo (Burkina Faso); Ahmed Ouledi (Comoros); Rosalie Liki-Bobo (Congo); Aka Michel Yessoh, Pascal Bogui (Cote d'Ivoire); Asgodom Mosazghi (Eritrea); Sefanit Mengistu Gebreab, Abdurahman Abdo (Ethiopia); Edith Wellington, S.O. Sackey (Ghana); Joyce Nato, Ezra Ouma Ogwell (Kenya); Itumelleng Kimane, Maletela Tuoane, Makholu Lebaka (Lesotho); Patrick Kanyimbo, Adamson Muula, John Kapito, Esther Chaswa (Malawi); Maitre Mahamane Ibrahima Cisse, Diarra Nazoum (Mali); Elhadj Diop (Mauritania); Deowan Mohee (Mauritius); Augusto Nunes (Mozambique); Taimi Amaambo, Elizabeth Indongo, Stanley Sinvula Mugambwa (Namibia); Daga Magagi (Niger); Ima-Obong Ekanem (Nigeria); Frida Mokiti (Republic of Tanzania); Cheikh Ibrahima Niang, Samba Cor Sarr (Senegal); Bharathi Viswanathan, Pascal Bovet (Seychelles); Dehran Swart, Fred Koopman (South Africa); Africa Magongo, David Pritchard, Sydney Nkambule (Swaziland); Osseni Tidjani, Abdou Gbadamassi (Togo); Lillian Mpabulungi, Frederick Musoke (Uganda); Richard Zulu, Mbiko Msoni (Zambia); Pepukai Chikukwa, Christopher Zishiri, Edwin G.V. Sithole, Shungu Munyati (Zimbabwe). Region of the Americas: Colin O'Keiffe, Joan A. Moses (Antigua & Barbuda); Hugo A. Miguez (Argentina); Judith Scavella, Larrie Williams (Bahamas); Elaine M. King, Peter Wickham, Sean Daniel, Ruchelle Roach (Barbados); Kimani Avila (Belize); Franklin Alcaraz del Castillo (Bolivia); Luisa Goldfarb, Valeska Caralho Figueiredo, Adelemara Mattoso Allonzi, Leticia Casado Costa, Liz Maria de Almeida (Brazil); Ivy George, Sheila L. Samiel (British Virgin Islands); Luis Caris, Claudia Gonzalez Wedmaier (Chile); Carlos Jose Castro, Carolina Weisner, Constanza Parda Ramos, Raul Murillo (Colombia); Julio Bejarano (Costa Rica); Lucia Lances Cotilla (Cuba); Joan Henry (Dominica); Raquel Pimentel (Dominican Republic); Silvia Corella Ramirez, Patricio Jacome (Ecuador); Carmen Elena Moreno (El Salvador); Alister Antoine (Grenada); Mirna Gracia, Irma Perez, Miguel Garces, Ana Garces (Guatemala); Shradhanand Haviprashad (Guyana); Gilbert Jean Charles, Gerald Lerebours (Haiti); Maria Gertrudis (Honduras); Karen Prendergast, Ellen Grizzle (Jamaica); Raydel Valdes Salgado, Blanca Villa-Contreras, Jesus Felipe Gonzalez Roldan, Luz Myriam Reynales Shigematsu (Mexico); Almae O'Garro (Montserrat); Marcos Membreno Idiaquez, Silvia Narvaez Flores (Nicaragua); Reina Roa (Panama); Graciela Gamarra (Paraguay); Alfonso Zavaleta (Peru); Milagros Sanchez (Puerto Rico); Petronella Edwards (Saint Kitts & Nevis); Elvina Lawrence, Cyprian Lande (Saint Lucia); Patsy Wyllie (Saint Vincent and the Grenadines); Gerold Vliet, Kris Rambali, M. Mangroo (Suriname); Leo Alleyne, Nicole Cooper (Trinidad & Tobago); Julia Sheen-Aaron (U.S. Virgin Islands); Raquel Magri, Gabriela Olivera (Uruguay); Ricardo Granero, Ligia de Pinto (Venezuela). Eastern Mediterranean Region: Sayed Ali Shah Alawie (Afghanistan); Salah Ali Abdulrahman, Khadem Al-Halwaji, Maha El Mokhla (Bahrain); Samira Ali Higo, Abdulrahman Mohamed Abubaker (Djibouti); Nevein Moneir Dous, Samy Ghanem, Mohamed Mehrez Mostafa (Egypt); Samah Eriqat, Salah Shaker Isa Soubani, Moein Al Kariry (Gaza Strip and West Bank); Ahmed Ali Bahaj, Ali Asghar Farshad, Hassan Azaripour Masooleh (Iran); Dilyara Barzani, Sarhang Jalal (Iraq); Heba Ayoub, Imam Al Jaghbeer (Jordan); Sami Al Nasser (Kuwait); Georges Saade, Nagib Ghosn (Lebanon); Mohamed Salah, Ahmed Buni, Mohamed Salah (Libya); Sanaa Cherqaoui, Noureddine Chaouki, Abdelkhalek Moujarrade (Morocco); Sahar Abdou Helmy, Issa Al-Shuaili, Jawad Al-Lawati, Salah Al Muzahmi (Oman); Shahzad Alan Khan, Muhammad Yaqoob Qureshi (Pakistan); Ahmad Moh'd Almulla, Ahmed Al-Ibrahim, Hamda Qotba (Qatar); Abdullah Mohamed Al Bedah, Abdulla Mohamed Al Rabeah (Saudi Arabia); Ali Sheikh Omar, Muse Yusuf Shirwae, Ali Sheikh Omaer Kabil, Mohamed Said Mohamed (Somalia); Ibrahim Abdelmageed Mohamed Ginawi, Ilham Abdalla Bashir (Sudan); Bassam Abu Al Zahab (Syria); Mohamed Nabil Ben Sahem, Alya Mahjoub Zarrouk, Mohamed Mokdad, Mongi Hamrouni (Tunisia); Bassam Abi Saab, Hala Haidar, Ayesha Al-Mutawa (United Arab Emirates); Ahmed Ali-Bahaj, Mohammed Al Khawlani (Yemen). European Region: Roland Shuperka (Albania); Alexander Bazarjyan (Armenia); Irina Zastenskaya (Belarus); Antoaneta Manolova (Bulgaria); Tanja Coric, Dijana Mayer (Croatia); Ourania Kolokotroni, Elpidoforos Soteriades (Cyprus); Hana Sovinova (Czech Republic); Kadi Lepp, Krystiine Liiv (Estonia); Aida Ramic-Catak, Zivana Gavric (Bosnia & Herzegovina); Elena Kosevska (FYR Macedonia); Nana Nikolaishvili, Akaki Gamkrelidze (Georgia); Elpidoforos Soteriades (Greece); Agnes Nemeth, Judit Kiss (Hungary); Kazbek Tulebaev, Alma Zhylkaidarova (Kazakhstan); Ivana Jovanovic, Naser Ramadani (United Nations administered province of Kosovo); Aisha Tokobaeva (Kyrgyzstan); Iveta Pudule (Latvia); Antanas Gostautas (Lithuania); Agima Ljaljevic (Montenegro); Krzysztof Przewoznjak (Poland); Vorfolomei Calmic (Republic of Moldova); Libija Dimitrijevic-Tanskovic, Djordje Stojilkovic, Andjelka Dzeletovic (Republic of Serbia); Ileana Mirestean (Romania); Elena Skvortsova, Konstantine Vitalievich Vyshinsky, Irina Parfenova, Andrei Demine (Russian Federation); Tibor Baska (Slovakia); Mojca Juricic (Slovenia); Zulfiya Nisanbaeva (Tajikistan); Toker Erguder, Mesut Yildirim (Turkey); Konstantin Krasovsky, Nadezhda Polka, Tatiana Andreeva (Ukraine). South-East Asia Region: Zulfiqar Ali (Bangladesh); Sonam Phuntsho (Bhutan); Nunik Kusumawardani (East Timor); Dhirendra Sinha, Prakash Gupta, Urmi Sen, Surendra Shastri, Vendhan Gajalakshmi, Monika Arora, Mira Aghi, Rameshwar Sharma, M. Prakasamma, G. Gururaj, Arun Chaturvedi, Sanjeev Misra, Mihir Shah, Rajesh Dixit, R. Thulasidasan, and S.K. Jindal (India); Tjandra Yoga Aditama (Indonesia); Ahmed Waheed, Maimoona Aboobakar (Maldives); Nyo Nyo Kyaing (Myanmar); M. R. Pandey (Nepal); P. W. Gunasekera (Sri Lanka); Nithat Sirichotiratana (Thailand). Western Pacific Region: Sivia Sunia (American Samoa); Sin Sovann, Sung Vin Tak (Cambodia); Jiangping Sun, Jiang Yuan (China); Edwina Tangaroa (Cook Islands); Brenda Hadley Epenam, Mary Ann Eperiam (Federated States of Micronesia); Ilisapeci Movono, Mosese Salusalu (Fiji); Francis Victor Epres, Joleen Almandres (Guam); Sun Ha Jee (Korea); Khattanaphone Phandouangsy, Anothay Kongsayasak, Ketkeo Boupha, Khampone Insixiengmay (Laos); Chan Tan Mui (Macao SAR); Manimaran Krishnan (Malaysia); Dondog Jargalsaikhan, L. Erdenebayar, Palam Enkhtuya, Tsogzolmaa Bayandorj (Mongolia); Andrew Morehu Waa (New Zealand); Isamu Abraham (Northern Mariana Islands); Valerie Whipps, Andrew Tabelual, Sylvia Matinag Andres (Palau); Jessica Yaipupu, James Wangi (Papua New Guinea); Marina Miguel-Baquilod (Philippines); Nancy MacDonald, Herbert Peters, Taumafaimolealilii Poleka (Samoa); Chng Chee Yeong, Foo Ling Li, Kaven Cheong, Lam Sian Lian (Singapore); Teimana Avanitele (Tuvalu); Winch Garae (Vanuatu); Phan Thi Hai (Viet Nam). CDC Support: Juliette Lee, Veronica Lea, Melissa Lewis. Research Triangle Institute Support: Donn Smith, Mathew Bensen.
Table 1 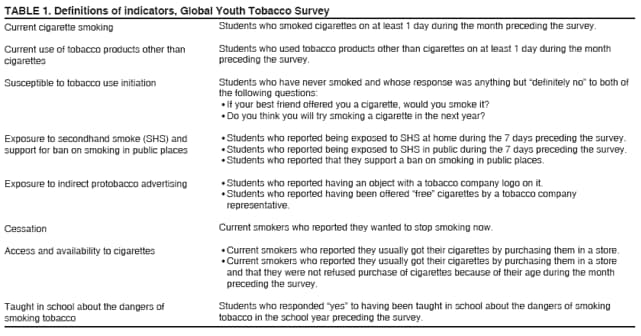 Return to top. Table 2  Return to top. Table 3 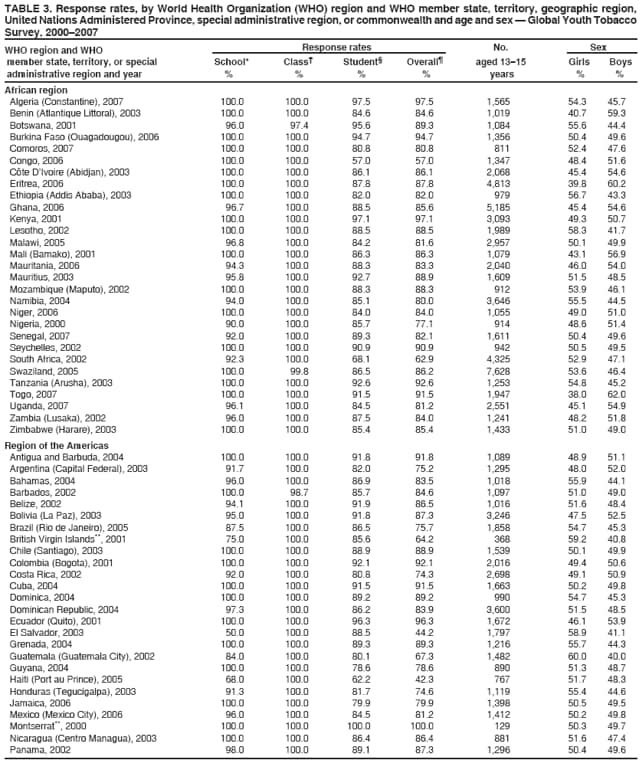 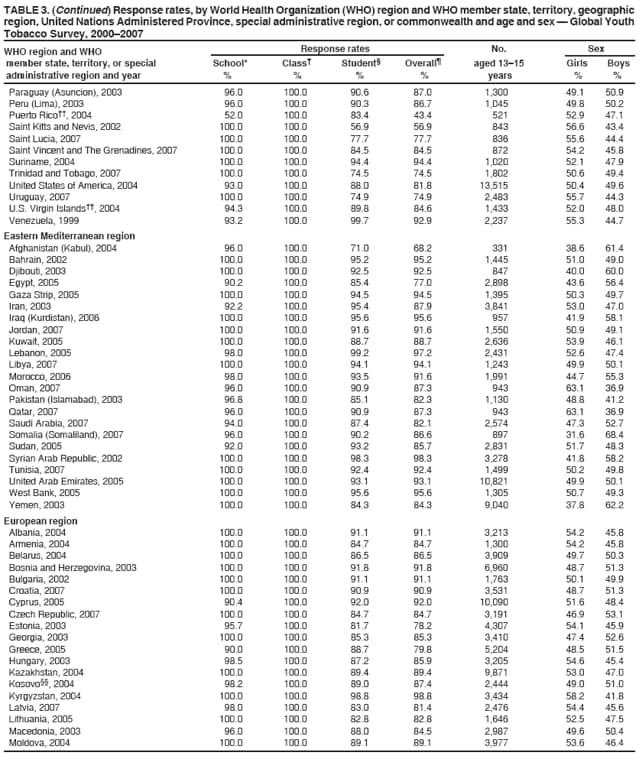  Return to top. Table 4 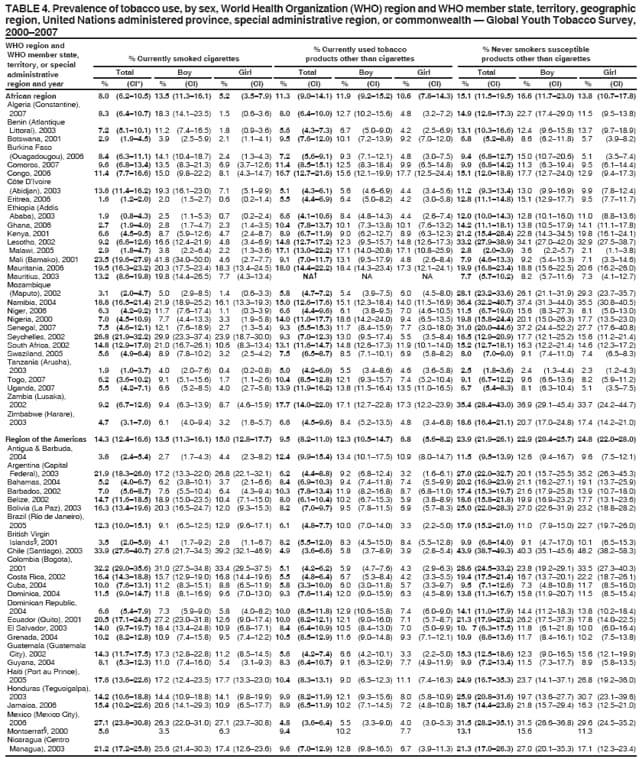 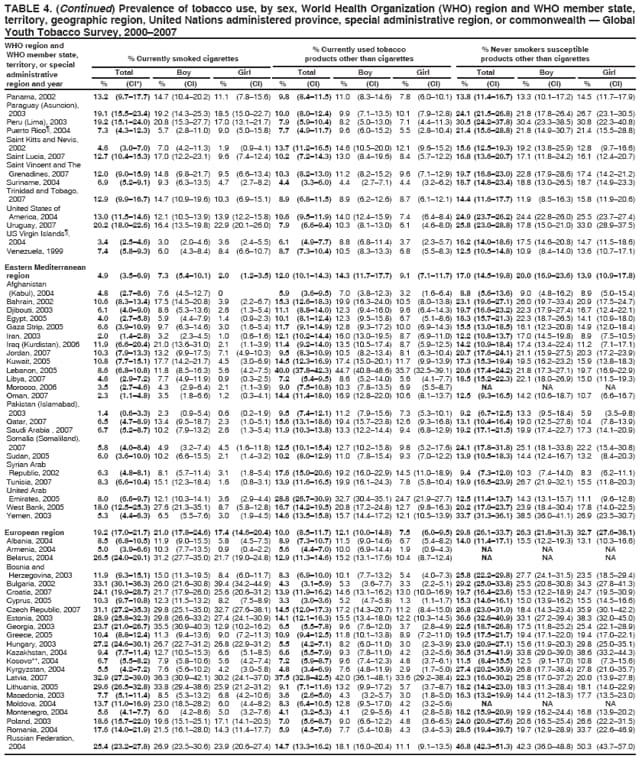 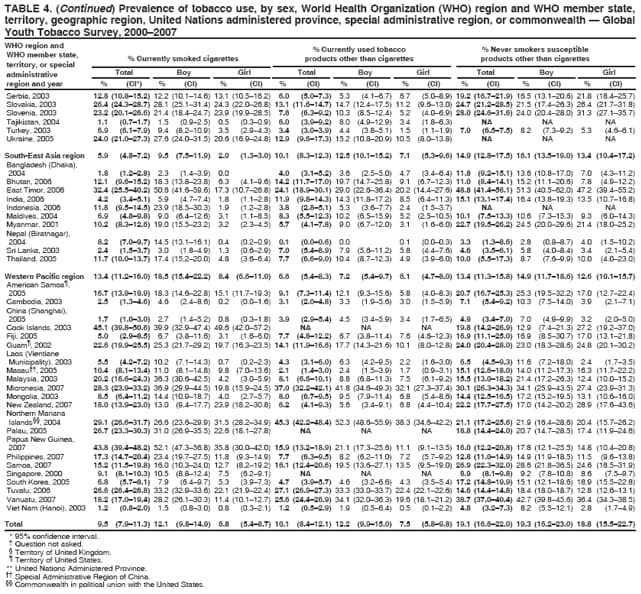 Return to top. Table 5 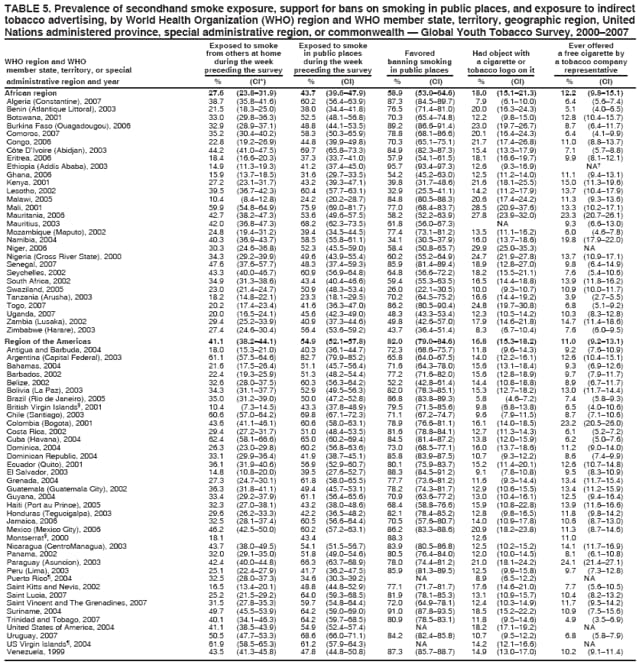 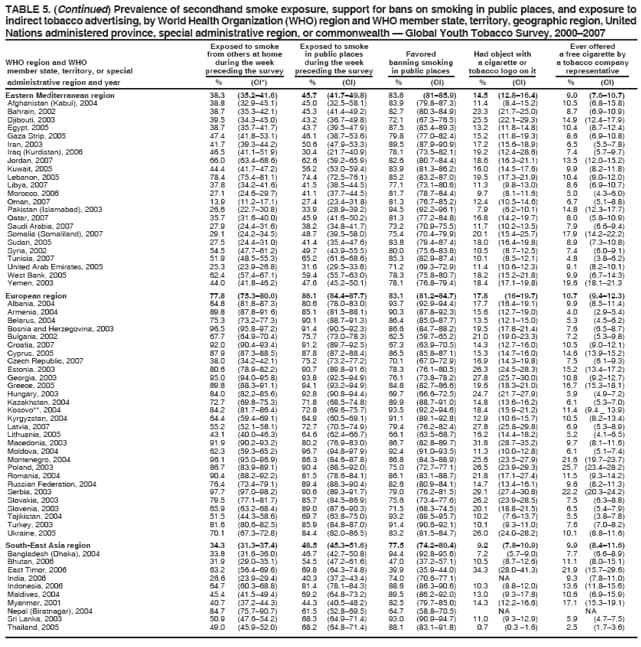 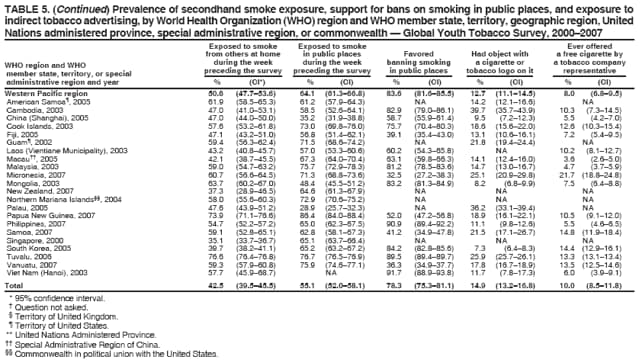 Return to top. Table 6  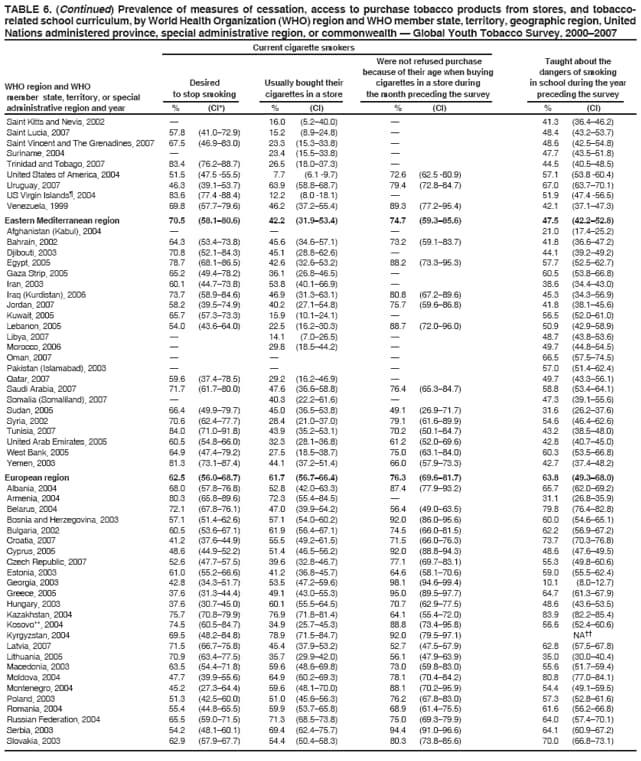 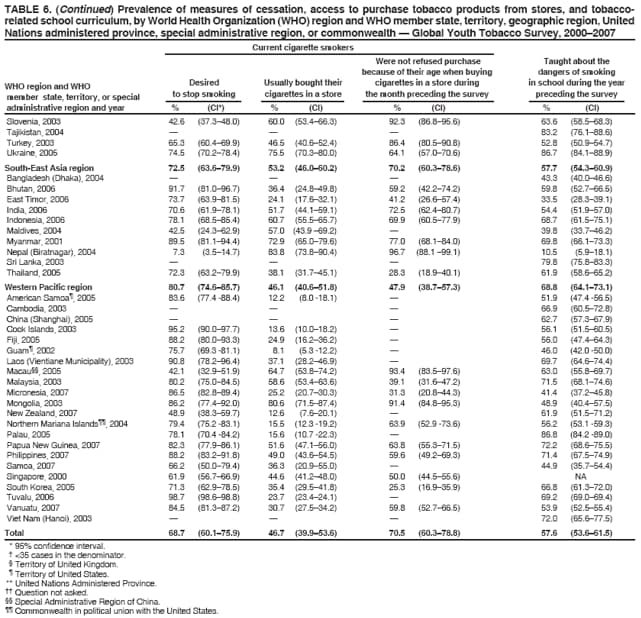 Return to top. Table 7 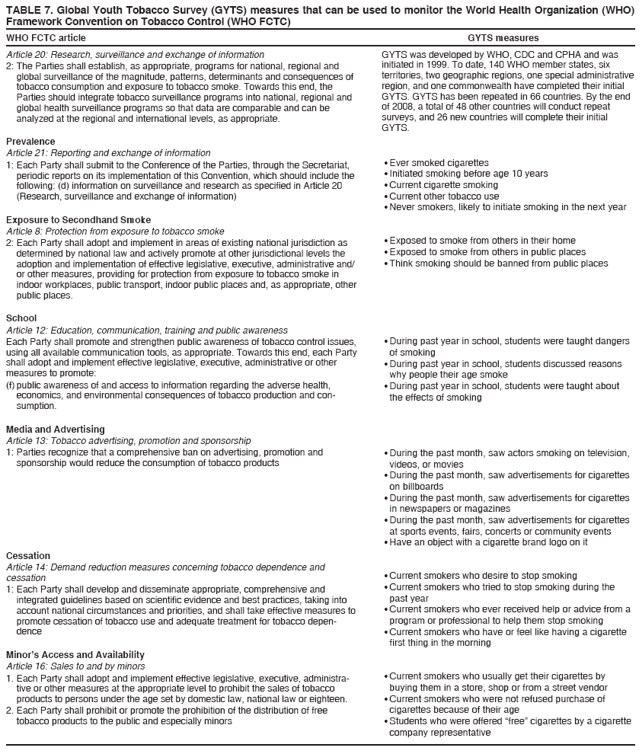 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Date last reviewed: 1/22/2008 |
|||||||||
|