 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. High-Risk Sexual Behavior by HIV-Positive Men Who Have Sex with Men --- 16 Sites, United States, 2000--2002The majority of persons living with human immunodeficiency virus (HIV) in the United States are men who have sex with men (MSM) (1). High-risk sexual behavior by HIV-positive MSM exposes sex partners to HIV. The risk for transmitting HIV from an infected partner to an uninfected partner through unprotected insertive anal intercourse (UIAI) is greater than the risk for transmission through receptive anal intercourse or oral sex (2). Differences in sexual risk behavior might be associated with the perceived HIV serostatus of the partner (i.e., HIV positive, HIV negative, or unknown serostatus) (3), as well as with the sex partner type (i.e., steady or nonsteady [4]). During May 2000--December 2002, HIV-positive MSM were interviewed in a behavioral surveillance survey at surveillance sites in 16 states*. This report describes insertive anal intercourse practices reported by these MSM; findings indicated that a large percentage of HIV-positive MSM were sexually abstinent, practiced safer sexual behavior by having protected insertive anal intercourse, or had UIAI with an HIV-positive partner. However, a small percentage of HIV-positive MSM reported UIAI with partners who were HIV negative or whose serostatus was unknown; for this group, more intensive and comprehensive HIV-prevention efforts are needed to eliminate this risk behavior. Information on selected behavioral characteristics of MSM with HIV/acquired immunodeficiency syndrome (AIDS) was obtained from CDC's Supplement to HIV/AIDS Surveillance (SHAS) project (5). SHAS is a cross-sectional, multisite study aimed at supplementing information routinely collected in HIV/AIDS surveillance. Trained staff conducted face-to-face interviews with persons aged >18 years who had HIV infection or AIDS recently reported to the 16 surveillance sites. Questionnaire modules included questions on demographics, drug use, sexual behavior, HIV testing and medical therapy, and use of health and social services. For sexually active MSM, insertive anal intercourse and condom use at last sexual encounter were compared by serostatus of the partner. Questions on sexual behavior were specific to the last sexual encounter with the most recent partner. Differences in behavior by partner type were evaluated by using the chi-square test (p<0.05); in analyses stratified by partner serostatus, percentages, odds ratios, confidence intervals, and statistical levels of significance were computed. During May 2000--December 2002, a total of 2,491 HIV-positive MSM were interviewed. MSM were defined as men categorized in the national HIV/AIDS reporting hierarchy as either "men who have sex with men" or "men who have sex with men and inject drugs," or as men who, in the interview, reported having sex with a man during the preceding 12 months or self-identified their sexual orientation as "gay" or "bisexual." Of 1,923 (77%) MSM who had HIV diagnosed for >12 months (Table 1), 1,177 (61%) reported having sex (i.e., any oral or anal intercourse) with a man during the preceding 12 months, 586 (31%) reported they were abstinent, and 160 (8%) reported they had sex but not with a man. The median number of male sex partners during this period was two (range: one to 500 sex partners). Data on sexual risk behavior were available for 1,153 MSM, who were categorized into two mutually exclusive groups based on the relationship of the sex partner(s): those who reported having only a steady partner (i.e., committed to that partner above anyone else) or any nonsteady partner. A total of 422 (37%) MSM reported having only steady male sex partners during the preceding 12 months; 408 (97%) reported having only one steady partner. A total of 731 (63%) MSM reported having nonsteady male sex partners during the preceding 12 months; 86 (12%) reported having only one partner. A significantly higher percentage of men with nonsteady partners (36%) did not know the serostatus of their most recent partner, compared with men who only had steady partners (8%; p<0.01). Among the sexually active MSM, 30% reported oral sex exclusively and 13% reported anal sex exclusively at last sexual encounter; 55% reported both behaviors. Overall, 40% of sexually active MSM reported insertive anal intercourse at last sexual encounter; of these, 25% did not use a condom. No significant differences were observed by partner type (steady versus nonsteady) for insertive anal intercourse at last sexual encounter (43% versus 38%, respectively) or not using a condom for insertive anal intercourse (28% versus 24%, respectively); therefore, data were combined by partner type. Insertive anal intercourse at last sexual encounter was significantly less likely with HIV-negative partners and partners of unknown serostatus than with HIV-positive partners (Table 2). Among men who had insertive anal intercourse at last sexual encounter, UIAI was significantly less likely with HIV-negative partners than with HIV-positive partners. No difference was observed when UIAI among HIV-positive partners was compared with UIAI among partners of unknown serostatus. Reported by: Supplement to HIV/AIDS Surveillance Project Group, participating state and local health departments. ML Campsmith, DDS, EB Begley, MPH, GV Nakamura, PhD, Div of HIV/AIDS Prevention, National Center for HIV, STD, and TB Prevention, CDC. Editorial Note:The findings in this report indicate that approximately 40% of MSM who had HIV diagnosed for >12 months did not have sex with a man (i.e., were abstinent or had sex with a woman) during the 12 months preceding the interview. Among sexually active MSM, anal sex was less common than oral sex. Insertive anal intercourse was significantly less likely with HIV-negative partners or unknown serostatus partners, compared with HIV-positive partners. Condom use for insertive anal intercourse was significantly higher with HIV-negative partners than with HIV-positive partners. Abstinence or sexual behaviors with a lower risk for transmitting HIV (e.g., oral sex, insertive anal intercourse with a seroconcordant partner, or protected insertive anal intercourse) were the common behaviors among this population of HIV-positive MSM. Certain HIV-positive MSM reported behavior that had a greater risk for HIV transmission. For MSM who had insertive anal intercourse with partners who were HIV negative or whose serostatus they did not know, 14% and 25%, respectively, did not use a condom. No significant difference in UIAI was observed between those with HIV-positive or serostatus-unknown partners. The assumption by HIV-positive MSM that partners of unknown serostatus are seroconcordant might be inaccurate, resulting in high-risk behavior with partners who are HIV negative. Recent outbreaks of sexually transmitted diseases (STDs) among MSM, including many who were HIV positive (6), indicate a possible resurgence of high-risk sexual behavior in this population. In response to the growing number of persons living with HIV/AIDS, CDC has increased its focus on prevention efforts for persons infected with HIV (those who have and have not yet received a diagnosis). In 2003, CDC launched Advancing HIV Prevention: New Strategies for a Changing Epidemic, a new initiative aimed at reducing barriers to early diagnosis of HIV and increasing access to quality medical care, treatment, and ongoing prevention services for HIV-infected persons (7). One key strategy is to prevent new HIV infections by helping persons with HIV and their partners reduce risk behavior and maintain behavior change. Current guidelines recommend routine provider-delivered prevention messages and STD screening for persons who are HIV positive (8). For those persons who have difficulty initiating and sustaining safer behaviors (e.g., adopting consistent condom use during insertive anal intercourse), higher-level interventions such as individualized support and counseling through prevention case management (9) or multisession behavioral interventions (10) might prove beneficial. The findings in this report are subject to at least four limitations. First, recruitment for SHAS was not random; participants might not represent all persons reported with HIV or AIDS from the participating sites. Second, data on sexual behaviors were self-reported and subject to recall and desirability biases. No assessment was conducted of how participants determined the serostatus of their most recent male sex partner or whether the participants had disclosed their own HIV-positive status to their sex partners. Third, the analysis was limited to UIAI with male partners and did not examine differences in receptive anal intercourse or oral sex (behaviors with a lower per-episode risk for transmitting HIV [2]) by partner type or serostatus. Finally, behavioral data were available for only the most recent sexual encounter with the most recent partner and did not include information about motivations for behavior (e.g., whether HIV-positive MSM were abstinent, limiting sexual contact to seroconcordant partners, or substituting lower-risk sex as an HIV-risk--reduction strategy). Unprotected sexual intercourse between HIV serodiscordant partners can lead to HIV transmission. This analysis suggests that although the majority of HIV-positive MSM are sexually active, most engage in behaviors with less risk for HIV transmission than UIAI. Nonetheless, UIAI occurred in 6% of the sexual encounters with HIV-negative and unknown serostatus partners. Sexual behaviors and risk-reduction strategies of HIV-positive MSM are complex and dependent on many factors, including partner relationship and perceived serostatus. To stop HIV transmission, public health authorities and health-care providers must provide effective HIV-prevention activities to those who continue to demonstrate risk behaviors. References
* Arizona, California, Colorado, Connecticut, Delaware, Florida, Georgia, Kansas, Maryland, Michigan, Minnesota, New Jersey, New Mexico, South Carolina, Texas, and Washington. Table 1 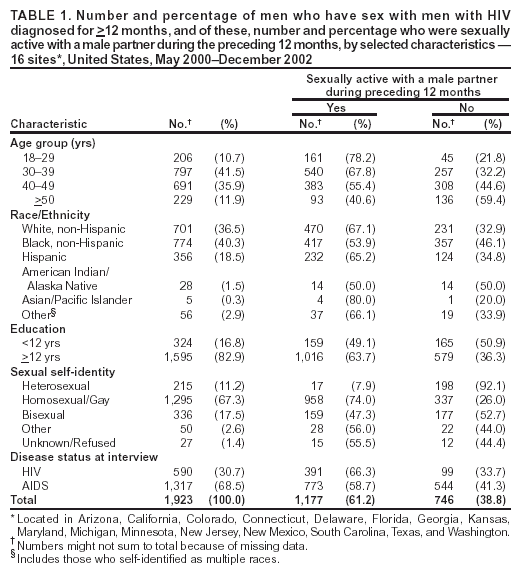 Return to top. Table 2 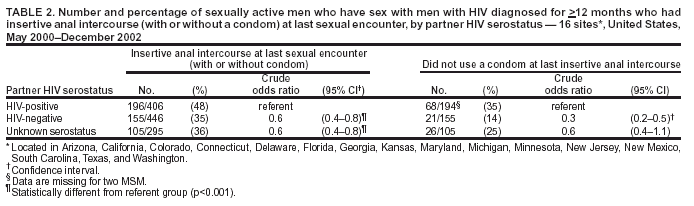 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 9/30/2004 |
|||||||||
This page last reviewed 9/30/2004
|