 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Infectious Disease and Dermatologic Conditions in Evacuees and Rescue Workers After Hurricane Katrina --- Multiple States, August--September, 2005On August 29, 2005, Hurricane Katrina struck states along the Gulf Coast of the United States. In the days after the hurricane struck, approximately 750 evacuation centers were established in at least 18 states to accommodate more than 200,000 evacuees (1). State and local health departments, with assistance from CDC, initiated enhanced infectious disease surveillance and outbreak response activities, implemented by teams of public health and rescue workers, including military personnel. Outbreak monitoring included direct reporting of conditions of public health significance to public health agencies; daily contact between CDC and local public health officials; canvassing of reports from CDC, public health departments, and news media for potential infectious disease outbreaks; and investigation of reports of infectious disease with outbreak potential. This report summarizes infectious disease and dermatologic conditions reported during the first 3 weeks after the hurricane, before effective local surveillance was fully implemented. One outbreak of norovirus was reported among evacuees in Texas; no other outbreaks requiring unusual mobilization of public health resources were reported among evacuees or rescue workers. Dermatologic ConditionsAmong hurricane evacuees from the New Orleans area, a cluster of infections with methicillin-resistant Staphylococcus aureus (MRSA) was reported in approximately 30 pediatric and adult patients at an evacuee facility in Dallas, Texas. Three of the MRSA infections were confirmed by culture (Figure and Table). In addition, 24 cases of hurricane-associated Vibrio vulnificus and V. parahaemolyticus wound infections (2) were reported, with six deaths. Among rescue workers, CDC received reports of the following two types of skin lesions with infectious etiology: tinea corporis among military personnel from two locations working in the wet environment of early evacuation efforts, and an erythematous, papular, and pustular rash consistent with folliculitis among military personnel working in Mississippi. In addition, the following three rashes subsequently determined to be noninfectious were reported in rescue workers: 1) prickly heat (miliaria crystalline, rubra, and pustulosa); 2) two clusters of nonpruritic erythematous papular, nonfollicular lesions in exposed skin of 97 military rescue workers in Louisiana presumed to have been caused by arthropod (likely mite) bites; and 3) circumferential lesions, appearing as bands of macerated skin at the waist, attributed to excessive chafing. Diarrheal DiseaseCDC received reports of clusters of diarrheal disease among persons in evacuation centers in Louisiana, Mississippi, Tennessee, and Texas. In Louisiana, approximately 20 clusters of diarrheal illness in evacuation centers were reported and investigated. In Memphis, Tennessee, gastrointestinal illness was the most common acute disease complaint among evacuees. Approximately 1,000 cases of diarrhea and vomiting were reported among adult and child evacuees in Mississippi and Texas; tests detected norovirus in stool specimens from patients in Texas. Sporadic nontyphoidal Salmonella, nontoxigenic V. cholerae O1, and other infections were identified. No confirmed cases of Shigella dysentery, typhoid fever, or infection by toxigenic V. cholerae O1 were reported in evacuees from Hurricane Katrina. Three weeks after the initial displacement caused by Katrina, few cases of diarrheal disease were being reported. Respiratory DiseaseUpper respiratory infections and pneumonias were reported among evacuees, including a case of pertussis in an infant aged 2 months who was rescued from a rooftop in New Orleans and evacuated to Tennessee. Appropriate antimicrobial prophylaxis was provided, and contact tracing identified no additional cases. Control of tuberculosis (TB) among evacuees has consisted both of detecting new cases and providing treatment continuity for previously known cases. A homeless person without a previous diagnosis of TB who was evacuated from New Orleans to Philadelphia was identified by entry screening with symptoms consistent with pulmonary TB. The patient was promptly isolated and began treatment for TB disease; a subsequent culture confirmed TB. At least eight other evacuees initially identified as potentially having TB were subsequently determined to have other conditions (e.g., lung cancer and infection with nontuberculous mycobacteria). Treatment of TB requires a multidrug regimen for at least 6 months administered under directly observed therapy (3). A total of 195 persons in the most directly affected regions (eight counties in Alabama, six parishes in Louisiana, and 11 counties in Mississippi) were known by the local public health authorities to be undergoing treatment for TB disease when Hurricane Katrina struck on August 29. Immediately after the hurricane struck, TB program staff sought out known TB patients to check their status and assure that therapy continued. As of September 23, all 27 currently known TB patients who resided in Alabama, all 21 in Mississippi, and 105 (71%) of 147 in Louisiana had been located through a coordinated local, state, and federal public health response. Of the 42 TB patients from Louisiana not yet located, 41 were considered noncontagious at the time the hurricane made landfall on the basis of disease site, treatment duration, or smear status. However, treatment needs to be completed to prevent recurrence of disease and potential for emergence of drug resistance. Intense efforts continue to locate the remaining patients. Reported by: J Jablecki, DrPH, Div TB Control, Alabama Dept of Public Health. SA Norton, MD, 14th Combat Support Hospital, Fort Benning, Georgia. R Keller, MD, Ochsner Clinic Foundation, New Orleans; C DeGraw, TB Control Section, R Ratard, MD, S Straif-Bourgeois, PhD, Louisiana Office of Public Health; Louisiana Dept of Health and Hospitals. JM Holcombe, MPPA, S Quilter, MPH, TB Control Program; P Byers, MD, M McNeill, MD, PhD, Mississippi Dept of Health. D Schlossberg, MD, DP Dohony, MPH, Philadelphia TB Control Program, Pennsylvania. J Neville, MD, Air Force Institute for Operational Health, Brooks City Base; J Carlo, MD, D Buhner, MD, Dallas County Dept of Health and Human Svcs; BR Smith, MD, C Wallace, Texas Dept of State Health Svcs. D Jernigan, MD, J Sobel, MD, M Reynolds, MD, M Moore, MD, M Kuehnert, MD, J Mott, PhD, D Jamieson, MD, Outbreak Investigations Team; G Burns-Grant, T Misselbeck, PE Cruise, P LoBue, MD, T Holtz, MD, M Haddad, MSN, Div of TB Elimination, National Center for HIV, STD, and TB Prevention; TA Clark, MD, Div of Bacterial and Mycotic Diseases, National Center for Infectious Diseases; A Cohen, MD, R Sunenshine, MD, M Jhung, MD, P Vranken, DPH, FMT Lewis, MD, LR Carpenter, DVM, EIS officers, CDC. Editorial Note:Environmental conditions after natural disasters increase the risk for infectious disease. The experience of the public health community with diarrheal disease after natural disasters suggests that evacuation centers should be prepared for considerable demands on clinic staff, janitorial services, and maintenance of personal hygiene. Access to functioning flush toilets and potable water are often impaired. Extensive flooding, such as that which followed Katrina, can increase risk for exposure to waterborne agents and vectors such as mosquitoes (4). Hurricane survivors can suffer wound injuries that can become infected. Persons unable to evacuate affected areas because of underlying illnesses might be more susceptible to infectious disease. Finally, once evacuees have relocated to evacuation centers, crowding and unsanitary conditions can amplify transmission of infectious disease. However, despite the massive migration of evacuees and their subsequent placement in evacuation centers, only one known outbreak of communicable disease (norovirus) requiring unusual mobilization of public health resources had been reported as of September 23. Observations from previous natural disasters, such as the 2004 Asian tsunami (5), suggest that skin, diarrheal, and respiratory infections are the most common infectious diseases in survivors. Infectious disease outbreaks, however, are rare following natural disasters, especially in developed countries (6,7), and specific etiologies are usually predictable, reflecting infectious diseases endemic to the affected region before the disaster. Injury and soft tissue infections are expected during the first few days after a disaster. In contrast, airborne, waterborne, and foodborne diseases are expected to occur for up to 1 month after a disaster. Because norovirus is a common cause of diarrheal illness that is easily spread in densely populated communities (e.g., classrooms and cruise ships), outbreaks can be anticipated after a natural disaster. Conversely, the rarity of toxigenic V. cholerae, dengue, and malaria in the Gulf Coast states before Hurricane Katrina suggested that they were unlikely to pose public health challenges after the hurricane. Another consequence of natural disasters is the potential exposure to dead bodies, both human and animal. No evidence exists that exposure to bodies after a disaster leads to infectious disease epidemics; however, persons handling human corpses and animal carcasses might be exposed to infectious pathogens and should use appropriate protective equipment (8). Hurricane Katrina affected an area of approximately 90,000 square miles and resulted in the displacement of approximately 1 million persons. The local and state public health infrastructure for communicable disease surveillance and control was disrupted, shifting initial emphasis toward nonstandardized mechanisms for disease reporting. These mechanisms included direct reporting to public health agencies, which resulted in timely recognition of suspected instances of infectious disease while effective local surveillance was being established. The main offices of the Louisiana Office of Public Health were affected by the hurricane, and all operations were temporarily relocated from New Orleans to Baton Rouge. Because of the compromised capacity of the Louisiana State Public Health Laboratory, laboratory confirmation of causative agents was relocated to regional public health laboratories. Effective surveillance is now under way in all of the affected states. Guidance for health-care professionals for preventing and responding to potential infectious disease outbreaks after a hurricane is available at http://www.bt.cdc.gov/disasters/hurricanes/hcp.asp. In addition to routine vaccinations, evacuees living in crowded groups should consider vaccinations for influenza, varicella, measles-mumps-rubella (MMR), and hepatitis A (available at http://www.bt.cdc.gov/disasters/hurricanes/immunizations.asp). However, immunocompromised persons (e.g., persons infected with human immunodeficiency virus, pregnant women, and persons on systemic steroids) should not receive the live viral vaccines, varicella and MMR. Screening should be performed by self-report. Methods by TB outreach workers to locate persons with previous TB infections include 1) asking known contacts whether they have heard from patients since the hurricane, 2) visiting locations known to be frequented by patients before the hurricane, 3) calling all known phone numbers for each patient, 4) checking public registries (e.g., American Red Cross Family Linking at http://www.katrinasafe.org) for updated news on patient whereabouts, and 5) seeking access to mortality records and other registries for cross-matching. A Katrina Help Desk was established on September 2 at the CDC Division of Tuberculosis Elimination to facilitate communication between the National TB Controllers Association and state TB programs as patients were relocated to other states. Health-care providers should immediately contact their state TB controllers (available at http://www.cdc.gov/nchstp/tb/katrina/tbcontrollers.htm) if an evacuee has TB symptoms (i.e., cough of >3 weeks duration, fever, chills, night sweats, or recent weight loss) or was under treatment for TB disease. The Louisiana TB Control Program (telephone 337-262-5616) will provide information about treatment regimens previously administered to relocated patients. If providers are unable to reach a local or state TB controller, they may contact the CDC Division of Tuberculosis Elimination at telephone 404-639-8336 for assistance. Acknowledgments This report is based, in part, on contributions by NB Keenon, MPH, K Taylor, MPH, Div of TB Control, Alabama Dept of Public Health. G Barre, MD, Ochsner Clinic Foundation, New Orleans; J Plough, Louisiana Office of Public Health; Louisiana Dept of Health and Hospitals. B Amy, MD, S Hand, Mississippi Dept of Health. P Hicks, MD, Children's Medical Center of Dallas; J Romero, MPH, Dallas County Dept of Health and Human Svcs; HL Duran, MD, PhD, A Groda, AJ Abell, PhD, MA Davis, MS, Texas Dept of State Health Svcs. References
Figure 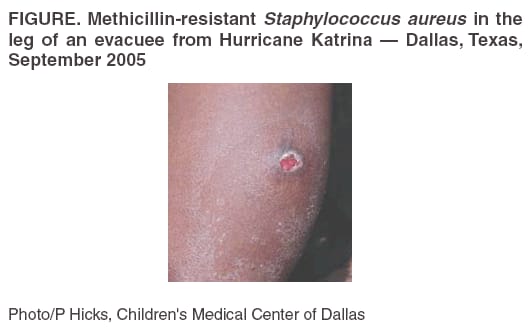 Return to top. Table 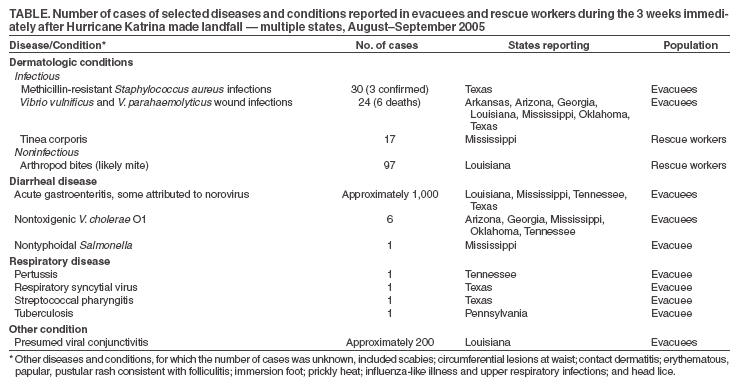 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Date last reviewed: 9/26/2005 |
|||||||||
|