
Monthy Case Studies - 2000
Case #31 - March, 2000
A 37-year-old male student from Liberia was seen at a local student health care facility for headaches and chills. He has been in the United States since 1997. The patient informed the physician that he had malaria in 1996 that was not speciated. Figures A through G are from his Wright-Giemsa stained blood smears. What is your diagnosis? Based on what criteria?
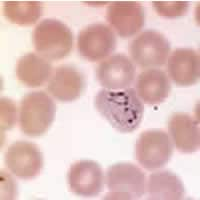
Figure A
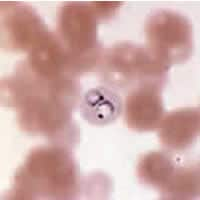
Figure B
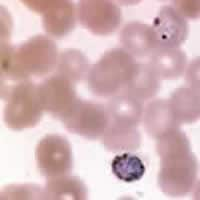
Figure C
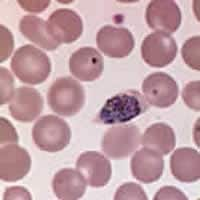
Figure D
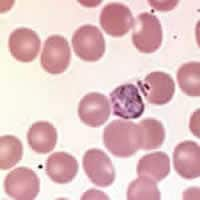
Figure E
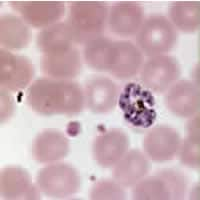
Figure F
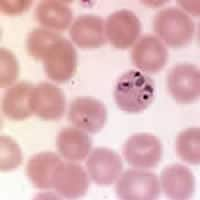
Figure G
Answer to Case #31
This was a case of malaria caused by relapsing Plasmodium ovale. Diagnostic features observed were:
- the presence of Schüffner's dots (Figure B).
- large nuclei and absence of ameboidicity (Figures B and G). In Figure A, one of the rings appears to be moderately amoeboid and this can happen with P. ovale as well as P. vivax.
- a slight enlargement of infected red blood cells, about 1.25 times normal size (Figures A, E, and F).
- a schizont with less than 13 merozoites (Figure F).
Fimbriation was not very evident in this case. When slides are prepared, laboratory conditions, primarily humidity, affect whether this reproducible artifact is present. It has been stated that "the diagnostic value of the artifact (fimbriation) is in inverse proportion to the relative humidity." Dry conditions are needed to visualize fimbriation when preparing thin smears.
Molecular techniques (PCR) also confirmed that this was a case of P. ovale.
Also of note is the epidemiology of this case. The patient is a native of Liberia, where, along with other W. African countries, there is little or no transmission of P. vivax. The reason for this is that most of the native population is Duffy Blood Group Antigen negative. This is a genetic trait that does not allow the expression of this host erythrocyte antigen, which is the critical receptor that allows P. vivax to invade red blood cells, making infection highly unlikely.
A final note: this was most likely a relapse versus a recrudescent infection because of the time frame between the patient's initial diagnosis and this episode (about three years) and the morphology of parasites seen, ruling out P. malariae. Between recrudescences, the blood infection persists; between recurrences (relapses), erythrocytic schizogony is absent in the so-called latent period.
More on: Malaria
Images presented in the monthly case studies are from specimens submitted for diagnosis or archiving. On rare occasions, clinical histories given may be partly fictitious.
 ShareCompartir
ShareCompartir


