Volume
7: No. 4, July 2010
Yukiko Asada, PhD
Suggested citation for this article: Asada Y. A summary measure of health
inequalities for a pay-for-population health performance system. Prev Chronic Dis 2010;7(4):A72.
http://www.cdc.gov/pcd/issues/2010/jul/09_0250.htm. Accessed [date].
PEER REVIEWED
Abstract
A system
that rewards population health must be able to measure and track health
inequalities.
Health inequalities have most commonly been measured in a bivariate fashion, as
a joint distribution of health and another attribute such as income, education,
or race/ethnicity. I argue this practice gives insufficient information to
reduce health inequalities and propose a summary measure of health inequalities,
which gives information both on overall health inequality and bivariate health
inequalities. I introduce 2 approaches to develop a summary measure of health
inequalities. The bottom-up approach defines attributes of interest,
measures bivariate health inequalities related to these attributes separately,
and then combines
these bivariate health inequalities into a summary index. The top-down approach measures overall health
inequality and then breaks it down into health inequalities related to different attributes. After
describing the 2 approaches in terms of building-block measurement properties, aggregation, value, data and sample size requirements, and communication, I recommend
that,
when data are available, a summary measure should use the top-down approach. In
addition, a strong communication strategy is necessary to allow users of the
summary measure to understand how it was calculated and what it means.
Back to top
Introduction
Developers of any performance reward system must select the performance
improvements that deserve rewards and ensure fairness by measuring them
appropriately.
Measurement is arguably more challenging in pay-for-performance
systems that reward population health than those that reward medical care
because determinants of population health go beyond medical care.
The questions sketched by Kindig (1) summarize challenges of measurement in a
pay-for-performance system that rewards population health: 1)
How should we measure health outcomes?, 2) How should we measure health
inequalities?, and 3)
How should we balance the need for improvement in both?
This article focuses on the second
question and calls for development of a summary measure of health inequalities,
where health inequalities associated with multiple attributes (such as income,
education, and race/ethnicity) are summarized into 1 number. I assume typical measures of population health,
such as life years or health-adjusted life
years, and population units that have a mandate for the health of their population, such as states. However, the core idea of a summary measure presented here can in principle be applied to other measures of population health and
other population units.
Back to top
Background
Because health inequality is an established field
of research and policy making, we might expect that a well-tested template
would be available for measuring health inequalities that could be used in a
pay-for-population health performance system. However, such guidance has not
yet been established. Over the past century, many empirical studies have
described health inequalities (2,3), and useful guides for measuring health
inequalities are now available (4,5). In the past few decades, jurisdictions and organizations have endorsed reducing health inequalities
(6) and have focused their efforts accordingly. The World Health
Organization’s (WHO’s) Commission on Social Determinants of Health (7) is a
notable example of such concerted efforts. Despite these efforts, progress
has been inadequate in reducing health inequalities. One reason could be the
lack of an effective strategy to measure and track health inequalities.
Health inequalities have most commonly been measured in a bivariate fashion, as a joint distribution of health and another attribute, such as income, education, sex, or race/ethnicity (8). A typical
measure of bivariate health inequality
assesses 1 attribute at a time, for example, different levels of health across
income groups (Figure 1).
The
degree of health inequality across groups can be quantified
by an index such as a range measure that compares the health of 2 groups (5). A
more sophisticated approach assesses
the level of income (or another attribute) for each
individual rather than the average level of health of each group. An index that
quantifies the degree of inequality can be complex,
for example, the Concentration Index, which compares the health of every
individual or income group
(5). Regardless of the unit of analysis (group or individual) or the inequality index used,
measures of bivariate
health inequalities always assess health inequality in relation
to another attribute.
Around 2000, there was a brief but heated debate about whether
we
should continue to measure bivariate health inequalities or start measuring
univariate health inequality (9-13). Regardless of
their association with other attributes,
measures of univariate health inequality assess health
inequality across individuals in the same way that income inequality is
typically assessed (Figure 2). A few researchers had measured health inequalities in a univariate fashion (14-16), but Murray and
colleagues proposed univariate health inequality as the
best focus in the assessment of population health (10,17,18).
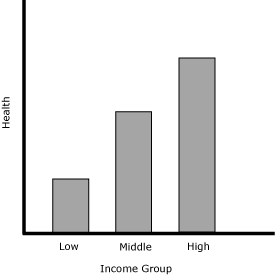
Figure 1. A hypothetical presentation of a bivariate health inequality.
Measures of bivariate health inequality assess the association of health
inequality with another attribute, in this example, income.
Figure 2. A hypothetical presentation of a univariate health inequality.
Measures of univariate health inequality assess health inequality
across individuals regardless of its association with other attributes.
This debate raised moral and policy questions (19). Health has an intrinsic
importance, those who support measuring univariate
health inequality argued, and we should not only be interested in health inequality by socioeconomic status, as
most studies have focused on, but also in how
health itself is distributed. The supporters of measuring bivariate health inequalities believed that health inequalities are significant when they are
associated with other attributes, such as income. Simply put, with an example of
income, this debate was about whether we should be worried about sick people regardless of their income level (univariate
health inequality), or about impoverished sick people more than the wealthy sick people (bivariate
health inequality).
Furthermore, those who support measuring univariate health inequality argued that the choice of which attributes
to study is generally driven by
the investigator’s intuition or
interest. Accordingly, we now have numerous empirical descriptions of health
inequalities by various attributes, which are not necessarily comparable and do not immediately offer an
overall picture of health inequalities. Univariate
health inequality, they maintained, can offer an overall picture of health
inequality in the population in a way that is comparable across populations. The advocates of
measuring bivariate health
inequalities, on the other hand, argued that univariate health inequality does not suggest how
to tailor interventions or policies to reduce health inequalities.
The result of this debate was an acknowledgment — primarily from supporters of univariate
health inequality — that bivariate and univariate health inequalities are complementary
(though exactly how they are complementary has not been specified) (20-22). Most
empirical work has continued to measure bivariate health inequalities.
Regarding univariate health
inequality
as a rarely used alternative, however, is a missed opportunity for health
inequality research and policy.
This
debate points to a need for a better strategy to measure and track health
inequalities.
This debate also suggests a strong resistance among health inequality researchers to abandoning bivariate
health inequalities. They may be resistant because 1) they view health as not only
intrinsically important but also as valuable in terms of its associations with other attributes, and 2)
it is useful to know who is sick in order to develop policies. Arguments for measuring univariate
health inequality also have merit. Lack of comparability of results and an
overall view of health inequalities may be a barrier between numerous
descriptions of health inequalities and effective policy making. A lesson from
this debate may be that we need to develop a summary measure of health
inequalities, which gives an overall picture of health inequalities in the
population while maintaining pertinent information on bivariate health
inequalities.
Back to top
Two Approaches for a Summary Measure of Health
Inequalities
Relevant literature suggests 2 approaches to developing a summary measure of
health inequalities: the bottom-up and top-down approaches.
The bottom-up approach
The bottom-up approach first defines attributes of interest and measures
bivariate health inequalities related to these attributes separately. It then combines these bivariate
health inequalities into a summary index. An example is the inequality measure developed for
the Health of Wisconsin Report Card 2007 (hereafter, the “Wisconsin
inequality measure”) (23,24). The Wisconsin inequality measure extends the Index of Disparity (25,26), a modified coefficient of variation
defined as equation no. 1.
Equation 1
Where rj is health of the jth group, rref is health of the reference group, and
J is the number of groups compared. The Index of Disparity is the average deviation of
the health of groups compared with the reference group’s health, expressed as a
percentage. When all groups have the same health, the index value is 0. Higher values suggest
more
inequality.
The Wisconsin inequality measure calculated the Index of Disparity by using all 14 groups (2 sex groups, 3 education groups, 4 rurality groups, and 5 race/ethnicity groups) and converted the index
to a letter grade for ease of communication. All attributes (sex, education, rurality, and race/ethnicity) are considered
to be of equal importance. The reference is set as the best health level among all groups (Figure 3).
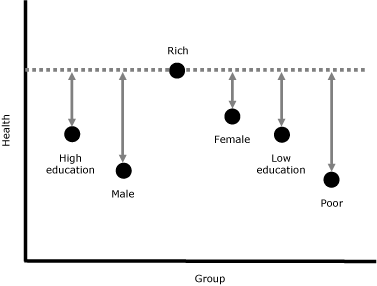
Figure 3. A simplified example of the Wisconsin health
inequality measure. To obtain the overall health inequality, calculate the difference from the reference health
level (rich) for each group (poor, low education, high education, male, and female), sum them, and divide by the number of groups minus 1 (6 − 1 = 5).
[A text description of this figure is also
available.]
The top-down approach
The top-down approach first measures univariate health inequality, then
breaks it down into health inequalities related to different attributes. Unlike
the bottom-up approach, there is no known example of a summary measure of
health inequalities using this approach. However, this approach comes close to
the principal idea underlying WHO’s health inequality measurement in the World Health Report 2000 (17,18), and similar methods have been proposed in other contexts. For
example, this approach is similar to the framework of
unfair inequalities in health and health care proposed by Fleurbaey and Schokkaert
(27), although they do not propose it for a summary measure. It is also akin to
inequality measure decomposition by attributes, though in health research
this technique is most often used with the Concentration Index (28), a sophisticated
measure of bivariate health inequality. Using decomposition, we
can tell which attributes (eg, education and sex) explain
a bivariate health inequality (eg, income-related health
inequality)
and to what degree. Although the Concentration Index decomposition is a useful tool to understand
bivariate health inequality, it is different from decomposing univariate health
inequality as a summary measure.
The top-down approach first attempts to explain the level of health of individual i by determinants of health. In the simplest form, Fleurbaey and Schokkaert
define such a “structural model” as equation no. 2.
Equation 2
hi = F(Ni, Si, Ii, Pi, Zi)
Where N is biologically determined health endowments, S is social background, I is available information, P is individual preferences, and Z is health care supply. At the risk of a gross simplification, empirically, N might be captured by age, S by income, I by education, P by health behavior such as smoking, and Z by health insurance. Variables can be extended to the community level, for example, adding neighborhood
income for S, and rurality for Z. The top-down approach then asks
which of these determinants or attributes are, following the increasingly used
term in health economics, “illegitimate” or result in unfair inequality across
individuals. For some attributes, there is a consensus on this question. For
example, health inequality associated with social background typically is
considered unfair. The top-down approach measures the distribution of hi (univariate
health inequality) and identifies the contribution of each of the illegitimate
attributes, however, defined, to univariate health inequality. Figure 4 is an example of information that the top-down approach can give.
| Attribute |
Degree of Health Inequality |
% Contribution |
| Overall |
|
|
| Income |
|
|
| Education |
|
|
| Race/ethnicity |
|
|
| Other (residual) |
|
|
Figure 4. An example of information given by the top-down approach. The top-down approach provides information on
univariate health inequality (as overall health inequality) and identifies contributions of the attributes we select (eg, income, education, and race/ethnicity). “Other (residual)” shows
univariate health inequality that
is not associated with the chosen attributes.
Back to top
Issues for Developing a Summary Measure of Health
Inequalities
Which approach is better suited to develop a summary measure of health
inequalities? To answer this question, I address the following
5 issues: building blocks, aggregation, value, data and sample size requirements,
and communication. Building blocks are common to both the bottom-up and top-down
approaches. The subsequent 4 issues separate these 2 approaches.
Building blocks
Whichever approach we take, we should carefully choose a bivariate or univariate
measure that becomes
a building block of a summary measure. The building block for the Wisconsin
inequality measure, an example of the bottom-up approach, is the Index of
Disparity, and the Gini coefficient (5) can be used as a building block for the top-down approach. To decide whether they are appropriate building blocks
on which to base a summary measure, we must examine the questions
researchers ask when choosing health inequality measures (Table 1) (4,5).
All measurement properties of the Index of Disparity and the Gini coefficient
coincide with the current discussion (4,5), except sensitivity to the mean (both measures) and subgroup
considerations
(Index of Disparity) (Table 1). The literature often recommends that researchers use both an absolute (ie, translation invariant) and a relative (ie,
scale invariant) measure (5). This recommendation reflects the lack of consensus among researchers on the issue of sensitivity to the mean. However, researchers
should choose one after trying both measures and understanding the nature and limitation of the chosen measure. Policy makers and the general public should not be
given 2 measures (and possibly two different answers) without guidance.
Insensitivity to the group size of the Index of Disparity contradicts the
recommendation in the health inequality literature (4,5). Measuring bivariate
health inequality with the Index of Disparity, we would consider the 2
populations in Figure 5, with 2 groups of different sizes, have the same degree
of inequality. We may judge that the degrees of health
inequality in these 2 populations are different
because, for example, suffering is likely to be more prevalent in Population A than
in Population B,
given its larger proportion of poor people (4). In this case, bivariate
inequality measures should be
sensitive to group size because a measure of inequality should reflect our
perception of inequality. Sensitivity to the group size, in practice, can be
incorporated in the measure by giving a proportional weight to each group (5).
Figure 5. Inequality judgment and subgroup population size. The width of the bars suggests the
proportion of poor and rich people in the 2 populations. If we consider the
degree of income-related health inequality differs in these populations, an
inequality measure should be sensitive to this difference. [A
text description of this figure is also available.]
Aggregation
The bottom-up and top-down approaches aggregate bivariate inequalities to overall health
inequality differently. The bottom-up approach aggregates bivariate inequalities
arbitrarily, and the top-down approach decomposes univariate inequality into
bivariate inequalities. This difference has 3 implications. First, the top-down
approach can identify an independent association between each attribute and
health and also interactive associations between attributes and health. Although
possible, identifying independent and interactive effects is cumbersome in the
bottom-up approach. The bottom-up approach starts by measuring unadjusted
bivariate health inequalities, where each attribute of health
inequality is measured without consideration for other attributes. We can categorize groups further, for example, from rich and poor (income) and male and female (sex) to rich male, rich female, poor male, and poor female. However, this is a time-consuming way
to describe independent and interactive effects of multiple determinants of health.
Second, the difference in aggregation between the 2 approaches leads to a difference in the meaning of an overall picture of health
inequalities.
An overall health inequality is a composite in the bottom-up approach, but it is univariate
health inequality in the top-down approach. The top-down approach has a logical
and mathematical hierarchy from bivariate health inequalities to univariate
health inequality; the sum of bivariate health inequalities equals univariate
health inequality. The bottom-up approach does not have such a hierarchy. Because each
individual in the population belongs to multiple groups (eg, an individual is
female, rich, educated, and minority), it is unclear exactly what an aggregation
of non-mutually exclusive bivariate health inequalities means.
Finally, by decomposing univariate health inequality into bivariate health
inequalities, the top-down approach can identify the contribution of each
bivariate health inequality to univariate health inequality and thus the relative
importance of bivariate health inequalities. For example, Wagstaff and van Doorslaer (29) reported that income-related health
inequality accounted for approximately 25% of univariate inequality in malnutrition among Vietnamese children and general health status among Canadian
adults, by using a subgroup decomposition technique that focuses on 1 attribute (as opposed to multiple attributes, as I am proposing here). Because of the use of a composite
to indicate overall health inequality, the bottom-up approach cannot identify
the relative contribution of each bivariate
attribute.
Value
A measure can be descriptive (describing the object) or normative (incorporating our value of the object). Using either the bottom-up or top-down approach, a summary measure of health
inequalities is normative in the most fundamental sense; it measures health
inequalities that we value. But these approaches differ in terms of how normativity is introduced, and the top-down approach offers a richer framework than the bottom-up approach. The bottom-up approach starts by selecting attributes
that we believe to be important in relation to health inequality. The top-down approach, on the other hand, starts by describing health
inequalities and moves on to normative assessment of fair and unfair health
inequalities (27). This assessment is done by selecting attributes that we believe to
cause unfair
health inequalities, and the top-down approach can embed the reasons these
attributes are important, as Fleurbaey and Schokkaert suggest in the formation
of N (health endowments),
S (social background), I (available information), P (individual preferences), and Z (health care supply) (27). These
selections and considerations can be incorporated in the bottom-up approach but are not built into it.
Furthermore, in either approach we must ask whether a summary measure of health
inequalities
should incorporate the relative importance of different attributes. According to Wagstaff and van Doorslaer (29), income-related health
inequality explains approximately 25% of overall, univariate health inequality. If we believe that income-related health
inequality is more important than
other bivariate health inequalities (eg, education-, sex-,
or geography-related health inequalities), then we might wish to reflect
our value in the measurement by giving more weight to income-related health
inequality than 25%. The Wisconsin inequality measure treats all bivariate health
inequalities as equally important. The top-down approach describes the contribution of each attribute to univariate
health inequality without considering which attribute is more important than
others. If we wish to develop a summary measure of health inequalities to
incorporate the importance of different attributes, whose values should
be included and in what way? What about concentration of burden? We may not
merely consider 1 attribute to be more important than another but
multi-attribute correlations (for example, the sick who are poor, uneducated,
and a minority) to be morally problematic. Not surprisingly, given the
uncoordinated numerous descriptions of bivariate health inequalities, the current empirical health literature is silent about these value questions.
Data and sample size requirements
Generally, the top-down approach requires more data than the bottom-up approach. The top-down approach
works best with individual-level data on health and determinants of health, while the bottom-up approach can be pursued with group-level data. Population health surveys, possibly linked with census data, may offer enough information for the top-down approach, but the sample size of the survey determines how small the population can be
for which a summary measure
of health inequalities can be calculated. Despite the clear advantage of the top-down approach in terms of aggregation and value, data and sample size requirements may be a critical hindrance to its policy application.
These considerations for data and sample size requirements are
typical in any quantitative analysis, but the use of a summary measure of health
inequalities for a system of pay-for-population health performance requires
at least 2 further considerations. First, how sensitive should a summary measure be to changes? If we agree to reward performance in
the short term (eg, in 3-5 years), a summary measure should be sensitive to changes
that occur in this time frame, and
data should be updated regularly. Second, for which population (eg, state, county, community) does it make
the most sense to establish a pay-for-performance system? The smallest population
for which data are available may not necessarily be the most appropriate size.
Communication
Effective use of a summary measure of health inequalities demands clear communication. Ideally, a measure should be conceptually and methodologically sound and easy to communicate. The bottom-up approach is arguably methodologically simpler than the top-down approach.
However, ease of communication does not necessarily equal simplicity in concepts
and methods. A complex Concentration
Index decomposition, similar to the top-down approach, has been increasingly used in policy-oriented work (28).
Complex concepts and methods require an effective communication strategy.
I suggest a summary measure of health inequalities using the top-down approach
and a strong communication strategy when data and sample size requirements are surmountable. Compared with the bottom-up approach, it offers a conceptually clearer meaning of overall health
inequality and a richer framework
for choosing relevant attributes associated with health inequality. In addition, development of a summary measure of health
inequalities requires clarification of
value questions.
Back to top
Recommendations
First, a system of pay-for-population health performance should incorporate measurement of health
inequalities. Second, measurement of bivariate health inequalities, the most
common way to measure health inequalities, may not be the most effective mechanism to reduce health
inequalities.
A system that rewards population health should seek to develop a summary measure of health
inequalities. Third, a summary measure of health inequalities can be developed
by adopting the bottom-up or top-down approach. When data are available, a summary measure using the top-down approach
should be used, along with a strong communication strategy to help users
understand what the measure means and how it was calculated. Finally, clarification of value questions is a high priority for development of a summary measure of health
inequalities.
Back to top
Acknowledgments
This manuscript was developed as part of the Mobilizing Action Toward
Community Health (MATCH) project funded by the Robert Wood Johnson
Foundation. The work was also funded by a Canadian
Institutes of Health Research New Investigator Award and a Dalhousie
Faculty of Medicine Clinical Research Scholar Award. I thank Yoko Yoshida for her assistance during the early stage of this project and anonymous reviewers for providing extensive and constructive comments.
Back to top
Author Information
Yukiko Asada, PhD, Department of Community Health and Epidemiology, Faculty of Medicine, Dalhousie University, 5790 University Ave, Halifax, Nova Scotia, B3H 1V7, Canada. Telephone: 902-494-1421.
E-mail:
yukiko.asada@dal.ca.
Back to top
References
- Kindig DA.
A pay-for-population health performance system. JAMA 2006;296(21):2611-3.
- Harper S, Lynch J, Burris S, Smith DG.
Trends in the black-white life expectancy gap in the United States, 1983-2003. JAMA 2007;297(11):1224-32.
- Mackenbach J, Bos V, Andersen O, Cardano M, Costa G, Harding S, et al.
Widening socioeconomic
inequalities in mortality in six Western European countries. Int J Epidemiol 2003;32(5):830-7.
- Asada Y.
Health
inequality: morality and measurement. Toronto,
Ontario (CA): University of Toronto Press; 2007.
- Harper S, Lynch J. Methods for measuring cancer disparities: using data relevant to
Healthy People 2010 cancer-related objectives. National Cancer Institute Cancer Surveillance Monograph Series,
No. 6. http://seer.cancer.gov/publications/disparities/. Accessed February 5, 2010.
- Graham H.
Social determinants and their unequal distribution:
clarifying policy understandings. Milbank Q 2004;82(1):101-24.
- Commission on Social Determinants of Health. Closing the gap in a generation: health equity through action on the social determinants of health. Final report of the Commission on Social Determinants of Health. http://www.who.int/social_determinants/thecommission/ finalreport/en/index.html. Accessed December 27, 2009.
- Wolfson M, Rowe G.
On measuring
inequalities in health. Bull World Health Organ 2001;79(6):553-60.
- Braveman P, Krieger N, Lynch J.
Health
inequalities and social inequalities in health. Bull World Health Organ 2000;78(2):232-3.
- Murray CJ, Gakidou EE, Frenk J.
Health
inequalities and social group differences: what should we measure? Bull World Health Organ 1999;77(7):537-43.
- Murray CJL, Gakidou EE, Frenk J. Response to P. Braveman et al. Bull World Health Organ 2000;78(2):234-5.
- Braveman P, Starfield B, Geiger HJ.
World
health report 2000: how it removes equity from the agenda for public health monitoring and policy. BMJ 2001;323(7314):678-81.
- Murray CJ. Commentary: comprehensive approaches are needed for full understanding. BMJ 2001;323(7314):680-1.
- Illsley R, Le Grand J. Measurement of inequality in health. In: Williams A, editor. Health in economics. London (GB): Macmillan; 1987. p. 12-36.
- Le Grand J. Inequality in health: some international comparison. Eur Econ Rev 1987;31:182-91.
- Silber J.
Health and
inequality: some applications of uncertainty theory. Soc Sci Med 1982;16(19):1663-6.
- World Health Organization. The world health report 2000. http://www.who.int/whr/2000/en/. Accessed December 27, 2009.
- Gakidou EE, Murray CJ, Frenk J.
Defining and measuring health
inequality: an approach based on the distribution of health expectancy. Bull World Health Organ 2000;78(1):42-54.
- Asada Y.
Is health
inequality across individuals of moral concern? Health Care Anal 2006;14(1):25-36.
- Gakidou EE, King G.
Measuring total health
inequality: adding individual variation to group-level differences. Int J Equity Health 2002;1:1-12. http://www.equityhealthj.com/content/1/1/3. Accessed December 27, 2009.
- Pradhan M, Sahn DE, Younger SD.
Decomposing world health
inequality. J Health Econ 2003;22(2):271-93.
- Smith J, Monden M.
Length of life
inequality around the globe. Soc Sci Med 2009;68(6):1114-23.
- Booske BC, Kemph AM, Athens JK, Kindig DA, Remington PL. Health of Wisconsin report card. University of Wisconsin Population Health Institute; 2007. http://uwphi.pophealth.wisc.edu/pha/healthiestState/ reportCard/2007.htm. Accessed December 27, 2009.
- Booske BC, Rohan AM, Kindig DA, Remington PL. Grading and reporting health and health disparities. Prev Chronic Dis
2010;7(1).
http://www.cdc.gov/pcd/issues/2010/Jan/08_0235.htm. Accessed February 5, 2010.
- Pearcy J, Keppel K.
A summary measure of health disparity. Public Health Rep 2002;117(3):273-80.
- Healthy people 2010. 2nd edition. Washington (DC): US Department of Health and Human Services; 2000.
- Fleurbaey M, Schokkaert E.
Unfair
inequalities in health and health care. J Health Econ 2009;28(1):73-90.
- O’Donnell O, van Doorslaer E, Wagstaff A, Lindelow M. Analyzing health equity using household survey data: a guide to techniques and their implementation.
Washington (DC): The World Bank; 2007.
- Wagstaff A, van Doorslaer E.
Overall versus socioeconomic health
inequality: a measurement framework and two empirical illustrations. Health Econ 2004;13(3):297-301.
Back to top
