

|

|

Volume
3:
No. 4, October 2006
ORIGINAL RESEARCH
Estimating Chronic Disease Deaths and Hospitalizations Due to Alcohol Use in Canada in 2002: Implications for Policy and Prevention Strategies
Jürgen Rehm, PhD, Norman Giesbrecht, PhD, Jayadeep Patra, MA, Michael Roerecke, MSc
Suggested citation for this article: Rehm J, Giesbrecht N, Patra J, Roerecke M. Estimating chronic disease deaths and hospitalizations due to alcohol use in Canada in 2002: implications for policy and prevention strategies. Prev Chronic Dis [serial online] 2006 Oct [date cited]. Available from:
http://www.cdc.gov/pcd/issues/2006/
oct/05_0009.htm.
PEER REVIEWED
Abstract
Introduction
Alcohol consumption is a factor that increases risk of chronic disease. This study estimates various indicators of alcohol-attributable premature chronic-disease morbidity and mortality for Canada in 2002.
Methods
Information on mortality and morbidity was obtained from Statistics Canada and from the Canadian Institute for Health Information database. Data on alcohol use were obtained from
the Canadian Addiction Survey and weighted for per capita consumption. Risk
information was taken from published literature and combined with alcohol
consumption information to calculate age- and sex-specific alcohol-attributable
chronic disease morbidity and mortality.
Results
In Canada in 2002, there were 1631 chronic disease deaths among adults aged 69
years and younger attributed to alcohol consumption, and these deaths were 2.4%
of the deaths in Canada for this age group. The net number of
deaths comprised 2577 deaths caused and 947 deaths prevented by alcohol
consumption. Moderate drinking was involved in 25% of deaths caused and 85% of
deaths prevented by alcohol. There were 42,996 years of life lost prematurely in
Canada due to alcohol consumption in 2002, 28,890 for men and 14,106 for women. In
Canada in 2002, there were 91,970 net chronic disease hospitalizations
attributed to alcohol consumption among individuals aged 69 years and younger. The net numbers were 124,621 hospitalizations
caused and 32,651 hospitalizations prevented by alcohol consumption.
Conclusion
With rising rates of alcohol consumption and extensive high-risk drinking, both chronic and acute damage from alcohol are expected to increase. Attention is needed to 1) create effective policies and interventions; 2) control access to alcohol; 3) reduce high-risk drinking; and 4) provide
brief interventions for high-risk drinkers.
Back to top
Introduction
According to recent studies by the World Health Organization, alcohol consumption is a leading contributor to chronic disease and is recognized as a strong risk factor affecting health in developed countries such as the United States and Canada (1-3).
In terms of global burden of disease, about 4% of disability-adjusted life years
(DALYs) worldwide in the year 2000 were attributable to alcohol. In developed countries, the percentage is still higher
with ranges for men from 8% to 18% and ranges for women 2% to 4% in the Americas
and Europe (1). Chronic
diseases such as cancer, liver cirrhosis, cardiovascular diseases, neuropsychiatric
conditions, and gastrointestinal diseases are affected by alcohol consumption
and contribute to global disease burden (3,4). In Canada, aggregate-level
studies focused on drinking and disease trends over the past 50 years indicate a strong positive association between average consumption levels and rates of
alcohol-attributable mortality (5), liver cirrhosis deaths (6), and total mortality (7).
Both the volume of alcohol consumed and high-risk drinking patterns were found to contribute to chronic disease and disability (8). In this study, the terms
heavy drinking occasion and high-risk drinking pattern are used synonymously with
binge drinking. High-risk drinking patterns impact chronic diseases, especially ischemic or other cardiovascular disease categories (9). Increased alcohol
consumption, as well as increased high-risk drinking, is expected to raise the
burden of alcohol-attributable chronic diseases
in Canada.
Recorded adult per capita alcohol consumption increased in Canada from 7.3 liters of absolute alcohol per person aged 15
years and
older in 1997 to 7.9 liters in 2004 (10,11). According to Canadian Community Health Surveys,
high-risk drinking (five or more drinks on one occasion and 12 or more
of these occasions in the past 12 months) has increased from about 11.4% in 1994 to 17.8% in 2003 (age-standardized prevalence
among the total
population aged 15 years and older) (12,13).
Prevention strategies in Canada have not provided adequate attention to the importance of appropriate prevention of alcohol consumption (14). Even when
reduction of alcohol consumption is included in prevention strategies, evidence-based effective prevention measures to reduce alcohol-attributable harm,
such as higher prices or brief interventions by health care personnel, are often ignored
(15).
The general public has little knowledge about the effects of alcohol
consumption on chronic diseases (16). Increasing this knowledge should become a
public health priority for the following reasons: 1) epidemiological evidence
indicates alcohol consumption is a major health risk factor in developed
countries (1,3); 2) there is a strong association between recent levels of
increased drinking and alcohol-attributable damage in Canada (10,11) and other
western countries; 3) damage from alcohol consumption is expected to increase, so
it is increasingly important to develop and use evidence-based interventions to reduce alcohol-attributable harm (15); and 4) alcohol tends to be overlooked as a risk factor (17) in chronic disease prevention initiatives in many western countries. This study provides
data on the impact of alcohol consumption on chronic diseases by showing estimated premature chronic-disease deaths and hospitalizations caused by alcohol in Canada for the year 2002.
Back to top
Methods
Determining chronic disease categories attributable to alcohol
Chronic disease conditions attributable to alcohol were identified through a
review of epidemiological literature that found most assessments converge on the chronic disease
categories causally related to alcohol (3,9). This study takes a conservative
approach and includes only chronic disease categories with an established
biological pathway, temporal order, consistent effects, and dose–response
relationships (18). Table 1 gives an overview of chronic conditions identified.
The meta-analyses reviewed to determine the nature of the effect of alcohol on
chronic conditions in this study showed that the effect of alcohol consumption
on chronic diseases can be detrimental or, in some cases, beneficial. The nature
of the effect (detrimental or beneficial) of alcohol on chronic conditions
depends on the level of alcohol consumed for some conditions, such as stroke
(22) or ischemic heart disease (3,21). Lower levels of consumption have a
beneficial effect; higher levels of consumption have a detrimental effect. For
type 2 diabetes mellitus among men and cholelithiasis (i.e., gall bladder
disease) among both sexes, the effect is beneficial for all drinking categories
(Table 1). Either detrimental or beneficial effects may be based on confounding
phenomena (23), which, in scientific literature, is discussed more for beneficial
than for detrimental effects.
Measurement of alcohol consumption
To measure level of alcohol consumption, we followed the approach of English et al (24) and used four drinking categories based on average volume of alcohol consumed (Table 2).
The four levels are 1) abstainer or very light drinker, 0 to less than .25
grams of alcohol per day for men and women; 2) category I, .25 to less than 20 grams
of alcohol per day for women and .25 to less than 40 grams for men; 3) category II, 20 to
less than 40 grams of alcohol per day for women and 40 to less than 60 grams for men; and 4) category III, 40
grams of alcohol or more per day for women and 60 grams or more for men. Most meta-analyses have given relative
risks based on these categories (9).
The prevalence data of
different levels of alcohol consumption were collected between 2003 and 2004
through the Canadian Addiction Survey (CAS) (25) with a total sample size
of 13,909 (n = 5,721 men and n = 8,188 women) and a 47% response rate. The CAS is a stratified (by region) and randomized (by household and respondent)
telephone-based survey of the population aged 15 years and older initiated by the
Canadian Centre on Substance Abuse (CCSA). This survey was used despite a
relatively low response rate because it had the necessary alcohol
consumption measures, a large sample size, and closest temporal proximity to
the mortality data provided by Statistics Canada (27). It has previously
been reported that higher response rates in surveys did not essentially
change distribution results of alcohol consumption
(28).
Characteristics of the CAS
sample were weighted to correspond to age and sex distribution of the
Canadian population. Average volume of alcohol consumption was derived from
a quantity–frequency measure and adjusted by adult per capita consumption (26).
Quantity of alcohol was assessed in beverage-specific drinks per usual
occasion (25). A per capita consumption adjustment was used because it is
considered the most valid choice for alcohol consumption measurements for a
population (28). Measurements based on usual quantity and frequency tend to
underestimate alcohol consumption because respondents do not usually include
heavy drinking occasions in their responses (29).
Mortality data
Mortality data, with underlying
cause of death coded according to the International Classification of
Diseases, 10th Revision (ICD-10), were obtained from Statistics Canada for
2002 (27). Comparisons of causes of death in the elderly have methodological
problems; death certificates tend to be less valid for older individuals
than for younger individuals because multiple causes of
death are often involved (30,31). In this analysis, only data for those aged
69 years and younger are included because there is indication that relative
risks, such as for ischemic heart disease and for substance-attributable
mortality and morbidity, tend to converge with increasing age (26) and to result
in overestimation of alcohol-attributable deaths caused or prevented in older age groups.
Computing alcohol-attributable
chronic-disease deaths
Alcohol-attributable fractions (AAFs) are generally defined
as the proportion of a disease in a population that will disappear if
alcohol is removed (32,33). AAFs for this study were calculated from alcohol
usage proportions in Canada and disease- and sex-specific pooled relative
risks from previous meta-analyses (Table 1) and by using the following formula:
AAF = [Σki
= 1Pi(RRi – 1)] / [Σki
= 0 Pi(RRi – 1) + 1]
where
i is the category with usage (i = 1) or no
alcohol (i = 0),
RR(i) is the relative risk at exposure level i compared with no alcohol
consumption,
P(i) is the prevalence of the ith category of alcohol
consumption, and
k is the highest drinking category (i.e., category III).
For each disease category, the sex- and age-group-specific AAFs were calculated as follows: the prevalence of alcohol consumption
(exposure category) in the population was multiplied with the excess risk
(RR-1) for the given level of alcohol consumption. The numerator in the
formula represents the sum of all alcohol-attributable cases of a
disease by exposure category within a given sex- and age-group. This sum is
divided by all cases of a disease in the given sex- and age-group to derive
a proportion that is attributable to the exposure (i.e., alcohol
consumption). The counterfactual alternative in this conceptualization is no
(or zero) consumption. To derive estimates of the number of deaths due to
alcohol for a specific disease (by sex- and age-group), the AAFs were then
multiplied by the number of deaths from that specific disease within the
sex- and age-group.
We cite a meta-analysis for each condition (e.g., malignant neoplasms,
type 2 diabetes mellitus, neuropsychiatric conditions, cardiovascular diseases,
digestive diseases) (18) (Table 1) to derive information of relative risk
for the diverse categories. Meta-analyses usually cited are from Gutjahr et
al (19), a series of meta-analyses based on English et al (24). The Gutjahr
et al meta-analyses incorporate literature published since publication of
the English et al paper. For some disease categories, other meta-analyses
were cited if they were more comprehensive than the Gutjahr et al paper. For
stroke, we based relative risks on Reynolds et al (22) because, contrary to
other authors, this work separates ischemic and hemorrhagic stroke. Alcohol
usage has been shown to differentially influence both types of stroke (3). For
hemorrhagic stroke, the effect of alcohol consumption, even at low levels,
is detrimental for men (34); for women, the effect may be protective at
low levels of drinking (categories I and II) (20), but the effect
depends on the pattern of drinking (35). The effect of alcohol consumption
on ischemic stroke is partly protective for low to moderate consumption
levels (35), and the beneficial effect is more pronounced among women. For
depression data, we used mental health surveys to estimate AAFs directly and
took into consideration the rates of comorbidity and time of onset for
alcohol use disorders and depression in comparison to other mental diseases
comorbid with alcohol (3).
No alcohol consumption was used as a counterfactual scenario that was
selected for the following reasons: 1) the counterfactual of zero
consumption is the most widely used and allows comparisons with other
studies; 2) the level of alcohol associated with lowest burden differs from
country to country and is different for mortality and morbidity; 3)
alcohol-attributable harm is related to average volume of alcohol
consumption and consumption patterns; and 4) selection of any volume of
consumption other than zero without considering the other dimensions would
be arbitrary (36,37).
We calculated AAFs separately by sex and age (men and women 15–29 years, 30–44 years, 45–59 years, 60–69 years). To show detrimental
and beneficial effects of alcohol, we applied AAFs to Canadian mortality data
(27) to estimate the number of alcohol-attributed deaths by age and sex.
A negative AAF, in this case, means that more deaths were prevented than caused
by alcohol for the respective disease condition (Table 3).
Potential Years of Life Lost
We hypothesized that persons dying due to alcohol consumption would have lived longer if they had not
consumed alcohol. The average extra time such individuals would have lived is known as
residual life expectancy. If a man died of alcoholic liver cirrhoses at age 50 in Canada, he would have a residual life expectancy of 28.4 years (38). The sum of residual life expectancies for people dying
from alcohol consumption is known as potential years of life lost (PYLL) due to
alcohol. PYLL for each sex- and age-group can be estimated by interpolating the observed mean age at death and the standard life expectancies tables for
each respective sex– and age–group. This study uses the World Health Organization (WHO) 2000 standard life expectancies table for Canada
(38).
To calculate the mean ages within age intervals, we followed rules specified by the WHO Global Burden of Disease study
(39). Canadian PYLL were calculated for each age group (15–29, 30–44, 45–59, and 60–69) by multiplying the number of deaths by the
interpolated life expectancy for the observed mean age at death for the age interval. The
upper age limit of 76.0 years for men and 81.5 years for women was used to approximate Canadian life expectancy at birth. PYLL
were calculated per 100,000 population (Table 4).
Data on hospital diagnoses
Canadian fiscal year 2002 to 2003 hospital diagnoses data (ICD-10) were obtained from the Canadian Institute for Health Information (CIHI) Hospital Morbidity Database (HMDB) for both national and provincial levels (40). National data were available for seven provinces (Alberta, British Columbia, Newfoundland, Nova Scotia, Ontario, Prince Edward Island, Saskatchewan) and two territories (Northwest
Territories and Yukon) and were provided for disease conditions, and sex- and
age-groups in
5-year segments. Data for the provinces of Quebec, Manitoba, New Brunswick, and Nunavut (a northern territory) were not available according to
ICD-10 classifications. Aggregated data for each condition were estimated based on total population and the combined data of available provinces and territories. The HMDB captures information on patients separated (through discharge or death) from acute-care facilities in Canada and provides national data on acute-care hospitalizations by diagnoses and procedures. Diagnoses were categorized based on most responsible diagnosis (MRD) of hospitalized patients. In cases where multiple diagnoses may be classified as most responsible, the diagnosis associated with
the longest stay in a hospital was used. AAFs were then applied to hospital data to estimate alcohol-attributable hospital diagnoses for each treatment facility by age and sex.
Back to top
Results
Alcohol-attributable mortality
This study estimates premature deaths and hospitalizations for Canadians aged
69 years and younger and provides an overview of the 2002 estimated volume of
alcohol exposure in Canada by sex- and age-group. As expected, men consumed on
average more than women, and alcohol consumption decreased with age.
Table 5 provides estimates of
alcohol-attributable deaths — deaths caused or prevented by alcohol consumption.
In Canada in 2002, there were 1631 net alcohol-attributable premature deaths
estimated, 1155 deaths among men and 476 among women. These numbers were derived
by multiplying AAFs with number of deaths for each category to produce numbers
with decimals. As a result, there may be minor rounding errors after collapsing
numbers across different categories.
The 1631 alcohol-attributable deaths constituted 2.4% of the deaths
in Canada for people aged 69 years and younger. These were net figures, and the
estimates of deaths prevented by alcohol have been taken into account. There
were 2577 deaths (1906 men and 672 women) attributable to alcohol and 947
deaths (751 men and 195 women) prevented by alcohol consumption. Figures were calculated
by using the epidemiological procedure previously described.
Moderate drinking (category
I, less than 20g per day of pure alcohol for women and less than 40g per day for men) was associated with 25% of deaths caused by alcohol consumption and
85% of deaths prevented by alcohol consumption. In this group of moderate
drinkers, the deaths prevented (n = 827) outnumbered deaths caused (n = 677) by
alcohol use.
Among premature deaths caused by alcohol, malignant neoplasms accounted for 891 deaths (608 men and 283 women), and digestive diseases accounted for 881 deaths (663 men and 218
women) (Table 3). Among deaths prevented by alcohol for those aged 69 and
younger, 788 prevented deaths were ascribed to ischemic heart disease (678
men and 110 women).
Figure 1 gives an overview of deaths prevented and caused by alcohol. Of the deaths caused by alcohol, including detrimental effects of alcohol on some cardiovascular diseases, cancer
(34.6%) and digestive diseases (34.2%) had the highest proportions of deaths caused by alcohol.
Figure 1. Alcohol-attributable chronic-disease
mortality in people aged 69 years or
younger in Canada, 2002. [A tabular version of this chart is also available.]
Alcohol-attributable PYLL
In 2002, the PYLL rate for Canada for premature deaths due to alcohol was 196 per 100,000 for men and 92 per 100,000 for women aged
15 to 69 (Table
4). For every population of 100,000, there was a potential net loss of 196 years of life among men and 92 years of life among women as a result of premature death due to alcohol
consumption. In total, 42,996 potential years of life were lost due to alcohol in
Canada in 2002.
Alcohol-attributable hospitalizations
Table 6 provides estimates of alcohol-attributable diagnoses for those aged 69 and younger, and Table 7 shows AAFs applied to hospital data to estimate
alcohol-attributable fractions and mean age at hospital diagnosis. In Canada for fiscal year 2002
to 2003, 91,970 alcohol-attributable
diagnoses among hospital diagnoses from acute care facilities were estimated and
accounted for 65,161 hospital separations for men and 26,809 for women. These
numbers were derived by multiplying AAFs with number of diagnoses for each
category to produce numbers with decimals. As a result, there may be minor
rounding errors after collapsing numbers across categories.
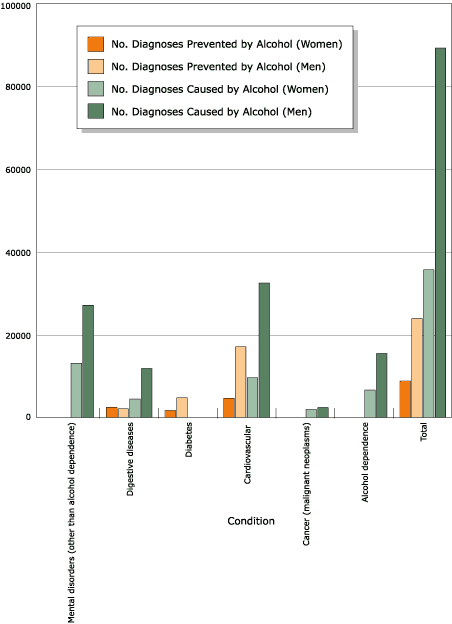
Figure 2. Alcohol-attributable chronic disease diagnoses
in population aged 69 years or younger in Canada, 2002. [A tabular version of this chart is also available.]
Figure 2 gives an overview of alcohol-attributable chronic disease
diagnoses. The number of diagnoses (91,970) is a net figure and includes estimates of
hospital separations prevented by alcohol consumption. There were 124,621
acute-care hospital diagnoses (hospital separations for 89,022 men and
35,599 women) caused by alcohol and 32,651 hospital diagnoses (23,861
men and 8790 women) prevented by alcohol consumption. Among acute-care
hospital diagnoses attributable to alcohol, neuropsychiatric conditions
accounted for 49.9%, cardiovascular disease 33.7%, digestive diseases 13.0%,
and cancer (malignant neoplasms) 3.4% of diagnoses (Table 6).
Back to top
Discussion
This analysis presents the main associations between alcohol consumption and
death and hospitalization due to chronic disease in Canada in 2002. General limitations
of the study include the fact that it relies on secondary analysis of existing
data, such as official statistics, and these sources have limitations and
potential errors. As noted previously, the Canadian Addiction Survey, although
it had a modest response rate, was the best resource available to calculate
average alcohol consumption by age and sex. People aged 70 and older were excluded from the analysis
because there is less confidence in diagnoses among this age group. The assumption that alcohol-attributable relative risks as seen through meta-analyses are transferable between countries may introduce error.
Based on meta-analyses used and their systematic exploration of variance, the chronic
disease bias may not be large for a country like Canada (24,19,41).
Another potential bias is that detailed hospitalization data were missing for three provinces and one territory.
Because current analyses did not focus on provincial comparisons, the effect is probably minimal. The adjustment for
adult per capita alcohol consumption may result in an overestimate
because underlying epidemiological estimates were usually not adjusted. In Rehm et al (26), the authors
quantified potential overestimation for health effects of alcohol and came to the conclusion that this effect for Canada is limited. Consequently, data are presented with adjustment to be comparable with mainline research such as the WHO Comparative Risk Assessment within the Global Burden of Disease
project (1,2,4).
International research, including the WHO Global Burden of Disease study (1), show
that alcohol is a risk factor for
numerous malignant neoplasms, neuropsychiatric conditions, cardiovascular diseases, and digestive diseases in both developed and developing countries. The number of premature deaths associated with alcohol varies greatly between general categories and specific conditions within a
category. Digestive diseases and malignant neoplasms are implicated in similar numbers of alcohol-attributable premature deaths in Canada in 2002, and these
disease categories are followed by neuropsychiatric conditions. However, an
overall protective effect was estimated for cardiovascular disease mortality.
A somewhat different picture emerges when focusing on hospital diagnoses. The greatest numbers of alcohol-attributable conditions in the hospital diagnoses category are neuropsychiatric conditions associated with alcohol use. These are followed by cardiovascular diseases, digestive diseases, and malignant neoplasms. There are also substantial alcohol-attributable treatments of neuropsychiatric
conditions in specialized treatment systems outside of acute-care hospitals.
AAFs generally show at least double the number of deaths or hospitalizations among men compared
with
women. By age group, the absolute number of deaths is greatest among those aged 45 to 59, followed by those aged 60 to 69. There is a similar age-specific pattern for hospital diagnoses. Total PYLL are estimated at
more than 42,000 in Canada for 2002. Alcohol-attributable chronic diseases impact
many people during their adult productive years as well as young adults and youth. There are substantial social costs and economic burdens related to diagnoses, treatment, medication, and care.
The findings in this study are generally in line with international research
on alcohol and chronic disease as reported in the WHO Global Burden of Disease
project (1,2,3) and with analyses of causes of death in the United States (42).
In developed countries, such as Canada and the United States, alcohol is a
noteworthy risk factor for chronic and acute disease, disability, and death. The
WHO Global Burden of Disease project estimated that in developed countries alcohol was
responsible for 9.2% of burden of disease compared with 12.2% from tobacco and
10.9% from high blood pressure. The estimated contribution from alcohol was
greater than that from high cholesterol, high body mass, low fruit and vegetable intake,
or physical inactivity (1,2).
Effective interventions and policies are needed if alcohol-attributable chronic diseases are to be reduced. Babor et al (15) have provided an evidence-based analysis of interventions and alcohol policies that have been shown to be effective in controlling the damage of chronic disease
and other harm associated with alcohol use. Their analysis examined hundreds of published evaluations of interventions and rated
them on the following four criteria: 1) evidence of effectiveness, 2) breadth of research report, 3) assessment across cultures, and 4) costs to implement. Their analysis took into account the target group in general, adverse side effects, population reach (e.g., number of people affected by the intervention), and political and economic feasibility. The Babor et al assessment pointed to
several alcohol-related policies that are effective in controlling and reducing harm from alcohol consumption and that are also relevant in reducing alcohol-related chronic disease. Their study included information on measures that control access to alcohol (e.g., increased real price of alcoholic beverages, lower density of outlets, government alcohol retailing systems), server interventions to
prevent service to intoxicated patrons, and brief interventions (short counseling sessions) directed at high-risk drinkers.
An increase in real price of alcoholic beverages has been shown to reduce
not only the consumption of moderate drinkers but also the consumption of high-risk drinkers as indicated by
declining cirrhosis mortality (43). The Babor et al research (15) and supporting work (44–46) indicate that alcohol access control has a preventive impact at the population level for men and women. Access control measures have also been found to have beneficial impacts on specific sectors of a population,
such as occasional high-risk drinkers, chronic heavy drinkers, and youth. In general, control measures have greater impact on
high-risk drinkers than on moderate drinkers (15,44,46).
Research by Norström based on European and Canadian data (7) has shown that at the population level, cardiovascular mortality levels are not reduced by
an increasing rate of alcohol consumption nor elevated by lowering consumption
rate. At the population level, there may be no net benefits for cardiovascular disease
for those with a higher alcohol consumption level but an increased risk of both chronic and
acute damage (7,15).
Additional prevention-based evaluations are needed to assess whether public health benefits of controls on access to alcohol can be further enhanced by combining control measures with other targeted interventions (e.g., server interventions in establishments that sell alcohol and brief interventions for
high-risk drinkers who
come into contact with health facilities). Population-level interventions
could be combined with targeted alcohol awareness messages delivered by health experts and their combined impact assessed. Physicians, nurses, and other health care providers should be encouraged to advise patients routinely about the risks for chronic disease associated with alcohol consumption when they do routine patient monitoring.
Both population-level phenomena (e.g., overall per capita consumption,
societal prevalence of high-risk drinking) and individual drinking behaviors are
important considerations for alcohol-related prevention initiatives. Efforts to
prevent chronic disease need to address risk factors, including alcohol
consumption, through focused resources and program coordination in ways that ensure initiatives are
informed by epidemiological evidence. Because there is a rising rate of alcohol
consumption and high-risk drinking in Canada, increased damage from alcohol is
expected. Effective policy, intervention, and prevention efforts are needed, as
is public recognition of alcohol as a contributor to chronic disease. Medical,
health care, and public health professionals have important roles in drawing
attention to alcohol damage and other risk factors for chronic disease and in
supporting effective interventions.
Back to top
Acknowledgments
The authors gratefully acknowledge the contributions of the Second Canadian Study on Social Costs of Substance Abuse, funding from the Canadian Centre on Substance Abuse, and Health Canada for support to prepare an overview paper on alcohol and chronic disease for the National Alcohol Strategy Working Group.
Back to top
Author Information
Corresponding Author: Jürgen Rehm, Public Health and Regulatory Policies, Centre for Addiction and Mental Health, University of Toronto, 33 Russell St, Room 2035, Toronto, Ontario, Canada M5S 2S1. Telephone: 416-535-8501, ext. 6907. E-mail: jtrehm@aol.com. Dr Rehm is also associated
with Public Health Sciences, Faculty of Medicine, University of Toronto,
Ontario, Canada; the Research Institute
for Public Health and Addiction, Zurich, Switzerland; and the Technische
Universität Dresden, Germany.
Author Affiliations: Norman Giesbrecht, Centre for Addiction and Mental
Health and Public Health Sciences, University of Toronto, Ontario, Canada; Jayadeep Patra,
Centre for Addiction and Mental Health and Human Development and Applied Psychology, University of Toronto, Ontario, Canada; Michael Roerecke, Centre for Addiction and Mental Health and Public Health
Sciences, University of Toronto, Ontario, Canada.
Back to top
References
- World Health Organization. World Health Report 2002: reducing risks, promoting healthy life. Geneva
(CH): World Health Organization; 2002.
- Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ; Comparative Risk
Assessment Collaborating Group.
Selected major risk factors and global and regional burden of disease. Lancet 2002;360(9343):1347-60.
- Rehm J, Room R, Monteiro M, Gmel G, Graham K, Rehn N, et al. Alcohol use. In: Ezzati M, Lopez A, Rodgers A, Murray C, eds. Comparative quantification of health risks: global and regional burden of disease attributable to selected major risk factors. Vol 1. Geneva
(CH): World Health Organization; 2004. p. 959-1109.
- Rehm J, Room R, Monteiro M, Gmel G, Graham K, Rehn N, et al.
Alcohol as a risk factor for global burden of disease. Eur Addict Res 2003;9(4):157-64.
- Ramstedt M.
Alcohol consumption and alcohol-related mortality in Canada, 1950-2000. Can J Public Health 2004;95(2):121-6.
- Ramstedt M.
Alcohol consumption and liver cirrhosis mortality with and without the
mention of alcohol--the case of Canada. Addiction 2003;98(9):1267-76.
- Norström T.
Per capita alcohol consumption and all-cause mortality in Canada, 1950-98. Addiction 2004;99(10):1274-8.
- Rehm J, Ashley MJ, Room R, Single E, Bondy S, Ferrence R, et al.
On the emerging
paradigm of drinking patterns and their social and health consequences. Addiction 1996;91(11):1615-21.
- Rehm J, Room R, Graham K, Monteiro M, Gmel G, Sempos CT.
The relationship of
average volume of alcohol consumption and patterns of drinking to burden of disease: an overview. Addiction 2003;98(9):1209-28.
- Statistics Canada. The control and sale of alcoholic beverages in Canada.
Catalog 63-202-XIB. Ottawa (ON):
Government of Canada; 2002.
- Statistics Canada. The control and sale of alcoholic beverages in Canada.
Catalog
63-202-XIE. Ottawa (ON): Government of Canada; 2005.
- Statistics Canada. National Population Health Survey 1999. Ottawa (ON):
Government of Canada; 1999.
- Statistics Canada. Canadian Community Health Survey 2004. Ottawa (ON):
Government of Canada; 2004.
- Haydon E, Roerecke M, Giesbrecht N, Rehm J, Kobus-Matthews M. Chronic disease
in Ontario and Canada: determinant, risk factors, and prevention priorities. Toronto
(ON): Ontario Public Health Association; 2005.
- Babor T, Caetano R, Casswell S, Edwards G, Giesbrecht N, Graham K, et al.
Alcohol: no ordinary commodity. Research and public policy. Oxford (UK): Oxford University Press; 2003.
- Anglin L, Giesbrecht N, Ialomiteanu A, Grand L, Mann R, McAllister J. Public
opinion on low-risk drinking, alcohol and cancer, and alcohol policy issues: findings
from the 2004 CAMH Monitor Survey of Ontario adults. Toronto (ON): Centre for Addiction & Mental Health;
2005.
- Chronic Disease Prevention Alliance of Canada. Integrated chronic disease
prevention: getting it together. Conference proceeding from the First National Conference. 2004 Nov 6; Ottawa,
ON.
- Hill AB.
The environment and disease: association or causation? Proc R Soc Med.
1965;58:295-300.
- Gutjahr E, Gmel G, Rehm J.
Relation between average alcohol consumption and
disease: an overview. Eur Addict Res 2001;7(3):117-27.
- Ridolfo B, Stevenson C. The quantification of drug-caused mortality and morbidity in
Australia, 1998. Canberra (AS): Australian Institute of Health and Welfare; 2001.
- Corrao G, Rubbiati L, Bagnardi V, Zambon A, Poikolainen K.
Alcohol and coronary
heart disease: a meta analysis. Addiction 2000;95(10):1505-23.
- Reynolds K, Lewis B, Nolen JD, Kinney GL, Sathya B, He J.
Alcohol consumption
and risk of stroke: a meta-analysis. [Published erratum in: JAMA
2003;289(21):2798]. JAMA 2003;289(5):579-588.
- Naimi TS, Brown DW, Brewer RD, Giles WH, Mensah G, Serdula MK, et al.
Cardiovascular risk factors and confounders among nondrinking and moderate-drinking U.S. adults. Am J Prev Med 2005;28(4):369-73.
- English D, Holman C, Milne E, Winter M, Hulse G, Codde G, et al. The
quantification of drug-caused morbidity and mortality in Australia, 1995. Canberra
(AS): Commonwealth Department of Human Services and Health; 1995.
- Canadian Centre on Substance Abuse. Canadian Addiction Survey 2004: Microdata
eGuide. Ottawa (ON): Canadian Centre on Substance Abuse; 2004.
- Rehm J, Patra J, Popova S.
Alcohol-attributable mortality and potential years of life
lost in Canada 2001: implications for prevention and policy. Addiction 2006;101(3):373-84.
- Mortality Database [CD-ROM]. Ottawa (ON): Statistics
Canada;2005.
- Gmel G, Rehm J. Measuring alcohol consumption. Contemp Drug Probl
2004;31:467-540.
- Dawson DA.
Volume of ethanol consumption: effects of different
approaches to measurement. J Stud Alcohol 1998;59(2):191-7.
- Minder CE.
Quality of coding of causes of death in Switzerland. Soz
Praventivmed 1984;29(6):248-50. [German].
- Kesteloot HE, Verbeke G.
On the relationship between all-cause, cardiovascular,
cancer, and residual mortality rates with age. Eur J Cardiovasc Prev Rehabil 2005;12(2):175-81.
- Walter SD.
The estimation and interpretation of attributable risk in
health research. Biometrics 1976;32(4):829-49.
- Walter SD.
Prevention of multifactorial diseases. Am J Epidemiol 1980;112(3):409-16.
- Berger K, Ajani UA, Kase CS, Gaziano JM, Buring JE, Glynn RJ, et al.
Light-to-moderate alcohol consumption and risk of stroke among U.S. male
physicians. N Engl J Med 1999;341(21):1557-64.
- Hillbom M.
Alcohol consumption and stroke: benefits and risks.
Alcohol Clin Exp Res 1998;22(7 Suppl):352s-58s.
- Rehm J, Monteiro M, Room R, Gmel G, Jernigan D, Frick U, et al.
Steps towards constructing a global comparative risk analysis for alcohol
consumption: determining indicators and empirical weights for patterns of
drinking, deciding about theoretical minimum, and dealing with different
consequences. Eur Addict Res 2001;7(3):138-47.
- Murray CJ, Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S.
Comparative quantification of health risks conceptual framework and
methodological issues. Popul Health Metr 2003;1(1):1.
- World Health Organization. Discussion Paper No. 40:
Life tables for 191 countries for 2000: data, methods, results. Geneva (CH):
World Health Organization; 2000.
- Mathers CD, Vos A, Lopez AD, Salomon J, Ezzati M. National burden of disease
studies: a practical guide. Global program on evidence for health policy.
2nd ed. Geneva (CH): World Health Organization; 2001.
- Canadian Institute for Health Information. Hospital Morbidity
Database [CD-ROM]. Ottawa (ON): Canadian Institute for Health Information; 2004.
- Corrao G, Bagnardi V, Zambon A, Arico S.
Exploring the dose-response
relationship between alcohol consumption and the risk of several
alcohol-related conditions: a meta-analysis. Addiction 1999;94(10):1551-73.
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL.
Actual causes of death in
the United States, 2000. [Published erratum in: JAMA 2005;293(3):293-4.
JAMA 2005;293(3):298]. JAMA 2004;291(10):1238-45.
- Cook PJ, Tauchen G. The effect of liquor taxes on heavy drinking. Bell
Journal of Economics 1982;13:379-90.
- Edwards G, Anderson P, Babor T, Casswell S, Ferrence R, Giesbrecht N, et al.
Alcohol policy and the public good. New York (NY): Oxford University Press; 1994.
- Holder H, Edwards G. Alcohol and public policy: evidence and issues.
Oxford (UK): Oxford University Press, 1995.
- Giesbrecht N, Greenfield T. Preventing alcohol-related problems in the U.S. through
policy: media campaigns, regulatory approaches, and environmental interventions. J Prim Prev 2003;23:63-104.
Back to top
|
|
