

|

|

Volume 1:
No. 4, October 2004
SPECIAL TOPICS IN PUBLIC HEALTH
The eHealth Behavior Management Model: A
Stage-based Approach to Behavior Change and Management
Robert J. Bensley, PhD, Nelda Mercer, MS, John J. Brusk, MPH, Ric
Underhile, PhD, Jason Rivas, Judith Anderson, DrPH, Deanne Kelleher, MS,
Melissa Lupella, MPH, André C. de Jager, DPhil
Suggested citation for this article:
Bensley RJ, Mercer N, Brusk JJ, Underhile R, Rivas J, Anderson J,
et al. The ehealth behavior management model: a stage-based
approach to behavior change and management. Prev Chronic
Dis [serial online] 2004 Oct [date cited]. Available
from: URL: http://www.cdc.gov/pcd/issues/2004/
oct/04_0070.htm.
Abstract
Although the Internet has become an important avenue for disseminating health
information, theory-driven strategies for aiding
individuals in changing or managing health behaviors are lacking.
The eHealth Behavior Management Model combines the Transtheoretical Model, the behavioral intent aspect of the
Theory of Planned
Behavior, and persuasive communication to assist individuals in negotiating the
Web toward stage-specific information. It is here — at the point of stage-specific
information — that behavioral intent in moving toward more active stages of change
occurs.
The eHealth Behavior Management Model is applied in three demonstration projects
that focus on behavior management issues: parent-child nutrition education among
participants in the U.S. Department of Agriculture Special Supplemental
Nutrition Program for Women, Infants and Children; asthma management
among
university staff and students; and human immunodeficiency virus prevention among
South African women.
Preliminary results have found the eHealth Behavior Management Model to be
promising as a model for Internet-based behavior change programming.
Further application and evaluation among other behavior and
disease management issues are needed.
Back to top
Introduction
It has been 30 years since the release of A New Perspective
on the Health of Canadians: A Working Document (1). This
report solidified the role of lifestyle behaviors as the most
likely cause of premature death and sparked a flurry of
international efforts toward preventing and
reducing the occurrence of behaviors known to be determinants of morbidity and
mortality. For the past 30 years, health-risk
behavior has continued to be a prime focus of public health
efforts. The leading causes of death in the United States are dominated by
health-risk behaviors — with tobacco use, poor diet, physical
inactivity, and alcohol consumption contributing to nearly 40% of
all U.S. deaths (2).
As a greater focus on behavioral determinants of health
evolved, so did the development and implementation of theories and models of behavior.
Focus has increased on individual health behavior
theories and models such as the Theory of Planned Behavior, the
Health Belief Model, and the Transtheoretical Model. The Transtheoretical Model
is one of the most popular models for describing the processes that individuals
undergo as they move through stages of
readiness to change behaviors (3).
It is not the intent of this paper to provide an
in-depth discussion of the merits of behavior change and
prevention of premature death. It is also not the intent to compare and contrast
the myriad behavior change theories and models. Rather, the
purpose of this paper is to present the eHealth Behavior Management Model, a
behaviorally focused model that applies
existing theories to one of the newest and
greatest potential avenues of intervention: the Internet (4).
In a little more than a decade, the Internet has
grown from a collection of remote pages to an unparalleled
information source. By 2003, it was estimated
that more than 600 million users online worldwide were accessing
more than 170 million Web sites (5,6). The number of individual Web
pages is difficult to determine. At least three billion pages
currently exist, based on the size of the Web page
index for Google, the largest search engine in the world (5). The number of
health-related Web pages in a simple Google search using the keyword
“health” netted nearly 250 million Web
pages.
The Internet is used by a variety of populations. For example, more than
20% of people over the age of 65 have reported using the
Internet, with two out of three having used the Internet to seek health
information (7). Populations typically perceived to be hard to reach,
such as lower-income populations, are also using the
Internet. One of the projects described in this paper found
that nearly 60% of the 20,000 lower-income participants who accessed
an Internet-based behavior change project did so from their own
homes (8). This high rate of home-based computer access among
lower-income populations has also been observed elsewhere (9). The U.S.
Department of Health and Human Services recognizes the growing importance of
the Internet as a means for accessing health-related information. Baseline data
for Healthy People 2010 show that an estimated 26% of U.S. homes had access
to the Internet in 2000; the goal of Healthy People 2010 is to increase
this percentage to 80% by the year 2010 (10). Recent polls by Internet watchdog
groups have found that nearly two out of three American adults have Internet
access, with more than 85% of those connected from home
(11-13).
The Internet has fast established itself as a leading source
for health information. It is still in its infancy, however, in how health information is accessed and used for
behavior change purposes.
Today, most Web-based health information exists in
a resource-list format. A health-related Web page
commonly consists of information with hyperlinks to other similar
or complementary information. The use of search engines and
portals categorizing information by topic provides users with
easy ways to gain access to health information. In addition,
numerous health-related behavior change approaches exist on the Internet,
from basic health-risk assessment to individual behavior change
approaches for challenges such as smoking cessation, albeit at basic levels of
generic and broad health messages (14,15). What is missing,
however, is the infusion of theoretical models and approaches,
especially those oriented toward behavior change,
for creating interactive and didactic communication systems that
access existing Internet-based health information. Efforts to use technology for impacting health behavior have been most prolific
in tailored health
communication.
Tailoring is a process for creating individualized communication. This paper does not delve into the merits or
shortcomings of tailored health communication, but rather explains how the eHealth
Behavior Management Model
fits within the broader ehealth behavior change movement. In tailored health
communication, user-provided personal data are used to determine the most
appropriate information or strategies for meeting the unique needs,
wants, and interests of each user. Technology has allowed tailored health communication
to proliferate, expanding the potential of this approach to meet the unique needs
of individuals (16,17). Researchers have applied
tailoring techniques to numerous behavioral issues, including
childhood immunization, weight loss, smoking cessation,
nutritional consumption, and sedentary behavior (18-22).
Tailored health communication relies on the ability to match
individual health needs with a set of predeveloped messages. Data management and
access become central issues in tailored health communication because of the
ability to address the unique needs of each
individual within the system. Managing large populations and
their needs requires software programs capable of sorting through
and matching appropriate messages with unique needs. The Internet
has extended the capability of tailored communication by providing
expanded and easy access to interactive assessment and delivery
of messages (16,17).
The main difference between tailored health
communication approaches and the eHealth Behavior Management Model is that while
the former creates messages for individuals based on assessed need or interest,
the latter matches behavior change messages with information that already exists on the Internet. The eHealth
Behavior Management Model assesses
individual need based on readiness-to-change behavior and matches
the individual to preselected Web sites. Although the eHealth Behavior Management
Model is still in the early stages of application,
initial findings suggest that it is a promising model for Internet-based
behavior change programming.
Back to top Overview of the eHealth Behavior Management Model
The eHealth Behavior Management Model uses
the theoretical underpinnings of two popular behavior change models, the
Transtheoretical Model and the behavioral intent aspect of the Theory of Planned
Behavior, as well as the concepts of
persuasive communication, to engage Internet users in a pseudocounseling
approach. A brief discussion of the key ideas behind these theories will help in understanding the eHealth
Behavior Management
Model.
The Transtheoretical Model is well known among behavioral
scientists and has been widely applied in efforts designed to
reduce the occurrence of a multitude of behaviors. This model provides practitioners with an
effective way to move individuals toward healthier lifestyles. Change is viewed
as a process that occurs over time, rather than an action that must occur as an
immediate and
direct result of an intervention. The Transtheoretical Model is based on the
premise that individuals are in one of five possible stages of change
associated with a particular behavior. Precontemplation is the
stage in which a person has no interest in changing the behavior.
Contemplation is when a person would like
to change the behavior someday but is not yet ready. Preparation is when a person is ready to make the change but needs
assistance in moving that want into reality. The more active
stages include Action and Maintenance. Those in Action have begun
the behavior change process. Key to their success is moving the
change to Maintenance, where change takes place over time
(23).
The behavioral intent aspect of the Theory of
Planned Behavior is based on the premise that individuals with a defined
intent toward change are more likely to engage in change,
especially individuals with an attitude that change is necessary. The premise also
includes the idea that the closer
the change relates to subjective norms, the greater
the likelihood that a sense of behavioral control exists (24). Central to this
theory is that beliefs about the behavior, control, and norms influence
attitude, subjective norms, and behavioral control. The theory suggests that creating a situation in
which intent is high will result in a greater likelihood that an individual will
carry
through with the intent.
The persuasive communication concepts of response dependence
and transactional interaction are key components of the eHealth Behavior Management
Model. Transactional communication involves
the flow of information between a persuader and a persuadee (25).
It is transactional because at least two parties are involved in
both sending and receiving information. To be persuasive,
communication must 1) motivate receivers to attend to messages, 2) solicit feedback from users, and
3) elaborate message
arguments to move individuals toward change. Current Internet
resources typically utilize a one-way communication mode:
information exists on a Web page and is accessed by a user.
Feedback loops — in which each party involved shares in the roles of sender and
receiver — do not usually exist in Internet health communication.
Response-dependent communication controls the flow of the
communication process, where responses to inquiries serve as the
basis for driving the next round of persuasive messages and
inquiries (25). Response-dependent communication is similar to
what may occur between a counselor and a client: questions are asked based on responses
to previously
asked questions. The response then becomes critical to the
direction in which the communication unfolds and can take many
forms, such as a question or a persuasive statement, rather than
simply an answer to a question.
The eHealth Behavior Management Model creates a persuasive
communication environment in which a user and a computer serve as
two parties in the communication stream. An underlying algorithm
controls the flow of
communication that results from transactions between the two parties (Figure 1).
The staging algorithm developed
for the eHealth Behavior Management Model was developed specifically for this
model and is based on approaches
previously used in numerous interventions using the Transtheoretical Model, but
it is yet to undergo a comprehensive validation study. The initial Web page in the
algorithm consists of a persuasive statement about the issue
followed by an opening question for the user. The user has the
option of selecting a response, which is typically
“yes,” “no,” “not really,” or
“sometimes,” by clicking on the appropriate response.
Subsequent Web pages in the algorithm contain empowering feedback
followed by an additional statement about the issue (persuasive
argument) and a subsequent question. The communication that
occurs between the user and the computer is transactional in that
give and take exists between both parties, and the communication is response-dependent
as well in that algorithm paths are followed according to responses and feedback.
Figure 1.
Algorithm for eHealth Behavior Management Model.
(A text description of this graphic is also available.)
The transactional, response-dependent communication continues
until the user arrives at a specific stage of readiness to change. The breadth of the popularity of
the Transtheoretical Model has culminated in numerous uses of staging algorithms
for myriad behaviors. A popular approach is to use a serious of
yes/no questions to determine current stage and the temporal
distance of the behavior, resulting in identification of a specific stage of
readiness to change (26-29). The questions used in the communication process
direct the user toward a specific stage of change (Figure
1). In essence, the model is acting as a diagnostic tool in
determining user stage of readiness to change. At this
point, the model directs the user to stage-based information
already existing on the Internet. These “end nodes”
contain information on the behavioral issue. Ideally, end nodes already exist on
the Web. All end nodes must be reviewed and approved by model designers for credibility and
appropriateness for stage of change and target population.
End-node assessment for stage of readiness to change as well
as processes of change that users typically undertake to move toward
more active stages are essential to this model because at this
point — within the end node — critical information on the user’s
need for change exists. A systematic four-step method is used by model designers to identify a pool of potential end nodes:
1) review and selection, based on known association and credibility, of Web sites linked
from resources on the behavior issue, such as the American Dietetic
Association, the U.S. Department of Agriculture, or university extension
services; 2) review of Web pages used in existing literature and other academic
sources; 3) solicitation of related end nodes from a panel of
expert reviewers; and 4) comprehensive search of the Internet
using the leading Internet search engines and techniques.
Potential end nodes are scrutinized using a five-step process
once the pool has been established. First, end nodes are reviewed
to determine their direct associations with the behavioral issues.
Suspect end nodes, including those that violate standards set by the U.S. Department of Health and Human Services Science Panel on
Interaction Communication in Health, are eliminated. Second,
end nodes are assessed for stage of readiness to change, based on
general criteria of the Transtheoretical Model. End
nodes that cross numerous stages are eliminated from the pool,
unless a mechanism exists within the Web page to direct users to information specific to the stage. Third, potential
end nodes are further matched against the specific concepts
associated with the behavioral issue. Fourth, potential end nodes
are assessed for the 10 processes of change associated with the Transtheoretical
Model, ensuring the process of change within the
end node is appropriate for both the concept associated with the
behavior and the stage of change itself. Finally, end nodes are
subjected to an expert panel for review and ranking, if more than
one end node exists for a specific behavioral concept. End nodes
that meet all five criteria are considered viable options for
the eHealth Behavior
Management Model.
Also central to the model is the ability to move forward in intent toward
change based on the stage-based information contained in the end node. The model
allows for recognition of this intent and will adjust users in the communication
stream to the next stage of readiness to change, providing users with the
opportunity to fortify intent even further (Figure 2). Users also have the
option of exiting from the model after reviewing stage-based end nodes. A
feedback loop in the model allows users to provide comments on what continues to
hold them back from moving forward in intent toward change; this feedback can
provide model designers with direction on end-node selection. In the nutrition
education program discussed in this paper, information on the beginning node, the
ending node, and the reasons for not progressing further in stage of
change are entered onto a certificate of completion, which is then
used by agency staff to further counsel clients toward additional
resources designed to aid in progress toward an active stage of
change.
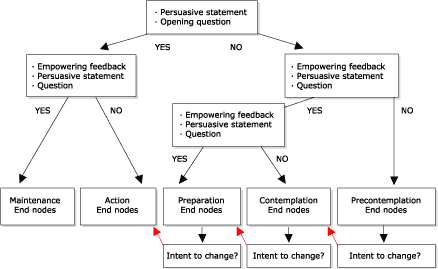
Figure 2.
Intent to change option of the eHealth Behavior
Management Model.
(A text description of this graphic is also available.)
Back to top
Application of the eHealth Behavior Management Model
The utility of the eHealth Behavior Management Model is
promising and may be applicable to a number of behavior
management issues, including behavior change, chronic disease
management, and disease prevention. Three demonstration projects
will be described to show how the model is currently being applied
to behavior management issues. The intent of this paper is to
provide examples of how the eHealth Behavior Management Model
has been adapted to fit behavior management and behavior change needs;
evaluative findings of the projects described below will be presented in the
future.
Women, Infants, and Children (WIC) nutrition educationNutrition education and nutrition counseling are vital
components of the U.S. Department of Agriculture WIC Program
(Special Supplemental Nutrition Program for Women, Infants, and
Children), accounting for 17% of state WIC operating expenses.
All WIC clients must be offered nutrition education, much of
which centers on parent-child feeding behaviors, as part of their
WIC participation. Traditional education methods, such as
one-on-one counseling, group education, classes, and printed
materials are typically used to provide this education.
Educational approaches are usually topic- or skill-based and
available to whomever may attend the WIC clinic on any particular
day. It is not feasible or routinely practiced to
segment audiences according to skills needed or stage of
readiness to change. Educational offerings may be divided by age
or type of participants (e.g., infants, toddlers, pregnant women,
breastfeeding women) but typically adhere to a one-size-fits-all educational approach given at the
Action stage of
change. Many WIC clients are unable to meet for traditional nutrition education
classes because of work or school schedules or transportation issues. In
addition, they may not attend classes because they may find that classes do
not meet their interests or needs, the educational materials offered are not
appropriate for them, or their available time is used in waiting for coupons to
be processed; if they do attend classes, they may be distracted by restless children. An incentive for completing secondary education
is the link between WIC contact and dispersion of food coupons.
While WIC benefits may not be withheld if a participant refuses
or cannot attend nutrition education, clinics usually schedule
nutrition education at the same time as coupon pickup to
encourage attendance.The need for more targeted stage-based educational
approaches led to the development of www.wichealth.org*, an
Internet-based parent-child feeding-behavior project based on the eHealth Behavior
Management Model. The project is in
its second year of implementation. To date, it has provided
stage-based secondary nutrition education to more than 30,000 WIC
participants in seven states. Five modules focus on providing regular meals and snacks, working with
picky eaters, providing a positive feeding environment, and outlining the
roles of parents and children in the feeding relationship. Nearly
70% of user access occurs from home or work, with an additional
16% occurring from parents’ or friends’ homes (30).
First- and second-year evaluations have consistently demonstrated high
levels of user satisfaction with the
helpfulness and ease of use of the site (84–99%), belief in
ability to make changes with what has been learned (87–90%), and
interest in using the Internet to learn about other WIC topics
(84–86%). Results also find the site to be popular with
participants in the more active stages of readiness to change
(Maintenance, Action, and Preparation), with significant movement
in intent toward Action in all modules where clients started in
earlier stages. Qualitative data support the quantitative
findings of this project (8,31).
All three theoretical underpinnings of the eHealth Behavior Management Model are inherent in www.wichealth.org*. The module
“Create
good eating habits in your child” will be used as an
example to depict how the eHealth model is applied to this
project. Once a user selects this module for learning, the staging process,
which uses persuasive communication
techniques, begins with a simple question. Users
in more active stages (Action-Maintenance path) are separated from those in earlier stages (Preparation-Contemplation-Precontemplation
path). Both options are response-dependent and include a persuasive empowering
statement and subsequent staging question, further defining the starting stage
of the user. Users who initially select less active stage options such as “We
don’t really eat together as a family” are further separated by stage with a
subsequent staging page. A positive response links to a page
(Preparation-Contemplation path) that uses a transactional and
response-dependent process to separate further Preparation and Contemplation
stages. A subsequent response such as “I am ready to start this week” identifies
the user as beginning in the Preparation stage. The system then provides a list
of topics and end-node links pertinent to processes of change for WIC
populations struggling with moving from Preparation to Action in child-feeding
environment issues. At this point, stage-based learning takes place. Users who
complete end-node review are then given the option of continuing to progress in
stage of change, based on behavioral intent, or exiting the system. Those who
intend to move forward enter the Action stage and have the option of learning
action-oriented skills from end nodes associated with this stage of readiness to
change. Those who choose to exit the system are provided with a certificate of
completion as evidence of successful completion of the module. Figure 3 depicts
the full staging algorithm, complete with response feedback (e.g.,
“Wonderful!”), empowering persuasive argument statements (e.g., “Creating a
focused eating environment helps children grow and develop normally”), and
subsequent staging question (e.g., “Are you ready to start doing this soon?”),
with the paths used in this example depicted in red. A review of the Web site
provides further perspective on how technical capabilities, such as frames and
links, stage users and move them toward active stages of readiness to change.
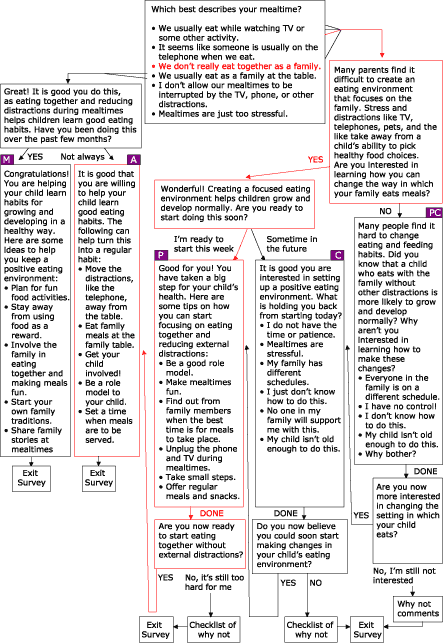
Figure 3.
Feeding-environment skills algorithm. PC = Precontemplation; C =
Contemplation; P = Preparation; A = Action; and M = Maintenance.
(A text description of this graphic is also available.)
Chronic disease management: Asthma Management Demonstration Project
According to the Centers for Disease Control and Prevention
(CDC), more than 20 million people in the United States have been
diagnosed with asthma, with 12 million of them experiencing uncontrolled asthma
(32). People diagnosed with asthma often accept a lower quality of life.
This lower quality of life includes missing days of work or
school, little or no participation in physical activity including
sports, regularly interrupted sleep, and overuse of
quick-relief medications.Despite an increase in data that elucidates the prevalence,
severity, and financial costs of uncontrolled or poorly managed
asthma, only a small amount of data describes the unique challenges
to asthma management in college or university settings. Colleges
and university settings require students and employees to
encounter myriad triggers of asthma. Those triggers include having little
control over living environments, including residence halls and
college apartments; sharing limited living space
with one or more roommates; changing
environments throughout the day because of classroom scheduling; and
managing exposure to outdoor pollens and molds created by the vast grounds-keeping
activities necessary for college campuses (e.g., mowing), to the prevalence of tobacco smoke
on college campuses, and
to fumes
emanating from chemistry labs, art studios, and physical
plants.
Many people living with asthma perceive asthma management to
be limited to symptom control. This perception is antithetical to
the goals of asthma management established by health educators
and medical professionals. In response, the Asthma
Management Demonstration Project was developed by the Office
of Health Promotion and Health Education at Western Michigan
University, with the purpose of managing behaviors and conditions
that lead to asthma-related consequences among employees and
students of Western Michigan University. Four modules based on
the eHealth Behavior Management model were created to address
the issues of asthma management: peak flow
monitoring, accessing asthma services, using prescription asthma medications
properly, and managing environmental
factors that trigger asthma attacks. Like the WIC nutrition education project,
four algorithms were created using empowering statements,
persuasive arguments, and transactional questioning to stage
users based on stage of readiness to change behavior. The modules are available
online from URL: http://www.wmich.edu/shc/HPAE/awp/homeset.html*. The underlying algorithms used for this project
are depicted below. Figure 4 shows the module on managing environmental triggers;
Figure 5 shows the module on accessing asthma services; Figure 6 shows the
module on using prescription drugs properly; and Figure 7 shows the module on
monitoring peak flow regularly.
The asthma project differs from the nutrition education project in the way that
algorithms link with one another. For example, in the module
“Managing Environmental Triggers,” initial questions determine if users
are actually ready to start managing triggers or if users need to focus first on accessing
medical care and using prescription asthma
medications properly, both of which are separate but linked modules within the
project (Figure 4).
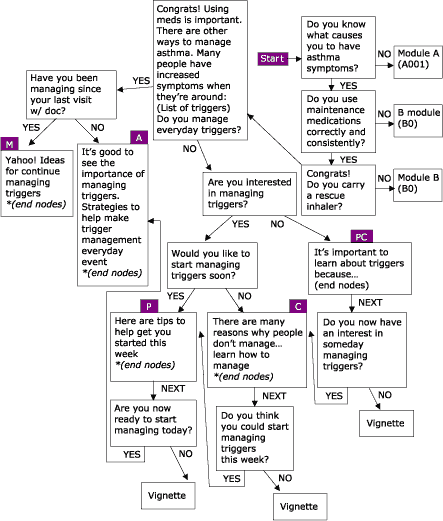
Figure 4.
Managing Environmental Triggers, one of four modules within the Asthma
Management Demonstration Project. PC = Precontemplation; C = Contemplation; P
= Preparation; A = Action; and M = Maintenance.
(A text description of this graphic is also available.)
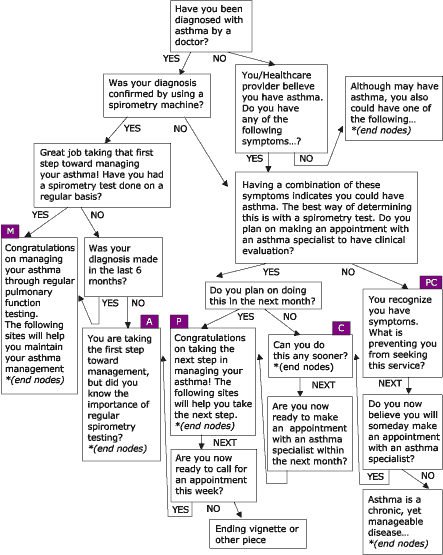
Figure 5.
Accessing Asthma Services, one of four modules within the Asthma Management
Demonstration Project. PC = Precontemplation; C = Contemplation; P =
Preparation; A = Action; and M = Maintenance.
(A text description of this graphic is also available.)
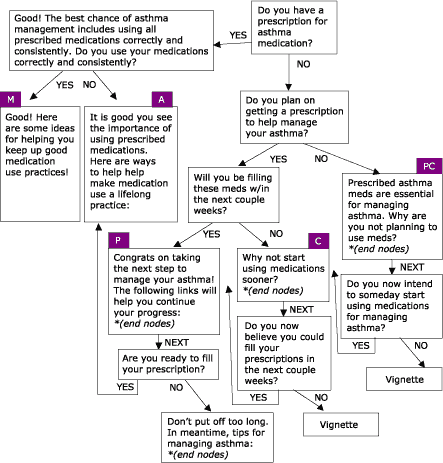
Figure 6.
Using Prescription Drugs Properly, one of four modules within the Asthma
Management Demonstration Project. PC = Precontemplation; C = Contemplation; P =
Preparation; A = Action; and M = Maintenance.
(A text description of this graphic is also available.)
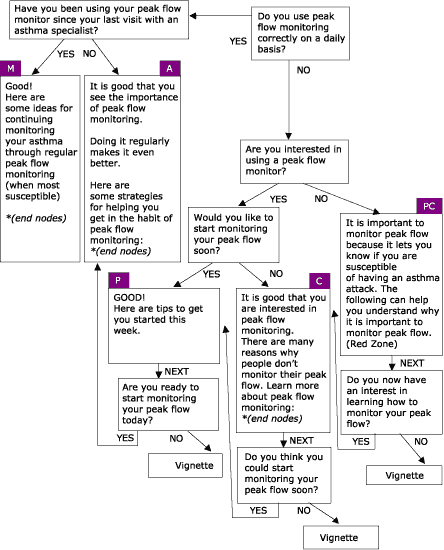
Figure 7.
Regular Peak Flow Monitoring, one of four modules within the Asthma
Management Demonstration Project. PC = Precontemplation; C = Contemplation; P =
Preparation; A = Action; and M = Maintenance.
(A text description of this graphic is also available.)
Two kiosks (stand-alone booths) placed in strategic locations on the
university campus serve as the mode for
delivering the asthma wellness education modules. Kiosks were chosen
and designed to maximize ease of use, ensure information
usefulness, and enhance user satisfaction with the educational
experience. SiteKiosk
database software
(Provisio, Muenster, Germany) was used to collect data based on user
responses and to send a secure e-mail transmission of the kiosk's daily
activities. Log files are downloaded from e-mails and then uploaded to a
database for analysis, which allows for a
deeper level of analysis of interactions between users and kiosks.
The Table presents preliminary data from 133 days of kiosk operation. Based on analysis of log files, it was
determined that at least 20 navigations within the Web site are
required to represent a quality use, which includes an initiating
navigation, navigation within the module pages, and navigation
into at least one end node within a module. During the 133 days analyzed, there were 220 total
quality uses with an average of 1.66 quality uses per day with
1.72 end-node visits per quality use. The module “Accessing Asthma Services” was
the most popular module accessed, likely due to a variety of reasons including
the broad nature of the topic and the location of the menu item (at the top of
the module selection page). Analysis of the actual path
each user completes as well as progress in intent toward stages of change will
be the purpose of final evaluation and analysis.
Preventing HIV through social-wellness building in South Africa
It is estimated 25 to 28 million of the 34 to 46 million
individuals living with human immunodeficiency virus/acquired immunodeficiency
syndrome (HIV/AIDS) live in sub-Saharan Africa (33).
It is further estimated that five million people living in South
Africa are infected with HIV, including 20% of individuals aged 15 to 49 years, representing one of the largest HIV-infected populations in
the world (34). The transmission of HIV/AIDS in South Africa is linked
primarily to sexual contact between opposite sexes. Women are at greater
risk of HIV because of physical and sexual violence, unequal
distribution of power among relationships between men and women resulting from male-dominated
cultures, migratory labor practices of male heads of households,
lack of access to relevant and accurate information about HIV/AIDS, and economic dependence of women
due to lack of economic
power (35-38).The eHealth Behavior Management Model is the basis
for an HIV/AIDS-prevention assertive-communication module currently being developed for South African women at the University of Port
Elizabeth, South Africa. Central to the project is the goal of
helping women to move toward more active behaviors associated
with open and assertive communication about
sexual relationships and practices. The empowering statements,
persuasive arguments, and transactional questions are now being pilot-tested for
validity, usability, and cultural translation with subsets of
women at the University of Port Elizabeth (Figure 8). Web design and applicability issues are also being addressed.
Figure 8. HIV/AIDS prevention assertive communication
module currently being developed for South African women at the University of
Port Elizabeth, South Africa.
(A text description of this graphic is also available.)
Many challenges exist in applying this model to a population
outside the United States, including different Internet practices and
accessibility issues and the lack of available and culturally
appropriate end nodes. Access to the Internet differs
dramatically from that in the United States, even though South Africa has
the highest availability of Internet access of any country in
Africa. Internet connection is especially lacking in rural South Africa;
high levels of poverty prevent South Africans from building the
infrastructure necessary for Internet connections; individuals
from populations at higher risk are often not computer-literate, and costs associated with per-minute connection to the
Internet proportionately far exceed costs found in
the United States. The major end-node barrier is the lack of existing Web
pages specific to South African cultures and languages. Most
existing Web pages are based in the United States, which limits the number of
appropriate end nodes. This project requires the development and
cultural adaptation of each end node, which in itself is a time-consuming process. Initial focus group results have
indicated
high interest in and acceptance of this Web-based assertive-communications
program as a viable method for behavior
change among the targeted population.
Back to top
Conclusion
The potential use of the eHealth Behavior Management Model is
both positive and broad, especially considering that the Internet
continues to be a viable avenue for health-related resources.
Expanded use of this model across other chronic disease
management issues, such as diabetes control, and across other
primary prevention issues, such as daily folic acid intake or
weight management, needs to occur to truly validate the extent to
which this model is applicable.
The benefits so far observed from implementation of the eHealth Behavior Management
Model are numerous. The behavior management and behavior change aspects of
this model are inherently evident. Early results have found the
model attracts people who are in the more active stages
of readiness to change (i.e., Preparation, Action, and
Maintenance). This may be because users who seek information from the Internet
are more likely to change or to be getting ready to change behaviors. This does
not discount the use of the model as a method within a comprehensive behavior
management or behavior change approach, but rather
suggests it may be an effective means for providing
change-related skills to a subset within a population at risk.
Equally important is the ability to use the model as a diagnostic
tool for identifying the stages that users are in and the issues in
which they are most interested. Being Web-based allows for data
collection and analysis of path movement, including specific end
nodes visited. Analyses of user traffic may provide program
planners with a greater understanding of the key issues that seem
to be of interest or have the greatest impact on preventing users
from progressing toward an active stage of change.
Internet-based approaches allow for reaching large numbers of people at
relatively low costs. The rapid increase in Internet use over the past decade attests to the expanding
interest in using the Internet as an avenue for
conveying health-related messages and skills to consumers. The eHealth Behavior
Management Model is built on providing better
and more appropriate access to this information. As with all
approaches, though, challenges do exist. The model directs users
to existing end nodes, and much time is required to maintain and
validate end-node links. Because end nodes are
maintained outside the control of the eHealth Behavior Management
Model, there is a greater likelihood that these external
sources information may not be available in the event of end-node host-server errors. Much of this uncertainty can be avoided through
reciprocal communication with the end-node site owners,
contingency plans for replacing end nodes in the event of
failure, and weekly or daily monitoring of end-node
functioning.
Use of predetermined end nodes deviates from more
traditional tailored communication approaches, decreasing the
ability to direct users to tailored messages based on user-interactive input. The trade-off is the benefit
of the breadth of potential existing end nodes and the lower costs
compared to those of developing computer-based expert systems. When used in
conjunction with other forms of behavior change management, such as follow-up health
counseling, the eHealth Behavior Management Model can play an
important role in initiating client movement along the stages-of-change continuum.
The usefulness and impact of this model are currently under investigation, with initial results showing the eHealth
Behavior Management Model to be both useful and effective
with intent toward health behavior change. It is recommended this
model be adopted to and evaluated with other health
behavior management and change issues.
Back to top
Acknowledgments
www.wichealth.org* is funded in part by the Midwest WIC Region of
the U.S. Department of Agriculture Food and Nutrition
Service’s Special Supplemental Nutrition Program for Women,
Infants, and Children and the Washington State Department of
Health WIC Programs Division.
The Asthma Management Demonstration Project is funded in part by the
Western Michigan University Health Management Group.
Back to top
Author Information
Corresponding Author: Robert J. Bensley, PhD, Western Michigan
University, 4024 SRC/Department of HPER, Kalamazoo, MI 49008.
Telephone: 269-387-3081. E-mail: robert.bensley@wmich.edu.
Author Affiliations: Nelda Mercer, MS, Judith Anderson, DrPH, Deanne
Kelleher, MS, Michigan
Department of Community Health, Lansing, Mich; John J. Brusk, MPH, Ric Underhile,
PhD, Jason Rivas, Western
Michigan University, Kalamazoo, Mich; Melissa Lupella, MPH, University of Illinois-Chicago,
Chicago, Ill; André C. de Jager, DPhil, University of Port Elizabeth, Port
Elizabeth, South Africa.
Back to top
References
- Lalonde M. A new perspective on the health of
Canadians: a working document. Ottawa (ON): Government of Canada;
1974.
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL.
Actual causes of death in the United States, 2000. JAMA.
2004;291(10):1238-45.
- Prochaska JO, DiClemente CC.
Stages and
processes of self-change of smoking: toward an integrative model
of change. J Consult Clin Psychol 1983;51(3):390-5.
- Bensley RJ. Developing Internet-based learning
modules. In: Bensley RJ, Brookins-Fisher J, editors. Community
health education methods: a practical guide.
2nd ed. Sudbury (MA): Jones and Bartlett Publishers;
2003.
- Metamend. How big is the Internet? How fast is
the Internet growing [Internet]? Victoria, British Columbia (Canada): Metamend
Software & Design Ltd [cited 2004 May 19]; 2004. Available from: URL: http://www.metamend.com/internet-growth.html*.
- Nua Internet Surveys. How many online [Internet]? Darien (CT):
Jupitermedia Corporation [cited 2004 May 19]; 2002. Available from: URL: http://www.nua.ie/surveys/how_many_online*.
- Pew Internet & American Life Project. Older
Americans and the Internet [Internet]. Washington (DC): Pew Internet & American
Life Project [cited 2004 May 19]; 2004 Mar 28.
Available from: URL: http://www.pewinternet.org/reports/toc.asp?Report=117*.
- Bensley RJ, Underhile R, de Jager AC, Bettin K,
Mercer N, Brusk JS. Application of the eHealth Behavior Change
and Management Model. Annual meeting of the American Public
Health Association; San Francisco (CA): 2003 Nov 15-19.
- Billing AS, Atkinson NL, Gold R. Assessing the needs of food stamp
recipients in five Maryland counties. Annual meeting of the American
Public Health Association; San Francisco (CA): 2003 Nov 15-19.
- U.S. Department of Health and Human Services.
Healthy people 2010: understanding and improving health. Washington (DC): U.S.
Government Printing Office; 2000.
- Pew Internet & American Life Project.
America’s online pursuits: the changing picture of
who’s online and what they do [Internet]. Washington (DC): Pew Internet &
American Life Project [cited 2004 May 19]; 2003 Dec 22. Available from:
URL: http://www.pewinternet.org/reports/toc.asp?Report=106*.
- Taylor H. Those with Internet access to continue to
grow but at a slower rate [Internet]. Rochester (NY): Harris Interactive [cited
2004 May 19]; 2003. Available
from: URL: http://www.harrisinteractive.com/harris_poll/ index.asp?PID=356*.
- Taylor H. Internet penetration at 66% of adults (137
million) nationwide [Internet]. Rochester (NY): Harris Interactive [cited 2004
May 19]; 2002. Available from: URL: http://www.harrisinteractive.com/harris_poll/ index.asp?PID=295*.
- Bock B, Graham A, Sciamanna C, Krishnamoorthy J,
Whiteley J, Carmona-Barros R, et al.
Smoking
cessation treatment on the Internet: content, quality, and
usability. Nicotine Tob Res
2004;6(2):207-19.
- Bensley RJ, Lewis J. Analysis of Internet-based
health assessments. Health Promot Pract 2002;3(4):463-76.
- Kreuter M, Farrell D, Olevitch L, Brennan L.
Tailoring health messages: customizing communication with
computer technology. Mahwah (NJ): Lawrence Erlbaum Associates;
1999.
- Kreuter MW, Jacobsen HA, McDonald EM, Carlson-Gielen
A. Developing computerized tailored health messages. In: Bensley
RJ, Brookins-Fisher J, editors. Community health education
methods: a practical guide. 2nd ed. Sudbury (MA): Jones and Bartlett Publishers; 2003.
- Kreuter M, Vehige E, McGuire AG.
Using
computer-tailored calendars to promote childhood immunization.
Public Health Rep 1996;111(2):176-8.
- Kreuter M, Bull F, Clark E, Oswald D.
Understanding
how people process health information: a comparison of tailored
and untailored weight loss materials. Health Psychol
1999;18(5):487-94.
- Rimer BK, Orleans CT, Fleisher L, Cristinzio S,
Resch N, Telepchak J, et al.
Does tailoring matter? The impact of
a tailored guide on ratings and short-term smoking-related
outcomes for older smokers. Health Educ Q 1994;9(1):69-84.
- Rimer BK, Orleans CT.
Tailoring smoking cessation
for older adults. Cancer 1994;74(7 Suppl):2051-4.
- Strecher V, Wang C, Derry H, Wildenhaus K,
Johnson C.
Tailored interventions for multiple risk behaviors.
Health Educ Res 2002 Oct;17(5):619-26.
- Velicer WF, Prochaska JO, Fava JL, Norman GJ,
Redding CA. Smoking cessation and stress management: applications
of the Transtheoretical Model of behavior change. Homeostasis
1998;38:216-33.
- Ajzen I. Theory of planned behavior [Internet]. Amherst (MA):
University of Massachusetts Amherst [cited 2004 May 19];2002. Available from: http://www.people.umass.edu/aizen/tpb.html*.
- Cassell MM, Jackson C, Cheuvront B.
Health
communication on the Internet: an effective channel for health
behavior change? J Health Commun 1998;3(1):71-9.
- Reed GR, Velicer WF, Prochaska JO.
What makes a good
staging algorithm: examples from regular exercise. Am J Health Promot 1997;12(1):57-66.
- DiClemente CC, Prochaska JO, Fairhurst S,
Velicer WF, Rossi JS, Velasquez M.
The process of smoking
cessation: an analysis of precontemplation, contemplation and
contemplation/action. J Consult Clin Psychol
1991;59(2):295-304.
- Velicer WF, Fava JL, Prochaska JO, Abrams DB, Emmons
KM, Pierce J.
Distribution of smokers by stage in three
representative samples. Prev Med 1995;24(4):401-11.
- Vallis M, Ruggiero L, Greene G, Jones H, Zinman B, Rossi S, et al.
Stages of change for
healthy eating in diabetes: relation to demographic,
eating-related, health care utilization, and psychosocial
factors. Diabetes Care 2003 May;26(5):1468-74.
- Brusk JS, Bensley RJ. Midyear evaluation report 2003-2004 [Internet].
Kalamazoo (MI): Western Michigan University; 2004. Available from: URL:
http://www.wichealth.org*.
- Bensley RJ. Nutrition education on the Internet.
Annual meeting of the National WIC Association. Anaheim (CA): 2004
Apr 26.
- Centers for Disease Control and Prevention.
Behavioral Risk Factor Surveillance System Survey Data. Atlanta (GA): U.S. Department of Health and Human Services; 2002.
- World Health Organization.
AIDS epidemic update:
December 2003 [Internet]. Geneva (Switzerland): World Health Organization [cited 2004 May 24];
2003.
- USAID.
Country Profile: HIV/AIDS South Africa [Internet]. Washington
(DC): USAID [cited 2004 May 24]; 2004. Available from:
http://www.usaid.gov/our_work/global_health/aids/ Countries/africa/safricabrief.pdf.
- Dunkle KL, Jewkes RK, Brown HC, Gray GE, McIntryre
JA, Harlow SD.
Gender-based violence, relationship power, and
risk of HIV infection in women attending antenatal clinics in
South Africa. Lancet 2004;363(9419):1415-21.
- Gilbert L, Walker L.
Treading the path of least
resistance: HIV/AIDS and social inequalities — a South
African case study. Soc Sci Med 2002;54(7):1093-110.
- Health24. Women’s vulnerability to HIV
infection [Internet]. Cape Town (South Africa): AfroAIDSinfo [cited 2004 May 24];
2003. Available from: URL:
http://www.afroaidsinfo.org/content/hivandyou/ HivAffectAdults/womens.htm*.
- Lurie MN, Williams BG, Zuma K, Mkaya-Mwamburi D, Garnett G, Sturm AW, et al.
The impact of
migration on HIV-1 transmission in South Africa: a study of migrant and nonmigrant men and their partners. Sex Transm Dis
2003;30(2):149-56.
Back to top
Table
 Preliminary Asthma Management Demonstration Project Usage Statistics, Sept
26, 2003–Apr 5, 2004, Kalamazoo, Mich Preliminary Asthma Management Demonstration Project Usage Statistics, Sept
26, 2003–Apr 5, 2004, Kalamazoo, Mich
|
Total navigations
|
4404
|
|
Average navigations per day
|
33.1
|
|
Days of data collection
|
133
|
|
Module A-related navigations
|
868
|
|
Module B-related navigations
|
575
|
|
Module C-related navigations
|
306
|
|
Module D-related navigations
|
453
|
|
End nodes accessed
|
379
|
|
Estimated quality uses
|
220.2
|
|
End nodes accessed per quality use |
1.7
|
|
Estimated quality uses per day
|
1.7 |
|

Back to top
*URLs for nonfederal organizations are provided solely as a
service to our users. URLs do not constitute an endorsement of any organization
by CDC or the federal government, and none should be inferred. CDC is
not responsible for the content of Web pages found at these URLs.
|
|
