 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Syndromic Surveillance at Hospital Emergency Departments --- Southeastern VirginiaChristine M. Yuan,1,3 S. Love,2
M. Wilson1
Corresponding author: Christine M. Yuan, Bureau of Epidemiology and Health Risk Assessment, District of Columbia Department of Health, 825 North Capitol St. NE, Third Floor, Washington, D.C., 20002. Telephone: 202-442-5859; Fax: 202-442-4796; E-mail: christine.yuan@dc.gov. AbstractHospital emergency department (ED) syndromic surveillance has been proposed for early detection of a large-scale biologic terrorist attack. However, questions remain regarding its usefulness. The authors examined the use of active syndromic surveillance at hospital EDs in Virginia for early detection of disease events and analyzed the effectiveness of the cumulative sum (CUSUM) algorithm in identifying disease events from syndromic data. Daily chief-complaint data were collected for 10 months at seven hospital EDs in southeastern Virginia. Data were categorized into seven syndromes (fever, respiratory distress, vomiting, diarrhea, rash, disorientation, and sepsis), and the CUSUM algorithm was used to detect anomalies in each of the seven syndromes at each hospital. Fever and respiratory distress syndromes exhibited monthly and ambient-temperature--specific trends consistent with southeastern Virginia's influenza season. Furthermore, preliminary frequencies of hospital ED patient chief complaints in southeastern Virginia during a 10-month period were produced by using syndromic data. This system represents an example of a local syndromic surveillance program serving multiple cities in a limited geographic region. IntroductionSyndromic surveillance in hospital emergency departments (EDs) involves monitoring incoming patients with nonspecific syndromes to determine whether an unusual excess of any group of symptoms exists. Although syndromic surveillance might prove useful for detecting a deliberate release of a biologic agent, baseline ED chief-complaint data first need to be better characterized to create a surveillance instrument that can detect unusual disease incidence of any cause (1,2). Lives might be lost if an untested surveillance system misses a disease event (3). Therefore, syndromic surveillance systems should be investigated critically to determine whether ED data can serve these purposes. Accordingly, syndromic surveillance was performed at seven hospital EDs in southeastern Virginia, and the value of ED-based syndromic surveillance was explored by analyzing the effectiveness of the cumulative sum (CUSUM) algorithm for detecting unusual disease events. Syndromic Surveillance SystemPopulationThe Tidewater or Hampton Roads region of southeastern Virginia has a substantial military presence, consisting of a major U.S. Air Force base and a naval amphibious base. Approximately 13% of the population of the four Virginia cities from which data were collected (Norfolk, Chesapeake, Newport News, and Virginia Beach) were either in reserve or on active military duty in the year 2000 (4). In addition, the military is responsible for approximately 25% of the region's economy (5). The syndromic surveillance system established in this region involved seven civilian hospitals serving approximately 1 million residents (6). Data Collection and Aberration DetectionED data were collected from seven hospitals during September 2001--June 2002. Chief-complaint data (i.e., the patient's stated reason for visiting the ED) were faxed daily from hospitals to the health department. These data were then categorized manually into one of seven syndromes (fever, respiratory distress, vomiting, diarrhea, rash, disorientation, and sepsis). A CUSUM algorithm (7) was used to analyze unusual increases in each of the seven syndromes at each hospital. The CUSUM algorithm used three different moving average calculations (mild, medium, and ultra) to identify unusually high occurrences of each syndrome. The mild calculation used a moving average of syndrome counts for the 7 days preceding the ED visit. The moving average for the medium calculation was for 3--9 days previous, and the moving average for the ultra calculation was for 3 preceding days. Upper limits for all three calculations were set to the moving average plus 3 standard deviations, and observed daily syndrome counts were compared with each upper limit. A working database was created for the Tidewater region that combined daily entry of syndrome counts with the CUSUM anomaly-detection algorithm. Daily syndrome counts were dichotomized as high occurrence or low occurrence on the basis of daily CUSUM calculations. On high occurrence days, the health department performed patient chart reviews and reported information on patient ED visits (e.g, discharge diagnosis, laboratory testing, and patient disposition) to the regional epidemiologist. Monthly reports were also generated on syndrome counts and distributed to participating hospitals' infection-control practitioners, personnel involved in emergency response to biologic terrorism, and ED personnel. Detection of InfluenzaThe CUSUM algorithm detected trends in fever and respiratory distress occurrences indicative of influenza at hospital C (Figure 1) and by month and temperature (Figure 2). According to the sentinel influenza surveillance system, which consists of a designated group of reporting physicians in the region, influenza occurrence in eastern Virginia increased during the week of January 23, 2002. However, syndromic data on fever and respiratory distress revealed an increase in these two syndromes during the week of January 14, 2002, indicating an earlier start to the influenza season. ExperienceChallengesSyndromic surveillance presented certain challenges. The collected data spanned only a 10-month period that included both a biologic terrorist event involving anthrax in a nearby region as well as an influenza season. Thus, syndromic data might have reflected both seasonally expected trends and unexpected syndrome occurrences. Moreover, the lack of an electronic method for rapid and accurate data transfer often delayed the collection process. Syndromic surveillance retrospectively detected disease occurrences (e.g., the influenza season); however, without timely data reporting, acute disease events might not be detected quickly enough to permit rapid response. Extrinsic ValueDespite certain difficulties, a preliminary characterization of hospital ED populations and syndrome occurrences in the Tidewater region was produced, the first such effort in southeastern Virginia. Because syndromic surveillance has only recently been introduced into public health, patterns from different surveillance systems have rarely been compared. This surveillance system compared seven different hospitals and syndromes and identified substantial pattern differences in two syndromes at only one hospital. This indicates that recognizing anomalies in any one place and for any one syndrome might require analysis of local circumstances (e.g., the populations served by particular hospitals) to enhance syndromic surveillance and improve detection of the unusual. The CUSUM algorithm identified increased influenza activity (i.e., respiratory distress and fever). With refinement and longer time series, CUSUM should become more sensitive and eventually be able to provide earlier recognition of natural outbreaks or terrorist events. Intrinsic ValueSyndromic surveillance can increase communication among professionals in public health and clinical medicine. Through greater interaction between the public health and medical fields, ED physicians and other health-care personnel realize the value of a public health specialist (8). Furthermore, partnering of public health professionals with physicians, law enforcement and other disaster-management workers can improve a jurisdiction's preparedness for any disease event (9). The effectiveness of a surveillance system requires the cooperation and collaboration of multiple persons. As part of syndromic surveillance, EDs might capture sudden, subtle changes in the magnitude and distribution of diseases in a population (8). Meanwhile, public heath departments are responsible for continuously monitoring surveillance reports and findings (1). For syndromic surveillance to enhance rapid detection of anomalous events, clear communication among hospitals and public health agencies, as well as preparedness and response capacities, must be in place. AcknowledgementsJ. Davies-Cole, C. Glymph, and A. Diallo of the District of Columbia Department of Health provided guidance and support. Reviewers also provided invaluable comments and suggestions. References
Figure 1 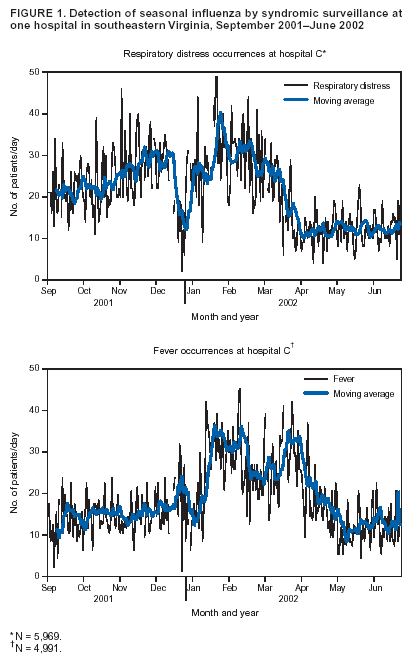 Return to top. Figure 2 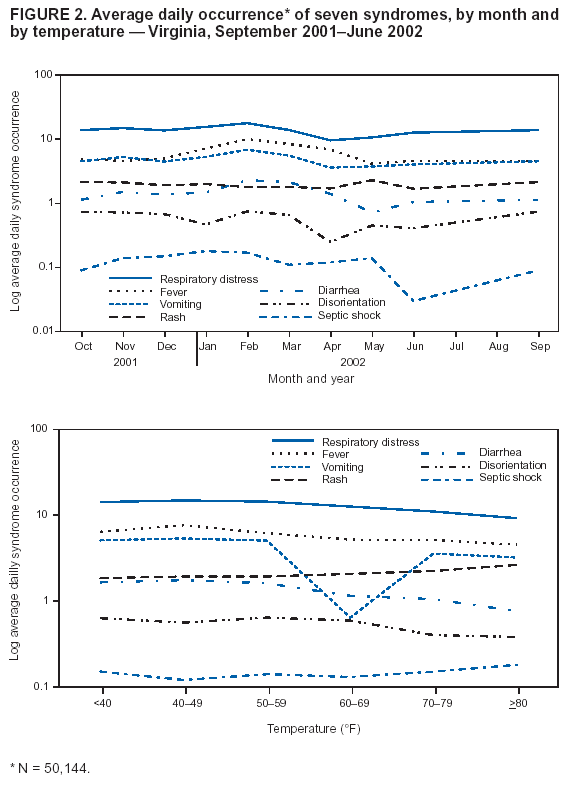 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 9/14/2004 |
|||||||||
This page last reviewed 9/14/2004
|