Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail.
Paul Coverdell National Acute Stroke Registry Surveillance --- Four States, 2005--2007
Abstract
Problem/Condition: Each year, approximately 795,000 persons in the United States experience a new or recurrent stroke. Data from the prototype phase (2001--2004) of the Paul Coverdell National Acute Stroke Registry (PCNASR) suggested that numerous acute stroke patients did not receive treatment according to established guidelines.
Reporting Period: This report summarizes PCNASR data collected during 2005--2007 from Georgia, Illinois, Massachusetts, and North Carolina, the first states to have PCNASRs implemented in and led by state health departments.
Description of System: PCNASR was established by CDC in 2001 to track and improve the quality of hospital-based acute stroke care. The prototype phase (2001--2004) registries were led by CDC-funded clinical investigators in academic and medical institutions, whereas the full implementation of the 2005--2007 statewide registries was led by CDC-funded state health departments. Health departments in each state recruit hospitals to collect data. To be included in PCNASR, patients must be aged ≥18 years and have a clinical diagnosis of acute ischemic stroke, intracerebral hemorrhage, subarachnoid hemorrhage, or transient ischemic attack (TIA) or an International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code indicative of a stroke or TIA. Data for patients who are already hospitalized at the time of stroke are not included. The following 10 performance measures of care, based on established guidelines for care of acute stroke patients, were developed by CDC in partnership with neurologists who specialize in stroke care: 1) received deep venous thrombosis prophylaxis, 2) received antithrombotic therapy at discharge, 3) received anticoagulation therapy for atrial fibrillation, 4) received tissue plasminogen activator (among eligible patients), 5) received antithrombotic therapy within 48 hours of admission or by the end of the second hospital day, 6) received lipid level testing, 7) received dysphagia screening, 8) received stroke education, 9) received smoking cessation counseling, and 10) received assessment for rehabilitation services. Adherence to these performance measures of care was calculated using predefined inclusion and exclusion criteria.
Results: A total of 195 hospitals from Georgia, Illinois, Massachusetts, and North Carolina contributed data to PCNASR during 2005--2007, representing 56,969 patients. Approximately half (53.3%) the cases of stroke in the registry occurred among females. A total of 2.5% of cases were among Hispanics; however, the proportion varied significantly by state. Cases among black patients ranged from 5.6% in Massachusetts to 35.8% in Georgia. The age at which patients experienced stroke varied significantly by state. On average, patients were oldest in Massachusetts (median age: 77 years) and youngest in Georgia (median age: 67 years). Overall, the clinical diagnosis for registry stroke cases was hemorrhagic stroke (13.8% of cases), ischemic stroke (56.2%), ill-defined stroke (i.e., medical record did not specify ischemic or hemorrhagic stroke; 7.3%), and TIA (21.6%). A total of 18.5% of patients with stroke symptoms arrived at the hospital within 2 hours of symptom onset; however, the time from onset of symptoms to hospital arrival was not recorded or was not known for the majority (57.8%) of patients. Of the 56,969 patients, 47.6% were transported by emergency medical services (EMS) from the scene of symptom onset, 11.1% were transferred by EMS from another hospital, and 39.4% used private or other transportation. Adherence to acute stroke care measures defined by PCNASR were as follows: received antithrombotic therapy at discharge (97.6%), received antithrombotic therapy within 48 hours of admission or by the end of the second hospital day (94.6%), assessed for rehabilitation services (90.1%), received deep venous thrombosis prophylaxis (85.5%), received anticoagulation therapy for atrial fibrillation (82.5%), received smoking cessation counseling (78.6%), received lipid level testing (69.9%), received stroke education (58.8%), received dysphagia screening (56.7%), and received tissue plasminogen activator (among eligible patients) (39.8%).
Interpretation: Between 2001--2004 (prototype phase) and 2005--2007 (implementation by state health departments), substantial improvement occurred in dysphagia screening, lipid testing, smoking cessation counseling, and antithrombotic therapy prescribed at discharge. These initial improvements indicate that a surveillance system to track and improve the quality of hospital-based stroke care can be led successfully by state health departments, although further evaluations over time are needed. Despite these improvements, additional increases are needed in adherence to these and other performance measures. Nearly 40% of stroke patients did not use EMS services for transport to hospitals, and no change occurred in the proportion of patients who arrived at the hospital in time to receive thrombolytic therapy for ischemic stroke. Patients who are not promptly transported to hospitals after symptom onset are ineligible for thrombolytic therapy and other timely interventions for acute stroke.
Public Health Actions: Results from PCNASR indicate the need for additional public health measures to inform the public of the need for timely activation of EMS services for signs and symptoms of stroke. In addition, low rates of adherence to certain measures of stroke care underscore the need for continuing coordinated programs to improve stroke quality of care. Additional analyses are needed to assess improvements in adherence to guidelines over time.
Introduction
Each year, approximately 795,000 persons in the United States experience a stroke; approximately 610,000 of these are first-time strokes, and the remaining are recurrent strokes (1). In 2001, Congress provided funding to CDC to establish the Paul Coverdell National Acute Stroke Registry (PCNASR) to monitor and improve the quality of care for stroke patients through assessment of adherence to established performance measures for acute stroke care (2). PCNASR regularly monitors for racial/ethnic, sex, and geographic disparities in stroke care and works with states to eliminate these disparities in care, as well as to decrease the rate of premature death and disability from acute stroke through prevention of recurrent disease and increased public awareness of stroke treatment and prevention.
During 2001--2004 (the prototype phase), CDC funded eight PCNASR prototype registries, which were led by academic principal investigators and medical institutions, to collect data on the quality of care provided to stroke patients from the initial emergency response through hospital discharge. This prototype phase was used to determine how best to develop stroke quality improvement registries, identify which data elements could and should be collected, and identify challenges involved in data collection. Four registries began receiving funding in 2001 (implemented by clinical investigators in Georgia, Massachusetts, Michigan, and Ohio), and four in 2002 (implemented by clinical investigators in California, Illinois, North Carolina, and Oregon).
Results from the prototype phase of PCNASR indicated that many acute stroke patients were not receiving treatments recommended in established guidelines (3). For example, one of the acute stroke care measures defined by PCNASR recommends that eligible patients with acute ischemic stroke who arrive at the hospital within 2 hours of onset of stroke signs and symptoms receive intravenous (IV) tissue plasminogen activator (tPA), a thrombolytic agent, within 3 hours of onset. Data from the North Carolina Stroke Care Collaborative, a CDC-funded PCNASR, indicated that among persons who either experienced or had a witnessed a stroke and knew the time of stroke onset, less than half (38%) arrived at the hospital within 2 hours of symptom onset; thus, few patients for whom tPA might have been indicated arrived in time to receive the treatment (4). Intravenous tPA is the only treatment approved by the Food and Drug Administration for use with ischemic stroke patients and is only approved for use within 3 hours of symptom onset (5). Patients treated with tPA are 30%--50% more likely to have good functional outcomes than those who do not receive tPA (6,7).
A CT scan is a crucial component of optimal stroke care for all stroke patients. The National Institutes of Neurological Disorders and Stroke recommends that stroke patients receive an initial CT scan within 25 minutes of hospital arrival (8). A study of the North Carolina PCNASR program (the North Carolina Stroke Care Collaborative) indicated that 23% of stroke patients who arrived within 2 hours of symptom onset received a CT scan within 25 minutes (median: 42 minutes) (5). In that study, prehospital delays and mode of arrival were the strongest predictors of a longer time between hospital arrival and initial CT scan. Arriving at the hospital by emergency medical systems (EMS) was associated with a shorter time between hospital arrival and initial CT scan.
Timely receipt of appropriate treatments for stroke requires prompt recognition of stroke signs and symptoms and activation of EMS. The five major signs and symptoms of stroke include 1) sudden severe headache; 2) sudden loss of vision in one or both eyes; 3) sudden weakness in an arm, a leg, or the face; 4) sudden confusion, trouble speaking, or understanding; and 5) sudden trouble walking, dizziness, or loss of balance or coordination. Awareness of these signs and symptoms ranged from 34.4% to 55.7% among respondents to the 2005 Behavioral Risk Factor Surveillance System survey from 13 states and the District of Columbia (9).
Data from hospital-based registries that track quality of stroke care can be used by state health departments to guide hospital quality improvement interventions through partnerships with hospital staff members and state-based stroke councils. Based on results from the prototype phase, PCNASR data elements and performance measures were refined. In 2004, CDC provided initial funding to state health departments in Georgia, Illinois, Massachusetts, and North Carolina to implement PCNASRs and begin collecting data in 2005. This initial report summarizes 2005--2007 PCNASR data from these four state stroke registries, which are the first PCNASRs to be implemented and led by state health departments.
Methods
PCNASR is funded by CDC through a cooperative agreement between CDC and state health departments. Any state with a CDC-funded heart disease and stroke prevention program (which, in 2004, included 32 states and the District of Columbia) was eligible to apply for participation through a competitive application process. An objective review process based on criteria established in the PCNASR request for application was used to fund four states to collect data during 2005--2007 (Georgia, Illinois, Massachusetts, and North Carolina), in accordance with Department of Health and Human Services grants policy directives. CDC provides technical assistance to funded states for all aspects of PCNASR, and state health departments provide technical assistance to PCNASR hospitals (i.e., provide educational programs for stroke care teams and assist with improving data quality and with quality improvement challenges).
Hospital Recruitment and Selection
Each state developed a strategy to recruit hospitals for the registry. Participation in the registry is voluntary; therefore, not all selected hospitals participated. In addition, all hospitals that were not specifically recruited or selected as part of a random sample but that individually volunteered to participate also were included in the registry (i.e., nonsample hospitals). Hospitals that collected data but subsequently withdrew from the registry were included in the analysis.
Georgia
To maintain registry continuity, the Georgia Division of Public Health chose the same hospitals that participated in the prototype phase to participate in the 2005--2007 registry. For the prototype phase, of the 151 non-Veterans Affairs (non-VA) acute care or critical-access hospitals* with at least one admission for acute stroke in Georgia during 2000, a total of 60 hospitals were selected to participate; 52 hospitals were selected from a random sample, and eight additional hospitals were selected from the county with the most annual acute stroke admissions. Of the 60 hospitals that participated in the prototype phase, three hospitals had gone out of business or merged with other hospitals. In November 2005, 19 (33%) of the random sample hospitals and seven nonsample hospitals were participating in the registry. In September 2006, an additional 20 sample hospitals and five nonsample hospitals began participating. Two additional nonsample hospitals volunteered to participate in December 2006 and March 2007, for a total of 53 hospitals (39 sample hospitals [68% of sample] and 14 nonsample hospitals) participating in the registry. Admission for stroke to these hospitals represented approximately 57% of stroke admissions in the state based on 2005 hospital discharge data (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] codes 430--438). During April 2007--December 2007, 11 sample hospitals withdrew from the registry at various times. No nonsample hospitals withdrew.
Illinois
Illinois developed a sampling design based on experience gained with the PCNASR prototype registry. For the prototype, a stratified random sample design was used to identify potential hospitals for registry participation. Before selection, all Illinois hospitals were stratified by Illinois Department of Public Health (IDPH) regions (Champaign, Chicago, Edwardsville, Marion, Peoria, Rockford, and West Chicago) and by size based on the annual number of stroke admissions in 2001 (small, 50--200 stroke admissions; medium, 200--400 stroke admissions; large, >400 stroke admissions). IDPH attempted to choose equal numbers of small, medium, and large hospitals; hospitals were randomly selected within size strata from each region. Nineteen hospitals that participated in the PCNASR prototype registry also were invited to participate. In 2005, 22 hospitals (18 sample hospitals and four nonsample hospitals from the prototype registry) were recruited (group 1). The same sample design was used to identify additional hospitals in the following years. Twenty hospitals were recruited from a random sample in 2006 (group 2), and three hospitals were recruited in 2007 (group 3). Of the total 142 non-VA acute-care eligible hospitals in Illinois, 45 hospitals participated in the registry at various points during 2005--2007. Two hospitals in group 1 withdrew at various times after 1 year of participation; eight hospitals in group 1 withdrew at the end of May 2007. Admission for stroke to the 45 registry hospitals represented approximately 40% of stroke admissions in the state based on 2004 hospital discharge data (ICD-9-CM codes 430--438).
Massachusetts
In 2004, the Massachusetts Department of Public Health issued licensure regulations for hospital designation as a primary stroke service (PSS) hospital. PSS hospitals must have written, guideline-based protocols for acute stroke care; the ability to meet time goals for assessment, management, and treatment of acute stroke for patients who arrive within 3 hours of symptom onset; and the capacity to provide thrombolytic therapy, brain imaging (i.e., computed tomography [CT] and magnetic resonance imaging [MRI]), laboratory services, and neurologic services at all times. In Massachusetts, only PSS hospitals (69 of Massachusetts' 72 hospitals) are allowed to treat acute stroke patients; therefore, the Massachusetts Department of Public Health only recruited PSS hospitals to participate in the registry; no VA hospitals participated. Hospitals joined the registry in three groups: 36 hospitals (group 1) in June 2005, 16 hospitals (group 2) in January 2006, and five hospitals (group 3) in January 2007. One hospital withdrew in 2007. As of December 2007, 56 of the 69 PSS hospitals were participating in the Massachusetts PCNASR. Admission for stroke to the 56 participating hospitals represented 83% of stroke admissions in the state based on 2005 hospital discharge data (ICD-9-CM codes 430--438).
North Carolina
In North Carolina, hospitals eligible for participation in the registry included all non-VA hospitals that had a dedicated emergency department (ED) as defined by the Centers for Medicare & Medicaid Services (CMS). Critical-access hospitals were eligible to participate if they had a dedicated ED. A total of 110 hospitals met the eligibility criteria. The North Carolina registry program did not limit the number of hospitals that could submit a request to participate, which increased the likelihood of establishing registries at hospitals in all geographic regions of the state. In May 2005, 13 hospitals began participating. Additional hospitals joined the registry during May 2005--December 2007; 33 hospitals were participating by January 2006, 46 by January 2007, and 53 by December 2007 (of 110 hospitals eligible to participate). Admission for stroke to the 53 participating hospitals accounted for approximately 69% of the total stroke admissions for North Carolina based on 2006 hospital discharge data (ICD-9-CM codes 430--438).
Case Definition
PCNASR includes patients aged ≥18 years with a clinical diagnosis of acute ischemic stroke, intracerebral hemorrhage, subarachnoid hemorrhage, or transient ischemic attack (TIA)† or an ICD-9-CM code indicative of a stroke or TIA.§ Patients who were already hospitalized at the time of stroke or TIA occurrence were not included in the PCNASR case definition and therefore not counted in the registry.
PCNASR program guidelines during 2004--2007 required hospitals to collect data for a minimum of 6 of every 12 consecutive months. Georgia and Massachusetts required hospitals to enter data every month.
PCNASR does not require states to include in the registry patients who were admitted to an ED but who were not admitted to the hospital. However, Massachusetts hospitals are legally required to enter into a registry all stroke cases in persons who arrive at a hospital (including an ED) within 3 hours of symptom onset and who still have symptoms when they arrive at the hospital.
Case Ascertainment
Hospitals were encouraged to identify stroke cases in the ED or at the time of hospital admission (prospective case ascertainment) and to collect data concurrently with hospital care. However, case ascertainment methods varied. Some hospitals prospectively identified cases, and some hospitals retrospectively identified cases based on ICD-9-CM codes and were asked to verify that these cases met the clinical case definition. Data collection tools used in Illinois and North Carolina contained questions regarding prospective and retrospective case ascertainment. The percentage of prospective case ascertainment compared with retrospective case ascertainment varied based on hospital personnel resources and use of electronic medical records.
Data Collection
State registry programs collected data for the registry using a uniform set of PCNASR data elements and definitions (Box 1). States were required to submit state registry data to CDC at the end of each calendar quarter. Data CDs from each state were mailed overnight to CDC as password-protected transport files; passwords were sent separately through a different carrier.
Methods for data collection varied among states. Georgia and Massachusetts used a modified version of an online patient management tool from Get With The Guidelines---Stroke, an American Heart Association program designed to improve stroke care for patients by measuring and increasing adherence to evidence-based guidelines.¶ The patient management tool was modified to include PCNASR data elements.
The Illinois and North Carolina registries used custom-designed data collection tools. The Illinois registry program developed an online tool to collect data, which were submitted electronically to the Center for Stroke Research at the University of Illinois at Chicago, the agency that managed the data for the Illinois registry. The North Carolina registry program also developed an online data collection tool, which included all required PCNASR data elements and optional data elements. The tool was designed to follow the typical flow of patient care to encourage prospective collection of data. In Illinois and North Carolina, hospitals have access to their own data and to aggregate data on performance measures combined from all participating hospitals in their respective state.
The specific strategies for training hospital staff members (e.g., how to abstract information from medical records, enter data, and understand and interpret data elements identified in the medical record) varied among states. However, most strategies included initial training sessions when a hospital began participating and varying levels of ongoing data abstraction training and support. Registry staff members performed the training sessions.
Completeness of Case Ascertainment and Data Validation
Case Ascertainment
All states determined the percentage of stroke patients admitted to the hospital for whom data were entered into the registry (i.e., completeness of case ascertainment). The registries in Georgia and Massachusetts monitored completeness of case ascertainment by comparing the number of cases entered by each hospital into the registry with the number of cases expected based on previous hospital discharge data, using ICD-9-CM codes to identify cases. The Georgia registry hospitals submitted monthly lists of discharged patients with selected primary stroke-related ICD-9-CM codes, and the number of cases on these lists was compared with the number of cases entered into the registry. The Illinois registry hospitals submitted reports at least annually of the number of discharged patients with a principal diagnosis of stroke or TIA, and the number of cases on these lists was compared with the actual number of abstracted cases entered into the registry (i.e., both retrospectively and prospectively identified cases). Hospitals that entered fewer cases in the registry than expected during the relevant time frame were provided assistance from registry staff members to identify barriers to case ascertainment and increase the number of cases entered into the registry.
In North Carolina, after 6 months of participation, hospitals were asked to compile hospital discharge data. The North Carolina registry program then provided participating hospitals a list of all stroke cases that had been entered into the registry during their seventh month of participation and requested that these cases be compared with the hospital discharge data for the same month. The hospitals were asked to verify that the registry cases were in the discharge data and compile a list of any recorded stroke-related cases that were missed, including information such as admission date and time, whether the patient had been admitted directly to the hospital or through the ED, and whether the stroke onset occurred while the patient was hospitalized. The proportion of stroke cases entered into the registry was calculated every 6 months based on the date the hospital began abstracting data.
Data Validation
All state registry programs monitored data accuracy. The tools used to collect registry data included internal checks to highlight and prevent the entry of implausible values. PCNASR required at least 5% of charts be reabstracted to assess the accuracy of data abstraction.
Georgia
Registry staff members in Georgia monitored data entered by hospitals for errors such as implausible values and asked hospitals to correct identified errors. Registry staff members also asked hospitals to submit to the Georgia Medical Care Foundation photocopies of clinical charts for a random sample of 10% of cases entered into the registry; statistical software was used to select the sample of cases. The medical information for these cases was reabstracted at the foundation by trained abstractors to assess the interrater reliability of the data using kappa statistics and whether entered cases met the clinical case definition. Data from the reabstractions were compared with data from the original chart abstractions, and results of the interrater reliability testing were provided to hospitals in a year-end report. Information from the chart reabstractions was used for subsequent data abstraction training sessions.
Illinois
Registry staff members in Illinois monitored data entered by hospitals by reabstracting cases soon after the original hospital abstraction. After abstractors at a hospital had entered data for at least 10 cases, two registry staff members visited the hospital to reabstract random samples of charts to monitor the accuracy of the initial abstraction. During this data monitoring visit, data abstracted by hospital staff members and then reabstracted by registry staff members were compared. Discrepancies were addressed, additional training was provided, and the hospital plan for concurrent case identification, chart abstraction, and data entry was reviewed.
Massachusetts
Registry staff members in Massachusetts monitored data entered by Massachusetts hospitals for errors, and hospitals were asked to correct identified errors. John Snow, Inc. (JSI) was hired to reabstract a random sample of approximately 10% of cases entered into the registry; charts were reabstracted at the hospitals by trained JSI abstractors and assessed for accuracy and reproducibility. Because few patients were eligible to receive thrombolytics and adherence to thrombolytic guidelines was poor in the prototype registries, cases for reabstraction were oversampled for patients who were eligible to receive thrombolytics. Immediate feedback was given to hospital staff members involved in the registry program, and the reabstractions results were used to develop future data quality training sessions.
North Carolina
The North Carolina registry developed a computer program to identify possible data errors. The program was run weekly and used to generate queries for hospitals to use while reviewing data. Hospitals were encouraged to use these queries to investigate and correct incomplete and inaccurate data. A random sample of 5% of cases entered at each hospital was reabstracted by hospital staff members and entered into the registry website, which allowed prospectively collected registry data to be compared with data in the medical records. The North Carolina registry program website links registry entries with the original records, which facilitates comparisons between original data and the data from reabstractions.
Data Quality
PCNASR continually monitors data to improve the quality and accuracy of data entered into state registries. After each quarterly data submission by state registry programs to CDC, CDC provides state registry programs with individual reports on missing, invalid, and questionable data. State registry programs use this information to work with hospitals to correct data (if possible). State registry programs help hospitals improve data abstraction by providing regular training sessions for new abstractors, conducting regular conference calls, and creating lists of responses to frequently asked questions about abstraction guidelines.
Hospital Inventory
State registry programs collect self-reported baseline hospital information, including annual numbers of stroke cases, number of hospital beds, and information on hospital resources for stroke care. Any information that identifies the hospitals is removed, and the inventory information is transmitted to CDC annually.
Quality Improvement
In addition to monitoring hospital care provided to stroke patients, PCNASR was created to improve the quality of stroke care. Hospitals have access to their own data and state-level aggregate data from other sites for use in developing quality improvement strategies; hospitals do not have access to patient-level data from other hospitals. PCNASR quality improvement occurs in two stages. First, the state registry program recruits hospitals (as discussed in a previous section) to participate in a hospital-based, patient-level quality improvement program for acute stroke care. Second, state registry programs are required to develop a quality improvement plan for hospitals and for the state registry. Registry staff members provide quality improvement assistance to hospitals in various ways, including evaluation of stroke-related quality improvement activities, hospital visits to consult with hospital staff members caring for stroke patients (i.e., the stroke team), training (in person or through conference calls), and workshops with participating hospitals.
During 2005--2007, PCNASR assessed 10 major performance measures of care for stroke patients (Box 2). Data also were collected on selected additional measures, including time between hospital arrival and receipt of brain imaging (a measure of optimal stroke care), time between hospital arrival and receipt of tPA, and time between hospital arrival and receipt of brain imaging by method of arrival (e.g., EMS versus private transportation). The 10 performance measures, which were developed by CDC in partnership with neurologists who specialize in stroke care, are based on established guidelines for care of acute stroke patients (10--18). Not all performance measures are applicable to every type of stroke for which information is collected in PCNASR. The performance measures are reported as the proportion of patients who received the intervention or treatment (numerator) among the proportion of patients eligible to receive the intervention or treatment (denominator). Patients who were discharged to another acute care hospital and patients who left the hospital against medical advice were excluded. In addition, each performance measure has specific inclusion and exclusion criteria based on stroke type and other factors (Box 2).
Hospital-based quality improvement programs also address implementation of stroke care processes recommended by the Brain Attack Coalition (BAC) to improve adherence to guidelines for acute stroke care. BAC recommendations include use of standardized stroke orders and protocols, establishment of acute stroke care protocols, hospital notification by EMS of incoming potential stroke patients, and establishment of stroke units within hospitals (19).
State registry programs used conference calls and in-person meetings to implement educational programs for participating hospital stroke quality improvement teams. These meetings allowed stroke team members to discuss successes and challenges and included topics such as how to improve adherence to the stroke performance measures, how to implement evidence-based guidelines such as those recommended by BAC, and how to address barriers to implementation. In-person meetings with registry staff members and hospital stroke teams took place at least annually in all states.
Analytic Methods
Adherence to performance measures was calculated using predefined inclusion and exclusion criteria; hemorrhagic stroke, ischemic stroke, ill-defined stroke, and TIA cases were included (Table 1 and Box 2). To eliminate invalid values, data on time intervals (i.e., time from hospital arrival to receipt of brain imaging) were reported based on a range of 0--240 hours (except for length of hospital stay, which was reported based on a range of 1--120 days). The chi-square test was used to examine differences between categorical variables; the Wilcoxon-Mann-Whitney rank test or the Kruskal-Wallis test was used to examine differences between continuous variables. All statistical analyses were conducted using unweighted aggregate data.
Results
Characteristics of Participating Hospitals
Of 208 hospitals recruited during 2005--2007, a total of 195 contributed data to the registry; hospital inventory information was available for 190 of these 195 hospitals (Table 2). Twenty percent of the hospitals had <100 beds, and 22.1% had ≥400 beds. The annual number of stroke and TIA cases per hospital ranged from 12 to 1,532 per year, with 5.8% of hospitals reporting ≤25 cases per year and 10.5% of hospitals reporting ≥750 stroke cases per year. A total of 66.3% of the hospitals were nonteaching hospitals (i.e., did not have residency programs). Nearly all (91.1%) hospitals had physical therapy available in the hospital; 86.8% had occupational therapy, and 83.7% had speech therapy. A total of 12.6% of hospitals were categorized as rural,** and many of these were critical-access hospitals.
Patient Demographics
Sex and Race/Ethnicity Overall and by State
Approximately half (53.3%) the stroke cases recorded in the registry occurred among females, a proportion that varied little by state (Table 3). Overall, 2.5% of cases were among Hispanics; however, the proportion of Hispanics varied significantly by state (chi-square test, p<0.001). In addition, race varied significantly by state (chi-square test, p<0.001). The proportion of cases among black stroke patients ranged from 5.6% in Massachusetts to 35.8% in Georgia.
Age
The age at which patients experienced stroke varied significantly among states (comparison of mean age among the four states, p <0.001). On average, patients were oldest in Massachusetts (median age: 77 years) and youngest in Georgia (median age: 67 years) (Table 3). Compared with men, women were significantly older (median age for women: 75 years, median age for men, 68 years [p<0.001]) (Table 4). The age at which strokes occurred also varied significantly by race. Whites who had strokes were significantly older than other racial groups (p<0.001). Black male stroke patients were significantly younger than white male stroke patients (p<0.001), and black females were significantly younger than white females (p<0.001). The median age among Hispanic stroke patients was 62 years (range: 18--97 years), compared with 72 years (range: 18--108 years) among non-Hispanics (p<0.001).
Diagnoses
Among stroke cases entered in the registry, the clinical diagnosis for 13.8% of cases was hemorrhagic stroke (unspecified cranial hemorrhage or combined intracerebral hemorrhage and intracranial hemorrhage), for 56.2% was ischemic stroke, for 7.3% was ill-defined stroke (i.e., medical record did not specify ischemic or hemorrhagic stroke), and for 21.6% was TIA (Table 5). Because more than one stroke type could be entered into the registry for a single stroke case (e.g., a case of hemorrhagic stroke that converted to an ischemic stroke, which could be categorized as both ischemic and hemorrhagic), determining a single type was not possible in a small proportion (1.1%) of cases. Stroke type varied substantially by state. Twenty percent of stroke cases in Georgia were hemorrhagic strokes, compared with 5.3% in Massachusetts. Because the Massachusetts PSS regulations do not address hemorrhagic stroke, caution should be used in interpreting the variability in stroke type for Massachusetts.
EMS, Prehospital, and ED Care
Of the 56,969 patients, 47.6% were transported by EMS from the scene of symptom onset, 11.1% were transferred by EMS from another hospital, and 39.4% used private or other transportation (Table 6). Mode of transportation was unknown or missing for 1.9% of patients. Most patients (90.4%) arrived at the ED for assessment; 8.4% were directly admitted to the hospital and did not use the ED. Of the 33,488 patients who were transported by EMS, the time from symptom onset to EMS call was missing or unknown in 81% of cases; two thirds of these were a result of unknown time of symptom onset (e.g., patients who woke from sleep to realize they had experienced a stroke). For patients who arrived within 10 days (i.e., 240 hours) of symptom onset, the median time from symptom onset to EMS call was 1 hour, 12 minutes (mean: 4 hours, 24 minutes). The time from symptom onset to arrival at the ED was missing or unknown in 58% of cases. For patients arriving within 10 days of symptom onset and with known time of symptom onset, the median time from onset to ED arrival was 2 hours, 30 minutes (mean: 6 hours, 12 minutes).
Initial Treatment and Receipt of Brain Imaging
A total of 18.5% of patients with stroke symptoms arrived at the hospital within 2 hours of symptom onset, 21.7% arrived in 2--24 hours, and 2.0% arrived >24 hours after symptom onset (Table 7). For the majority (57.8%) of patients, the time from onset of symptoms to hospital arrival was not recorded or was unknown. The time from hospital arrival to receipt of brain imaging was known for 82% of patients. The median time from hospital arrival to brain imaging among all patients was 1 hour, 12 minutes (mean: 2 hours, 36 minutes). However, among patients who arrived at the hospital within 2 hours of symptom onset, the median time from hospital arrival to receipt of brain imaging was 42 minutes (mean: 1 hour, 18 minutes). The initial brain image indicated hemorrhagic stroke in 13.9% of cases; imaging results were not available or were missing in 1.7% of cases. Fourteen percent of all hemorrhagic stroke patients had a National Institutes of Health Stroke Scale (NIHSS) score recorded (median score: 8), and 34% of ischemic stroke patients had an NIHSS score recorded (median score: 4).†† A neurologist was involved in the care of 62.1% of stroke patients.
Receipt of tPA
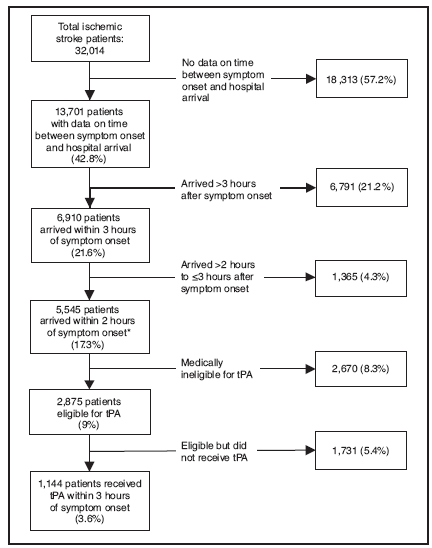
Among patients who experienced an ischemic stroke, 17.3% arrived within 2 hours of symptom onset. An additional 4.3% arrived 2--3 hours after symptom onset (Figure 1). The remaining 78.4% of patients either arrived >3 hours after symptom onset or did not know when their symptoms began or were not asked when symptoms began. To calculate the number of patients who were eligible for tPA, only patients who arrived within 2 hours of symptom onset and had no contraindications for tPA were considered. Of those 5,545 patients that arrived within 2 hours of symptom onset, 2,875 were eligible for tPA (9% of all ischemic stroke patients).
Patients identified by a health-care provider as having contraindications for tPA and who had documentation of the contraindication in the medical record were considered ineligible for tPA (Table 8). For patients who arrived within 2 hours of onset of stroke symptoms, the most common reasons for being ineligible for tPA were rapid improvement or mild stroke (46.6%) or any of the following contraindications: uncontrolled hypertension; recent surgery; recent trauma; recent stroke; active internal bleeding; suspicion of subarachnoid hemorrhage; platelets <100,000, partial thromboplastin time >40 seconds after heparin use, prothrombin time >15 seconds, or an international normalized ratio >1.7, or known bleeding diathesis; history of intracranial hemorrhage, brain aneurysm, vascular malformation, or brain tumor (22.6%); findings on brain imaging (7.7%); patient or family refusal (7.4%); and age (5.3%).
Lipid Levels
Lipid levels were measured after hospital admission, or previous lipid levels were recorded if the levels had been measured within 30 days before the stroke and were available in the medical record. Median total cholesterol and low-density lipoprotein cholesterol levels did not differ between hemorrhagic stroke and ischemic stroke patients (170 mg/dL and 171 mg/dL, 101 mg/dL and 102 mg/dL, respectively) (Table 9). The median high-density lipoprotein cholesterol level was significantly higher in hemorrhagic stroke patients compared with ischemic stroke patients (45 mg/dL and 41 mg/dL, respectively). The median triglyceride level was significantly lower in hemorrhagic stroke patients compared with ischemic stroke patients (99 mg/dL and 110 mg/dL, respectively).
Stroke Risk Factors
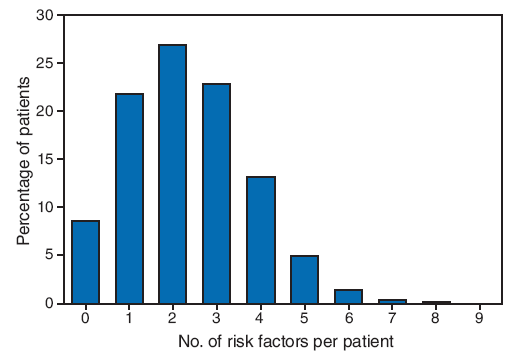
PCNASR includes medical history information for each patient, including 10 risk factors for stroke: previous stroke or TIA, history of ischemic heart disease, history of atrial fibrillation, history of hypertension, history of hyperlipidemia, history of diabetes, cigarette smoking during the preceding year, history of peripheral arterial disease, presence of a heart valve prosthesis, and history of carotid stenosis. Seventy percent of patients had more than one risk factor for stroke, and 8.6% had no risk factors (Figure 2).
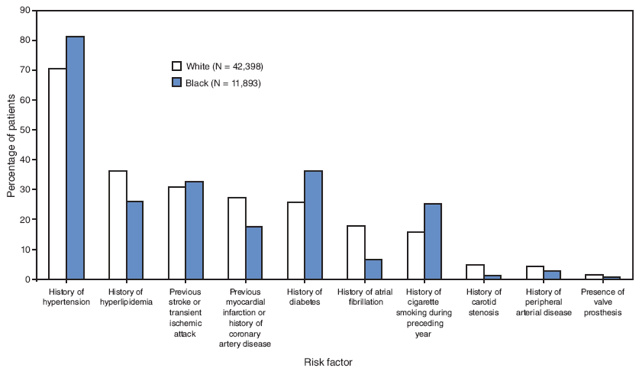
The most common risk factors were history of hypertension (72.7%), history of hyperlipidemia (33.8%), previous stroke or TIA (30.9%), history of diabetes (28.2%), previous myocardial infarction or history of coronary artery disease (24.7%), cigarette smoking (17.7%), and history of atrial fibrillation (15.1%) (Figure 3). A history of peripheral arterial disease, history of carotid stenosis, or presence of a valve prosthesis were recorded for <5% of patients. The prevalence of all risk factors differed significantly between white and black patients, with blacks having a higher prevalence of history of hypertension, diabetes, smoking, and previous stroke or TIA. The most common combinations of risk factors were hypertension and dyslipidemia (28.5%), hypertension and diabetes (23.8%), hypertension and previous stroke or TIA (24.4%), and hypertension and previous myocardial infarction or history of coronary artery disease (20.0%). The combination of hypertension, diabetes, and dyslipidemia, three components of metabolic syndrome, occurred in 11.0% of patients.
Risk factor prevalence varied by stroke type. Patients with hemorrhagic stroke had a lower prevalence of each risk factor than patients with ischemic stroke for all risk factors except cigarette smoking (Table 10).
Discharge Information
Median length of hospital stay varied by type of stroke: hemorrhagic stroke, 7 days; ischemic stroke, 4 days; and TIA, 2 days (Table 11). A total of 86.6% of ischemic stroke patients received rehabilitation services or were assessed for the need for rehabilitation services, compared with 68% of hemorrhagic stroke patients. Discharge status varied by diagnosis: 30.3% of hemorrhagic stroke patients were discharged home, compared with 45.8% of ischemic stroke patients; 22.7% of hemorrhagic stroke patients died, compared with 5.7% of ischemic stroke patients; 3.5% of hemorrhagic stroke patients were discharged to a hospice setting, compared with 2.5% of ischemic stroke patients. Hemorrhagic stroke and ischemic stroke patients were equally likely to be discharged to chronic care facilities (43.0% and 45.5%, respectively).
Ambulation Status
Approximately half (51.1%) of hemorrhagic, ischemic, or ill-defined stroke patients were able to ambulate independently before and after the stroke (Table 12). Among all stroke patients, 26.9% were able to ambulate independently before the stroke but only with assistance after the stroke, 12.9% were able to ambulate independently before the stroke but unable to ambulate after the stroke, and 2.2% were able to ambulate with assistance before the stroke but unable to ambulate after the stroke.
Adherence to Performance Measures
Ten measures of acute stroke care were developed for PCNASR by CDC in partnership with neurologists who specialize in stroke care. In this report, these measures are not used to assess improvement over time but rather to assess total performance for the entire 36-month reporting period. Receipt of antithrombotic therapy within 48 hours of admission or by the end of the second hospital day, antithrombotic therapy at discharge, and assessment for rehabilitation services were >90% for the reporting period. Receipt of tPA by eligible patients averaged 39.8% during 2005--2007 (Table 13).
Discussion
PCNASR provides information on the quality of care provided to stroke patients by collecting data on specific stroke performance measures. PCNASR assesses these data to identify areas of stroke care in need of improvement and to develop and implement quality improvement interventions in participating hospitals. A total of 195 hospitals contributed data in PCNASR during 2005--2007, representing 56,969 patients. PCNASR is based within and led by state health departments, indicating that a state-based registry is feasible. Rates of adherence to measures of quality of care improved between the 2001--2004 prototype phase and the 2005--2007 phase of the PCNASR. Substantial improvement occurred in dysphagia screening (56.7% versus 45.4%), lipid testing (69.9% versus 33.6%), smoking cessation counseling (78.6% versus 21.4%), and antithrombotic therapy prescribed at discharge (97.6% versus 91.5%) (3).
Despite these improvements, no change occurred in the proportion of patients who arrived at the hospital in time to receive thrombolytic therapy for ischemic stroke. Only 9% of all ischemic stroke patients were determined to be eligible to receive tPA, and only 3.6% of all ischemic stroke patients received tPA. Approximately half of ischemic stroke patients lacked documented information on time of symptom onset, and an additional 25% arrived too late to receive tPA. A total of 39.8% of acute ischemic stroke patients who were eligible for tPA received tPA within 3 hours of symptom onset. Stroke patients might have their stroke while sleeping and therefore will not know the time of onset; however, many others are unaware of the signs and symptoms of stroke. In addition, nearly 40% of stroke patients did not use EMS services for transport to hospitals, which might have contributed to prehospital delays and increased the number of ischemic stroke patients who were ineligible to receive thrombolytic therapy. This finding highlights the need for ongoing public health measures to inform the public about signs and symptoms of stroke and the need to activate EMS for suspected stroke. Timely recognition of stroke and hospital transport are necessary for patients to be eligible to receive tPA.
Three of the 10 acute stroke performance measures were met for >90% of patients: 1) treating patients with antithrombotic therapy within 48 hours of admission or by the end of the second hospital day, 2) prescribing antithrombotic therapy at discharge, and 3) assessing the need for rehabilitation. A total of 90.1% of stroke patients were assessed for the need for rehabilitation services. Forty-four percent of stroke patients who could ambulate independently before the stroke could not ambulate independently after the stroke, highlighting the need for access to rehabilitation.
Demographic data from PCNASR indicated high rates of hypertension among both white (71%) and black (81%) stroke patients, highlighting the substantial relationship between stroke and hypertension and the need for prevention of this important risk factor. PCNASR data also indicate that the mean age of black stroke patients is 10 years younger than that of whites (62 years versus 72 years). The younger age of stroke patients in Georgia (mean: 66 years) likely reflects the higher proportion of black patients in the Georgia (36%) registry; Massachusetts, which has a much lower proportion of black stroke patients (5.6%) in the registry, had the oldest stroke patients of the four states (mean: 73 years). Stroke is a leading cause of disability and affects a greater proportion of blacks during their productive work years.
The United States has approximately four neurologists per 100,000 persons. U.S. neurologists treat approximately 700,000 acute strokes per year; however, patients in many parts of the United States have no access to acute stroke services (20). PCNASR data indicate that neurologists were involved in the care of 62.1% of stroke patients. Most rural hospital staffs do not include neurologists. Telemedicine might increase neurologist participation in acute stroke care and improve geographic disparities in access to quality stroke care. In the Veteran's Administration Acute Stroke Study, care of stroke patients by a neurologist was associated with increased testing, improved outcomes, and decreased mortality in acute stroke patients (21).
The ultimate goal of programs such as PCNASR and Get With the Guidelines---Stroke (GWTG---S) is to improve care provided to stroke patients. GWTG---S reported improvements in stroke care in 99 participating hospitals (22). In a CMS review of another program to improve stroke care in the United States (the Medicare Quality Improvement Organization program), the median performance among all states in three performance measures related to stroke care improved between 1998--1999 and 2000--2001 (23). Additional analyses are needed to assess improvements in adherence to guidelines over time.
Although PCNASR focuses primarily on the 10 described acute stroke care performance measures, data on selected hospital outcomes also were collected, including in-hospital deaths by type of stroke. In-hospital deaths occurred among 22.7% of patients who experienced hemorrhagic stroke, 5.7% of patients who experienced ischemic stroke, and 4.3% of patients who experienced ill-defined strokes. These rates are similar to those reported in a study that involved 857 hospitals and 365,186 patients. In that study, in-hospital mortality for hemorrhagic and ischemic strokes was 25.9% and 5.5%, respectively (24). A recent report from the Registry of the Canadian Stroke Network found that the level of organized hospital stroke care, as determined by the presence or absence of occupational therapy, physical therapy, stroke team assessment, and admission to a stroke unit, was related to the risk-adjusted 7-day stroke mortality (25). Additional studies of outcomes associated with acute stroke performance measures in hospitals are needed to assess other outcomes (e.g., disability, postacute care, and quality of life), as are better methods of calculating risk-adjusted stroke mortality (26).
Arriving at the hospital by EMS was associated with a shorter time between hospital arrival and initial CT scan, a finding that is consistent with previous reports (27,28). This finding highlights the need for persons who are experiencing stroke signs and symptoms to be transported to the hospital by EMS rather than other forms of transportation. Combined PCNASR data from all four states indicated a median time of 42 minutes from hospital arrival to initial CT scan among patients who arrived within 2 hours of symptom onset, the same time as in North Carolina, suggesting that the combined data are consistent with data from a single state.
The findings in this report are subject to at least four limitations. First, methods for hospital selection and data validation varied among states. PCNASR data are not intended to be used for population estimates but rather to reflect care provided by hospitals participating in PCNASR. Second, the number of Hispanic cases is limited; therefore, statistical comparison of data on Hispanics should be interpreted with caution. Third, certain data were missing or excluded. For example, EMS date and times of service were missing from 81% of medical records because EMS trip sheets are not part of the hospital medical record; time of stroke was unknown in 57% of cases. Ambulation status was missing in 30% of stroke cases, lipid levels were missing in 38% of cases, and NIHSS scores were missing in 66% of ischemic stroke cases. In addition, because TIA patients often are not admitted to the hospital or are admitted to an observation unit only, not all TIA patients were included in the registry. Inclusion of patients admitted for short-term ED observation is optional, and ED cases that do not result in hospital admission are not typically included. (Massachusetts is the only state that requires inclusion of all stroke patients who arrive at the ED within 3 hours of symptom onset and still have symptoms on arrival.) Finally, although states reabstract at least 5% of cases to assess data accuracy, and CDC works with state registry programs to improve the accuracy of abstracted data, the overall accuracy of data likely varies among states and hospitals. Determining the completeness of data abstraction is difficult because the case definition is based on clinical diagnosis and retrospective comparisons with hospital case records based on ICD-9-CM codes. State registry programs report that they include approximately 57% of stroke discharges at registry hospitals based on ICD-9-CM codes. Because only a subset of these ICD-9-CM codes (430--438) represent acute stroke or TIA, the actual percentage of cases abstracted is thought to be >57%. The limitations of using ICD-9-CM codes to identify acute stroke patients have been described previously (29,30). State-reported estimates on case ascertainment based on hospital discharge records ranged from 54% to 97%.
Conclusion
Data from the 2005--2007, the first 3 years of PCNASR, provide a useful marker from which future trends can be evaluated, including acute stroke patient characteristics, hospital diagnostic and treatment performance measures, discharge status, and estimates of time from stroke onset to treatment. The focus on recruiting diverse types of hospitals within each state allows for identification of geographic and demographic variations in stroke care. The quality improvement component of the registry allows state health departments to work with hospitals to improve the stroke care and reduce disparities in care, including disparities by geographic area, race, and sex .
Implementing PCNASR within state health departments has several advantages, including 1) broadening stroke care to include linking secondary and primary stroke prevention activities; 2) capitalizing on established relationships with the various hospitals in the state; 3) engaging local health departments, state regulators, and regional health coordinators in the recruitment and retention of registry sites; 4) local monitoring of data quality; and 5) customizing quality improvement initiatives to meet local needs. PCNASR is implementing various quality improvement initiatives in funded states, including regional collaborations with hospital stroke quality improvement teams, data feedback to hospitals in the form of grand rounds presentations to a wide hospital staff audience, use of small tests of change to improve hospital care processes and pathways, identifying physicians willing to promote stroke quality of care initiatives, engaging hospital administration, and focused discussions on barriers and opportunities to implement best practices. This collaborative, state- and hospital-based quality improvement registry can be used to develop comprehensive stroke care protocols and to identify disparities in care by race/ethnicity, geographic region, and sex, which can be used to improve access to higher quality care for stroke patients in every state.
References
- Lloyd-Jones D, Adams R, Carnethon M, et al. Heart disease and stroke statistics---2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2009;119:e21--e181.
- Wattigney WA, Croft JB, Mensah GA, et al. Establishing data elements for the Paul Coverdell National Acute Stroke Registry: part I: proceedings of an expert panel. Stroke 2003;34:151--6.
- Reeves MJ, Broderick JP, Frankel M, et al. The Paul Coverdell National Acute Stroke Registry: initial results from four prototypes. Am J Prev Med 2006;31(6 Suppl 2):S202--S9.
- Rose KM, Rosamond WD, Huston SL, Murphy CV, Tegeler CH. Predictors of time from hospital arrival to initial brain-imaging among suspected stroke patients: the North Carolina Collaborative Stroke Registry. Stroke 2008;39:3262--7.
- Adams HP Jr, del Zoppo G, Alberts MJ, et al. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: The American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Stroke 2007;38:1655--711.
- Saver JL, Yafeh B. Confirmation of tPA treatment effect by baseline severity-adjusted end point reanalysis of the NINDS-tPA Stroke Trials. Stroke 2007:38:414--6.
- Hacke W, Donnan G, Fieschi C, et al. Association of outcome with early stroke treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet 2004;363:768--74.
- National Institute of Neurological Disorders and Stroke. Proceedings of a national symposium on rapid identification and treatment of stroke. December 12--13, 1996; Washington DC: National Institute of Neurological Disorders and Stroke; 2002. NIH publication no. 97-4239. Available at http://www.ninds.nih.gov/news_and_events/proceedings/strokeworkshop.htm.
- CDC. Awareness of stroke warning symptoms---13 states and the District of Columbia, 2005. MMWR 2008;57:481--5.
- Sacco RL, Adams R, Albers G, et al. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack: a statement for healthcare professionals from the American Heart Association/American Stroke Association Council on Stroke: co-sponsored by the Council on Cardiovascular Radiology and Intervention: the American Academy of Neurology affirms the value of this guideline. Stroke 2006;37:577--617.
- Duncan PW, Zorowitz R, Bates B, et al. Management of adult stroke rehabilitation care: a clinical practice guideline. Stroke 2005;36:e100--e143.
- Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2004;126(3 Suppl):338S--400S.
- Albers GW, Amarenco P, Easton JD, Sacco RL, Teal P. Antithrombotic and thrombolytic therapy for ischemic stroke. Chest 2001;119:300S--320S.
- Adams H, Adams R, Del Zoppo G, Goldstein LB. Guidelines for the early management of patients with ischemic stroke: 2005 guidelines update a scientific statement from the Stroke Council of the American Heart Association/American Stroke Association. Stroke 2005;36:916--23.
- Coull BM, Williams LS, Goldstein LB, et al. Anticoagulants and antiplatelet agents in acute ischemic stroke. Report of the Joint Stroke Guideline Development Committee of the American Academy of Neurology and the American Stroke Association (a division of the American Heart Association). Stroke 2002;33:1934--42.
- Goldstein LB, Adams R, Alberts MJ, et al. Primary prevention of ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council: co-sponsored by the Atherosclerotic Peripheral Vascular Disease Interdisciplinary Working Group; Cardiovascular Nursing Council; Clinical Cardiology Council; Nutrition, Physical Activity, and Metabolism Council; and the Quality of Care and Outcomes Research Interdisciplinary Working Group: the American Academy of Neurology affirms the value of this guideline. Stroke 2006;37:1583--633.
- National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002;106:3143--421.
- Amarenco P, Bogousslavsky J, Callahan A 3rd, et al; Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) Investigators. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med 2006;355:549--59.
- Alberts MJ, Hademenos G, Latchaw RE, et al. Recommendations for the establishment of primary stroke centers. Brain Attack Coalition. JAMA 2000;283:3102--9.
- Schwamm LH, Audebert HJ, Amarenco P, et al. Recommendations for the implementation of telemedicine within stroke systems of care: a policy statement from the American Heart Association. Stroke 2009;40:2635--60.
- Goldstein LB, Matchar DB, Hoff-Lindquist J, Samsa GP, Horner RD. VA Stroke Study: neurologist care is associated with increased testing but improved outcomes. Neurology 2003;61:792--6.
- LaBresh KA, Reeves MJ, Frankel MR, Albright D, Schwamm LH. Hospital treatment of patients with ischemic stroke or transient ischemic attack using the "Get With The Guidelines" program. Arch Intern Med 2008;168:411--7.
- Jencks SF, Huff ED, Cuerdon T. Change in the quality of care delivered to Medicare beneficiaries, 1998--1999 to 2000--2001. JAMA 2003;289:305--12.
- Reeves MJ, Smith E, Fonarow G, Hernandez A, Pan W, Schwamm LH; GWTG---Stroke Steering Committee & Investigators. Off-hour admission and in-hospital stroke case fatality in the Get With The Guidelines---Stroke Program. Stroke 2009;40:569--76.
- Saposnik G, Fang J, O'Donnell M, Hachinski V, Kapral MK, Hill MD; Investigators of the Registry of the Canadian Stroke Network (RCSN) for the Stroke Outcome Research Canada (SORCan) Working Group. Escalating levels of access to in-hospital care and stroke mortality. Stroke 2008;39:2522--30.
- Kelly A, Thompson JP, Tuttle D, Benesch C, Holloway RG. Public reporting of quality data for stroke: is it measuring quality? Stroke 2008;39:3367--71.
- Smith MA, Doliszny KM, Shahar E, McGovern PG, Arnett DK, Luepker RV. Delayed hospital arrival for acute stroke: the Minnesota Stroke Survey. Ann Intern Med 1998;129:190--6.
- Schroeder E, Rosamond WD, Morris DL, Evenson KR, Hinn AR. Determinants of use of emergency medical services in a population with stroke symptoms: the Second Delay in Accessing Stroke Healthcare (DASH II) study. Stroke 2000;31:2591--6.
- Goldstein LB. Accuracy of ICD-9-CM coding for the identification of patients with acute ischemic stroke: effect of modifier codes. Stroke 1998;29:1602--4.
- Benesch C, Witter DM Jr, Wilder AL, Duncan PW, Samsa GP, Matchar DB. Inaccuracy of the International Classification of Diseases (ICD-9-CM) in identifying the diagnosis of ischemic cerebrovascular disease. Neurology 1997;49:660--4.