 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Strategies for Reducing Exposure to Environmental Tobacco Smoke, Increasing Tobacco-Use Cessation, and Reducing Initiation in Communities and Health-Care SystemsA Report on Recommendations of the Task Force on Community Preventive Services Task Force on Community Preventive Services
CHAIR VICE-CHAIR
MEMBERS
George J. Isham, M.D. Patricia A. Buffler, Ph.D., M.P.H. Mary Jane England, M.D. David W. Fleming, M.D.* Mindy Thompson Fullilove, M.D. Fernando A. Guerra, M.D., M.P.H. Alan R. Hinman, M.D., M.P.H. Garland H. Land, M.P.H. Charles S. Mahan, M.D. Patricia Dolan Mullen, Dr.P.H. Susan C. Scrimshaw, Ph.D. Robert S. Thompson, M.D. * As of June 2000, Dr. Fleming is with CDC in Atlanta, Georgia, and no longer serves on the Task Force. The following CDC staff members prepared this report: David P. Hopkins, M.D., M.P.H. Division of Prevention Research and Analytic Methods Epidemiology Program Office Corinne G. Husten, M.D., M.P.H. Office on Smoking and Health National Center for Chronic Disease Prevention and Health Promotion in collaboration with Jonathan E. Fielding, M.D., M.P.H., M.B.A. SummaryReducing tobacco-related morbidity and death is an ongoing challenge for health-care providers, health-care systems, and public health programs. Interventions are available that a) reduce exposure to environmental tobacco smoke, b) reduce tobacco-use initiation,* and c) increase tobacco-use cessation.**The Task Force on Community Preventive Services has conducted systematic reviews on 14 selected interventions, which are appropriate for communities and health-care systems, and has made recommendations regarding use of these interventions. This report summarizes the recommendations, identifies sources that offer full reviews of the interventions and details about applying the interventions locally, and provides an update of the Task Force's work. BACKGROUNDIn the United States, tobacco use is the leading cause of preventable death (1--3), and exposure to environmental tobacco smoke (ETS) is a preventable cause of significant morbidity and death among nonsmokers (4--6). Reducing tobacco use and reducing exposure to environmental tobacco smoke are essential community and public health objectives (7). As part of the Healthy People 2010 initiative (7), goals have been developed to reduce tobacco-related morbidity and death by reducing exposure to ETS, decreasing tobacco-use initiation, and increasing tobacco-use cessation (Table 1). By implementing interventions shown to be effective, policy makers and health-care and public health providers can help their communities achieve these goals while using community resources efficiently. This report and other related publications provide guidance from the Task Force on Community Preventive Services to personnel in state and local health departments, managed care organizations, purchasers of health care, persons responsible for funding public health programs, and others who have interest in or responsibility for decreasing tobacco use and reducing exposure to environmental tobacco smoke in all segments of the population. INTRODUCTIONThe independent, nonfederal Task Force on Community Preventive Services (the Task Force) is developing the Guide to Community Preventive Services (the Community Guide) with the support of the U.S. Department of Health and Human Services and in collaboration with public and private partners. CDC and other federal agencies provide staff support to the Task Force for development of the Community Guide. However, the recommendations presented in this report were developed by the Task Force and are not necessarily the recommendations of CDC or the U.S. Department of Health and Human Services. This MMWR report is the second to be completed for the Community Guide, a resource that will include multiple chapters, each focusing on a preventive health topic. The first chapter was on vaccine-preventable diseases (8--11), and the information in this report will be part of a second chapter, on tobacco use. This report provides an overview of the process used by the Task Force to select and review evidence; it summarizes the Task Force's recommendations on community interventions to reduce exposure to ETS and tobacco use. A full presentation of the recommendations, supporting evidence, and remaining research questions will be published in the American Journal of Preventive Medicine in 2001. For more information about this report, please call the Office on Smoking and Health (OSH) press line at 770-488-5493. Copies of this report may be obtained through OSH's Web site at <http://www.cdc.gov/tobacco> or by calling 770-488-5705 (press 3 to talk to an information specialist). METHODSMethods used to conduct systematic reviews and link evidence to recommendations have been described elsewhere (12). In brief, for each Community Guide chapter, multidisciplinary chapter development teams conduct reviews by
For the chapter on tobacco use, the chapter development team focused on interventions to decrease exposure to ETS, reduce tobacco-use initiation, and increase tobacco-use cessation. The chapter consultation team members*** generated a comprehensive list of strategies and created a priority list of interventions for review based on their perception of the importance and the extent to which the interventions were practiced in the United States. Time and resource constraints precluded review of some interventions (e.g., communitywide risk factor screening and counseling). Interventions reviewed were either single-component (i.e., using only one activity to achieve desired outcomes) or multicomponent (i.e., using more than one related activity). Interventions were grouped together on the basis of their similarity. Some studies provided evidence for more than one intervention. In these cases, the studies were reviewed for each applicable intervention. The classifications or nomenclature used in this report were chosen to ensure comparability in the review process, and these classifications sometimes differ from those used in the original studies. To be included in the reviews of effectiveness, studies had to meet these criteria: a) they were limited to primary investigations of interventions selected for evaluation; b) they were published in English from January 1980 through May 2000; c) they were conducted in industrialized countries; and d) they compared outcomes in groups of persons exposed to the intervention with outcomes in groups of persons not exposed or less exposed to the intervention (whether the comparison was concurrent or before-after). For each intervention reviewed, the team developed an analytic framework indicating possible causal links between the intervention under study and predefined outcomes of interest. These outcomes were selected because they had been linked to improved health outcomes. For example, the Task Force concluded the following:
The evaluations of interventions in this report, therefore, focus on evidence of effectiveness in reducing ETS exposure, reducing tobacco-use initiation, and increasing tobacco-use cessation (including increasing patient receipt of advice to quit from health-care providers). Each study that met the inclusion criteria was evaluated by using a standardized abstraction form and was assessed for suitability of the study design and threats to validity. On the basis of the number of threats to validity, studies were characterized as having good, fair, or limited execution (12). The strength of the body of evidence of effectiveness was characterized as strong, sufficient, or insufficient on the basis of the number of available studies, the suitability of study designs for evaluating effectiveness, the quality of execution of the studies, the consistency of the results, and the effect size (12). The Community Guide links evidence to recommendations systematically (12). The strength of evidence of effectiveness corresponds directly to the strength of recommendations (e.g., strong evidence of effectiveness corresponds to an intervention being strongly recommended, and sufficient evidence corresponds to an intervention being recommended). Other types of evidence also can affect a recommendation. For example, evidence of harms resulting from an intervention might lead to a recommendation that the intervention not be used, even if it is effective in improving some outcomes. In general, the Task Force does not use economic information to modify recommendations. A finding of insufficient evidence of effectiveness does not result in recommendations regarding an intervention's use but is important for identifying areas of uncertainty and continuing research needs. In contrast, adequate evidence of ineffectiveness leads to a recommendation that the intervention not be used. RESULTSThe systematic search identified 243 studies on tobacco interventions that met the inclusion criteria. Of these 243 studies, 77 were excluded on the basis of limitations in their execution or design and were not considered further. The remaining 166 studies were considered qualifying studies.**** The 14 Task Force evaluations in this report are based on these qualifying studies, all of which had good or fair execution. On the basis of the evidence of effectiveness, the Task Force either strongly recommended or recommended nine of the 14 strategies evaluated (Table 2). These nine recommendations include one intervention to reduce exposure to ETS (smoking bans and restrictions), two interventions to reduce tobacco-use initiation (increasing the unit price for tobacco products and multicomponent mass media campaigns), and six interventions to increase cessation (increasing the unit price for tobacco products; multicomponent mass media campaigns; provider reminder systems; a combined provider reminder plus provider education with or without patient education program; multicomponent interventions including telephone support for persons who want to stop using tobacco; and reducing patient out-of-pocket costs for effective cessation therapies). In addition to the 14 completed evaluations, reviews for three more tobacco prevention interventions --- youth access restrictions, school-based education, and tobacco industry and product restrictions --- are still under way and will be included in the finished chapter. USE OF THE RECOMMENDATIONS IN COMMUNITIES AND HEALTH-CARE SYSTEMSGiven that tobacco use is the largest preventable cause of death in the United States, reducing tobacco use and ETS exposure should be relevant to most communities. In selecting and implementing interventions, communities should strive to develop a comprehensive strategy to reduce exposure to ETS, reduce initiation, and increase cessation. Improvements in each category will contribute to reductions in tobacco-related morbidity and death, and success in one area might contribute to improvements in the other areas as well. Increasing tobacco-use cessation, for example, will reduce exposure to ETS. Smoking bans, effective in reducing exposure to ETS, also can reduce daily tobacco consumption for some tobacco users and help others quit entirely. Choosing interventions that work in general and that are well-matched to local needs and capabilities and then implementing those interventions well are vital steps for reducing tobacco use and ETS exposure. In setting priorities for the selection of interventions to meet local objectives, recommendations and other evidence provided in the Community Guide should be considered along with such local information as resource availability, administrative structures, and economic, social, and regulatory environments of organizations and practitioners. Information regarding applicability can be used to assess the extent to which the intervention might be useful in a particular setting or population. Though limited, economic information --- to be provided in the full report in 2001 --- might be useful in identifying a) resource requirements for interventions, and b) interventions that meet public health goals more efficiently than other available options. If local goals and resources permit, the use of strongly recommended and recommended interventions should be initiated or increased. A starting point for communities and health-care systems is to assess current tobacco-use prevention and cessation activities. Current efforts should be compared with recommendations in this report as well as other relevant program recommendations proposed by CDC (18), the National Cancer Institute (19), the Public Health Service (16), the U.S. Department of Health and Human Services (17,20,21), and the Institute of Medicine (22). In addition to assessing overall progress toward meeting goals and the current status of tobacco control efforts, health planners should also consider how to eliminate health disparities related to tobacco use and ETS exposure. The identification and assessment of existing disparities are critical in selecting and implementing interventions to assist populations at high risk, such as low-socioeconomic populations and some racial/ethnic groups (14,18,20). This review did not examine the evidence of effectiveness of clinical cessation programs or therapies for tobacco dependence, which are not part of the Community Guide mandate but were addressed in an extensive, evidence-based review recently updated by the Public Health Service (16). However, evidence reviews conducted for the Community Guide include several interventions that might be useful to health-care providers and systems in identifying, advising, and assisting tobacco-using patients in their efforts to quit. Recommendations in the Community Guide complement those provided in the Public Health Service report (16), and both publications present a range of effective options for increasing and improving programs to help patients quit using tobacco. ADDITIONAL INFORMATION ABOUT THE COMMUNITY GUIDEDuring 2000--2001, Community Guide chapters will be prepared and released as each is completed. Upcoming chapters will focus on such topics as motor vehicle occupant injury, oral health, sexual behavior, physical activity, cancer, and the sociocultural environment. A compilation of the chapters will be published in book form. Additional information regarding the Task Force and the Community Guide is available on the Internet at <http://www.thecommunityguide.org>. References
*Tobacco-use initiation is defined as the onset, development, and establishment of tobacco- use behavior. ** Tobacco-use cessation is defined as a process that begins with the decision to stop using tobacco and ends with long-term maintenance of abstinence from tobacco. ***Consultants for the chapter on preventing tobacco use and exposure were Dileep G. Bal, M.D., California Department of Health Services, Sacramento, California; Anthony Biglan, Ph.D., Oregon Research Institute, Eugene, Oregon; Patricia A. Buffler, Ph.D., M.P.H., University of California, Berkeley, California; Gregory Connolly, D.M.D., M.P.H., Massachusetts Tobacco Control Program, Boston, Massachusetts; K. Michael Cummings, Ph.D., M.P.H., Roswell Park Institute, Buffalo, New York; Michael C. Fiore, M.D., M.P.H., University of Wisconsin Medical School, Madison, Wisconsin; David W. Fleming, M.D., CDC, Atlanta, Georgia; Sally Malek, M.P.H., North Carolina Department of Health, Raleigh, North Carolina; Patricia A, Mullen, Dr.P.H., University of Texas Health Sciences Center, Houston, Texas; Cheryl L. Perry, Ph.D., University of Minnesota, Minneapolis, Minnesota; John P. Pierce, Ph.D., University of California, San Diego, California; Helen H. Schauffler, Ph.D., University of California, Berkeley, California; Randy H. Schwartz, M.S.P.H., Maine Bureau of Health, Augusta, Maine; and Mitchell Zeller, American Legacy Foundation, Washington, DC. ****Additional information on the qualifying studies will be available at <http://www.thecommunityguide.org>. Table 1 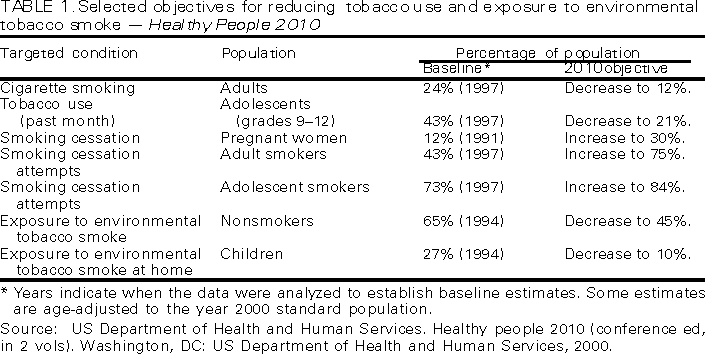 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 11/6/2000 |
|||||||||
This page last reviewed 5/2/01
|