Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail.
Brucella suis Infection Associated with Feral Swine Hunting --- Three States, 2007--2008
Historically, brucellosis from Brucella suis infection occurred among workers in swine slaughterhouses. In 1972, the U.S. Department of Agriculture National Brucellosis Eradication Program was expanded to cover swine herds. Subsequent elimination of brucellosis in commercial swine resulted in a decrease in B. suis-associated illness in humans. Currently, swine-associated brucellosis in humans in the United States is predominantly associated with exposure to infected feral swine (i.e., wild boar or wild hogs).* In May and July 2008, CDC was contacted by the state health departments in South Carolina and Pennsylvania regarding two cases of brucellosis possibly linked to feral swine hunts. Both state health departments contacted the state health department in Florida, where the hunts took place. The subsequent investigation, conducted jointly by the three state health departments and CDC, determined that the two patients had confirmed brucellosis from B. suis infection and the brother of one patient had probable brucellosis.† All three exposures were associated with feral swine hunting, and at least two patients did not have symptoms until 4--6 months after exposure (Table). The findings from this investigation suggest that clinicians treating patients with unexplained febrile illness should consider brucellosis in the differential diagnosis and obtain a thorough history of travel (e.g., to enzootic areas), food consumption, occupation, and recreational activities, including feral swine hunting. Cross-agency collaboration by state health departments and agriculture agencies is needed on brucellosis investigations to reduce the risk for illness through contact with infected animals.
Case Reports
Patient A. On May 7, 2008, a man aged 67 years from South Carolina (patient A) was referred by his private physician to a local emergency department after 1 week of fever (cyclic daily range: 99.2°--102.5°F [37.3°C--39.2°C]), malaise, anorexia, painful swollen left knee, and headaches. Patient A had a left total knee arthroplasty in 2004 and uneventful treatment in 2005 for septic arthritis in the same knee. Before onset of symptoms for his acute illness, patient A reported that he felt well except for an unintended 13-pound weight loss over a 16-week period and night sweats that began the day before he sought treatment. In the emergency department, blood and synovial fluid were obtained for culture, and the patient was empirically treated with intravenous nafcillin for septic arthritis.
Two days later, on May 9, the man was referred to a hospital with chills, persistent fever, continuing left knee arthralgia, and edema. He was admitted with a diagnosis of left knee infection and sepsis and treated initially with vancomyin. Knee aspirate cell count results were 16,700 white blood cells/mm3 (normal: <150/mm3) and 1,322 red blood cells/mm3 (normal: <1/mm3). Specimens of blood and a knee aspirate were collected for culture. Initial microbiologic examination indicated Corynebacterium urealyticum. Upon infectious disease consultation, the patient was started on doxycycline and naprosyn; on May 11, he developed epididymo-orchitis and was changed to levofloxacin and daptomycin on May 12 for a 6-week course. Brucella spp. subsequently were identified from isolates from the blood and synovial specimens collected from patient A on May 7. Isolates were sent to the South Carolina state public health laboratory and CDC for confirmatory testing. On May 29, B. suis biovar 1 was identified.
The epidemiologic investigation revealed that patient A had hunted feral swine in southwestern and south central Florida with two companions during December 23--29, 2007. All three participated in field dressing and butchering eight or nine feral swine at two locations. While field dressing one of the swine, patient A cut his hand with a knife. No personal protective equipment was worn during the field dressing and butchering. The meat was brought back to South Carolina, stored in a freezer, and boiled before being consumed by patient A over several months. No one else prepared or ate the meat, and no meat was collected for testing. No other risk factors for brucellosis were identified.
Because patient A's hunting companions were well, serologic testing for brucellosis was not performed. Patient A recovered with no permanent knee joint damage after antimicrobial therapy with levofloxacin and daptomycin for 6 weeks.
Patient B. On July 14, 2008, a previously healthy man aged 37 years from Pennsylvania (patient B) went to a local emergency department after 1 week of morning fevers, chills, myalgia, shortness of breath, and night sweats. He also reported an unintended 30-pound weight loss over a 1-month period, beginning 3 weeks before illness onset. A blood chemistry profile was within normal limits with the exception of glucose of 121 mg/dL (normal: 74--100 mg/dL). A complete blood cell count was within normal limits with the exception of mean platelet volume of 7.2 fL (normal: 7.4--10.4 fL); eosinophils on the differential were 0.2% (normal: 0.7%--5.2%). Urinalysis was positive for trace white blood cell esterase and for a white blood cell count of 1--4/mm3 (normal: 0--1/mm3). A chest radiograph was within normal limits, and a blood specimen for culture was obtained.
Clinical impression was acute viral syndrome; patient B was discharged with instructions to use an albuterol metered-dose inhaler three times daily for 1--2 days for his shortness of breath and to follow up with his private physician in 2--3 days. On July 23, the Pennsylvania state public health laboratory received patient B's blood specimen from the local hospital and isolated and identified B. suis using Laboratory Response Network§ standardized biochemical tests and polymerase chain reaction.
Epidemiologic investigation revealed that, on December 29, 2007, patient B had hunted feral swine in Florida with his brother (patient C), a Florida resident. Both men participated in field dressing and butchering four feral swine. No personal protective equipment was worn during these procedures, and no other risk factors for brucellosis were identified. Patient B brought the meat back to Pennsylvania and stored it in a freezer. The meat was prepared and consumed by patient B and his family members over a 7-month period. According to patient B, the meat was cooked adequately (i.e., to an internal temperature of 160°F [71.1°C]).
CDC received three B. suis isolates for confirmation and further molecular characterization. One isolate was from the blood of patient B, and the other two were recovered from frozen sausage and tenderloin of a feral swine from the December 29 hunt. All three B. suis isolates were analyzed at CDC by molecular genotyping assay, using multiple-locus variable-number tandem repeat analysis. The assay indicated that the two meat isolates had identical signatures at all of the 15 genomic markers, and the patient B isolate matched the meat isolates at all but one of 15 markers, suggesting that the three isolates were linked.
Patient B reported that his wife and children were not ill; however, his brother (patient C) had experienced similar symptoms in April. Although asymptomatic, initial serologic testing for brucellosis was performed on all household family members, and no antibody elevation was noted. Patient B recovered after 6 weeks of treatment with rifampin and doxycycline.
Patient C. In August, the Pennsylvania state health department reported the association between patient B's infection and feral swine hunting to the Florida state health department, which, on August 21, contacted patient C (patient B's brother who had accompanied him on feral swine hunts). At the time, neither patient C nor his family members reported experiencing symptoms of brucellosis. However, patient C recalled feeling ill in April with night sweats and shortness of breath. He did not seek treatment because he attributed his symptoms to a recent scorpion sting.
Other than feral swine hunting, no other brucellosis risk factors were identified for patient C. He reported that all the meat he received from the December 2007 feral swine hunts was either smoked, roasted, or barbequed and was consumed at one family cookout. On September 12, a serum specimen from patient C was tested at CDC for anti-Brucella antibodies using the Brucella microagglutination test. The resulting immunoglobulin G titer of 1:640 met the case definition for probable brucellosis.
Because patient C's family was well, serologic testing for brucellosis was not performed. Treatment was recommended for patient C, but he was lost to follow-up.
Reported by: D Giurgiutiu, MD, C Banis, South Carolina Dept of Health and Environmental Control. E Hunt, MPH, J Mincer, C Nicolardi, A Weltman, MD, Pennsylvania Dept of Health. D Stanek, DVM, S Matthews, MPH, C Siegenthaler, C Blackmore, DVM, Florida Dept of Health. R Tiller, MPH, B De, PhD, Div of Foodborne, Bacterial, and Mycotic Diseases, National Center for Zoonotic, Vector-Borne, and Enteric Diseases; K Stauffer, DVM, EIS Officer, CDC.
Editorial Note:
Brucellosis is a bacterial zoonotic infection usually caused by Brucella abortus, B. melitensis, B. suis, or rarely B. canis. Humans are infected through occupational or recreational exposure to infected animals, inhalation of infectious aerosols, laboratory exposure (1), consumption of contaminated unpasteurized dairy products, or consumption of inadequately cooked contaminated meat. The average incubation period for brucellosis is 2--10 weeks but, as seen in this report, can range to 6 months. Symptoms can be nonspecific and influenza-like: intermittent fever, chills, malaise, diaphoresis, arthralgia, myalgia, headache, anorexia, and fatigue (2,3). Because of its nonspecific clinical syndrome, B. suis infection likely is underreported. Clinicians should inquire about travel, food consumption, occupation, and recreational activities (including feral swine hunting) of patients with nonspecific influenza-like symptoms with intermittent fever.
Patient A likely was infected through the hand wound he acquired while field dressing feral swine. The investigations suggest that patient B and patient C also were infected during the field dressing or butchering process because family members consumed the meat and were not affected clinically. Clinicians should order brucellosis testing for persons who are symptomatic and have a history of feral swine hunting. Duration and type of therapy is dependent upon multiple factors such as health status or age of patient and the manifestation of disease. Untreated brucellosis can last from several weeks to several years. Chronic untreated brucellosis can lead to abscesses in the liver, spleen, heart valves, brain, or bone; osteoarticular complications; and, in rare cases, death (2,3).
Human brucellosis is a nationally notifiable disease in all 50 states, New York City, the District of Columbia, and all U.S. territories except Puerto Rico. In 2007, 131 brucellosis cases were reported in the United States (Figure). States with the highest numbers of reported cases were California (33), Texas (25), and Florida (10) (4).
Feral swine have been reported in 35 states (J. Corn, PhD, personal communication, Southeastern Cooperative Wildlife Disease Study, 2009). The national feral swine population is estimated at approximately 4--5 million, with the largest populations in Texas (1.5 million), California, Florida, and Hawaii. Serologic surveys have detected endemic feral swine infection with B. suis in 10 states (Arkansas, California, Florida, Georgia, Hawaii, Louisiana, Mississippi, Missouri, South Carolina, and Texas) (5--9). Feral swine hunting is allowed in most states with feral swine presence, and most states require some form of license to hunt feral swine. Out-of-state hunters, as in this report, often bring swine meat back to their home states.
Efforts to prevent B. suis infection should focus on education of hunters and partnerships between state and local public health, wildlife, and agricultural agencies, and sportsmen's associations. Educational materials for feral swine hunters should include recommendations for safe field dressing, butchering, and cooking (9). All human brucellosis cases should be investigated jointly by state health departments and agriculture agencies to determine the sources of infection and prevent further illness in humans.
Acknowledgments
This report is based, in part, on contributions by D Donch, DVM, Veterinary Svcs, S Swafford, MS, Wildlife Svc, Animal and Plant Health Inspection Svc, US Dept of Agriculture; J Corn, PhD, Southeastern Cooperative Wildlife Disease Study; M Piergallini, MD, practitioner; and S Weber, MD, Susquehanna Health Medical Group.
References
- CDC. Laboratory-acquired brucellosis---Indiana and Minnesota, 2006 MMWR 2008;57:39--42.
- Glynn MK, Lynn TV. Brucellosis. J Am Vet Med Assoc 2008;233:900--8.
- Mandell GL, Bennett JE, Dolin R. Brucella species [Chapter 223]. In: Mandell, Douglas, and Bennett's principles and practice of infectious diseases. 6th ed. Philadelphia, PA: Elsevier Inc.; 2005:2669--74.
- CDC. Summary of notifiable diseases---United States, 2007. MMWR 2009;56(53). In press.
- Gresham CS, Gresham CA, Duffy MJ, Faulkner CT, Patton S. Increased prevalence of Brucella suis and pseudorabies virus antibodies in adults of an isolated feral swine population in coastal South Carolina. J Wildl Dis 2002;38:653--6.
- Stoffregen WC, Olsen SC, Wheeler CJ, et al. Diagnostic characterization of a feral swine herd enzootically infected with Brucella. J Vet Diagn Invest 2007;19:227--37.
- van der Leek ML, Becker HN, Humphrey P, et al. Prevalence of Brucella sp. antibodies in feral swine in Florida. J Wildl Dis 1993;29:410--5.
- Zygmont SM, Nettles VF, Shotts EB, et al. Brucellosis in wild swine: a serologic and bacteriologic survey in the southeastern United States and Hawaii. J Am Vet Med Assoc 1982;181:1285--7.
- Animal and Plant Health Inspection Service, US Department of Agriculture. Feral/wild pigs: potential problems for farmers and hunters. Agriculture information bulletin no. 799. Washington, DC: US Department of Agriculture; 2005. Available at http://www.aphis.usda.gov/publications/wildlife_damage/content/printable_version/feral%20pigs.pdf.
* Swine that have lived any part of their lives as free-roaming animals.
† Probable: a clinically compatible case that is epidemiologically linked to a confirmed case or that has supportive serology (i.e., Brucella agglutination titer of ≥160 in one or more serum specimens obtained after onset of symptoms). Confirmed: a clinically compatible illness that is laboratory confirmed. Laboratory criteria for diagnosis: 1) isolation of Brucella spp. from a clinical specimen, 2) fourfold or greater rise in Brucella agglutination titer between acute- and convalescent-phase serum specimens obtained ≥2 weeks apart and studied at the same laboratory, or 3) demonstration by immunofluorescence of Brucella spp. in a clinical specimen. Case definitions available at http://www.cdc.gov/ncphi/disss/nndss/casedef/brucellosis_current.htm.
§ Additional information available at http://www.bt.cdc.gov/lrn.
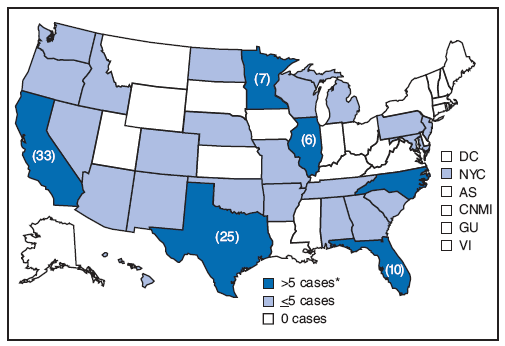
SOURCE: CDC. Summary of notifiable diseases---United States, 2007. MMWR 2009;56(53). In press.
* Actual totals for states with >5 cases are shown in parentheses.
Alternative Text: The figure above is a U.S. map showing reported cases of brucellosis in the United States in 2007 by state. A total of 131 cases were reported, with the highest numbers of reported cases were California (33), Texas (25), and Florida (10).
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services. |
All MMWR HTML versions of articles are electronic conversions from typeset documents. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr) and/or the original MMWR paper copy for printable versions of official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Date last reviewed: 6/10/2009


