Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail.
Outbreak of Cryptosporidiosis Associated with a Splash Park --- Idaho, 2007
Please note: Errata have been published for this article. To view the errata, please click here and here.
On August 6, 2007, Idaho's Central District Health Department (CDHD) received a complaint of several ill persons with watery diarrhea consistent with cryptosporidiosis after attendance at a municipal splash park on July 26. Cryptosporidium spp. is a protozoan that causes diarrheal illness and has been implicated previously in recreational water illness outbreaks at splash parks (1--3). CDHD and the Idaho Department of Health and Welfare (IDHW) initiated an investigation of illness among municipal park visitors who attended reservation-only gatherings at an onsite pavilion July 23--August 10. The investigation revealed five immunofluorescence assay (IFA)-confirmed and 45 clinically compatible cases of cryptosporidiosis among 154 persons interviewed (32% attack rate). Patients were more likely than non-ill park visitors to have been exposed to water from a splash feature (relative risk [RR] = 4.7). Water samples collected from splash features and an adjacent drinking fountain tested positive for Cryptosporidium hominis. This report summarizes the investigation of the outbreak and highlights the importance of splash park design, operation, access to hygiene facilities, and public education in prevention of waterborne cryptosporidiosis and other infectious agents. Educational efforts and enactment of regulations requiring enhanced disinfection technology, exclusion of persons with diarrhea, adequate hygiene facilities, and preconstruction consultation with health departments might decrease the risk for recreational water illness at splash parks.
The exposures occurred at a recently constructed splash park located within a municipal park in a suburban community in Idaho with a surrounding population of 550,000. Splash parks are increasingly popular venues associated with recreational water illness (1--4) and are often easily accessible, unmonitored, and charge no admission (5). Splash parks have multiple, interactive water features that spray, splash, or pour water on visitors, without pools or standing water. Typically, a municipal system supplies the water, which flows from the features onto impermeable surfaces (e.g., concrete), through drains, and recirculates through high-flow sand filters back to the water features. In Idaho, splash park design, construction, and operation are not regulated by the Idaho pool code.
The initial investigation by CDHD and IDHW began on August 7 with interviews of 20 persons who attended a party at the splash park on July 26. Among those 20 persons, 12 reported gastrointestinal illness that began August 1--6 (6--11 days after exposure), including eight persons who reported watery diarrhea. All 12 ill persons reported exposure to splash-feature water, and six reported exposure to water from a nearby drinking fountain. No food items at the party were implicated as the source of the outbreak. Investigators hypothesized that swallowing contaminated splash park water was the source of illness.
To find additional cases, identify risk factors, and implement control measures, CDHD and IDHW initiated telephone interviews of municipal park visitors who attended reservation-only gatherings at an onsite pavilion July 23--August 10, the only dates for which reservation listings were available. Reservations for 12 separate groups encompassing approximately 600 persons were identified. Information about visitors without reservations was not recorded by the municipal park; consequently, the total number of visitors during the study period could not be determined. To enable prompt intervention, interviews were limited to the first 154 respondents contacted, representing nine (75%) of the 12 reservation parties. Respondents were contacted in order of their position on the reservation listings.
A clinical case was defined as the onset of diarrhea (three or more loose stools in 24 hours) or four or more symptoms consistent with gastroenteritis (i.e., abdominal cramps, nausea, vomiting, fever, or body aches) in a person within 1--12 days after visiting the municipal park. A confirmed case was defined as illness in a person with a positive IFA stool test result for Cryptosporidium. Non-ill park visitors were identified from attendees who did not meet either case definition. Study participants were administered a standardized questionnaire by telephone.
The 154 respondents represented 51 separate households and 12 different days of exposure. For respondents reporting multiple days of exposure to the municipal park, the latest day of exposure was used for the analysis. Fifty (32%) of 154 attendees had illness meeting the clinical (n = 45) or confirmed (n = 5) case definition; 26 (52%) were males (Table 1). The median age of patients was 7 years (range: 10 months--58 years). Illness onset ranged from July 28 to August 20 (Figure), and the median time from exposure to onset of illness was 6 days (range: 1--14 days). One patient with a confirmed case reported splash park exposure on August 1 and illness onset August 15. Among 29 patients whose illness was resolved at the time of interview, the median duration of illness was 3 days (range: 1--9 days). The most common symptoms reported were diarrhea (86%), vomiting (64%), abdominal cramps (62%), nausea (62%), fever (52%), headache (46%), and body aches (40%). No hospitalizations or deaths associated with illness were reported. Treatment information for patients was not available.
A retrospective cohort analysis was used to identify risk factors for illness, after combining confirmed and clinical cases. Patients were more likely to have been exposed to splash-feature water only than were non-ill persons (RR = 4.7; 95% confidence interval [CI] = 1.8--11.9) (Table 2). Patients also were more likely to report exposure to both splash-feature water and adjacent drinking fountain water than were non-ill persons (RR = 8.6; CI = 3.2--23.3). In a second analysis, to limit the possibility of including secondary cases in the risk factor analysis, household contacts who also had visited the municipal park were excluded if they reported exposure to the splash park after August 4 or illness onset >4 days after the household index case. The remaining household patients (n = 32) were more likely to have been exposed to the splash park (RR = 18.4; CI = 2.6--128.2) and to an adjacent drinking fountain (RR = 1.5; CI = 1.1--2.0) than were non-ill persons.
An environmental investigation was begun August 9. During an initial site inspection, young children were observed to be the predominant users of the splash park, and diapered children frequently sat on top of splash features. Soap was not available in nearby restrooms, nor were showers. Public health education signs were not posted at the park. The splash park did not have any standing water; investigators noted that water drained from a concrete deck, passed through a high-flow sand filter, and was chlorinated before recirculation through several splash features.
On August 9, CDHD collected water samples from the splash park, and those samples were analyzed for total coliforms and Escherichia coli using the 9223B substrate Colilert method. Water samples collected on August 20 from the high-flow sand filter backwash and adjacent drinking fountain were tested at the Environmental Protection Agency (EPA) Region 10 laboratory following EPA method 1623* (6). C. hominis was identified in the sample by polymerase chain reaction-restriction fragment length polymorphism analysis of the 18S rRNA gene in DNA extracted from microscopy-positive slides. Oocysts in both samples were further subtyped by DNA sequencing of the gp60 gene as IaA28R4 (7). Two Cryptosporidium isolates from patients also were genotyped and subtyped C. hominis IaA28R4.
The splash park was closed August 17, and the municipal park drinking fountains were turned off August 23. An engineering investigation determined no source of drinking water contamination; however, after the outbreak, two return backflow-prevention devices designed to prevent retrograde flow of splash park water into municipal water lines failed inspection and were replaced. Although the municipal water supply is maintained at a higher pressure than the splash park, a decrease in water pressure could have allowed a potential retrograde flow of contaminated water into the municipal water line. Repeat testing of the drinking-fountain water on August 29 and upstream municipal water on August 31 yielded no Cryptosporidium oocysts. The drinking fountains were turned back on September 11. The municipality reopened the splash park in 2008 after installation of an ultraviolet treatment system, improvement of hygiene facilities, hiring of attendants to monitor for nonhygienic behaviors by visitors, and posting of educational signs instructing visitors not to drink the splash-feature water.
Reported by: R Jue, T Schmalz, Central District Health Dept, Idaho. K Carter, DVM, Coordinating Office for Terrorism Preparedness and Emergency Response; RJ Nett, MD, EIS Officer, CDC.
Editorial Note:
Cryptosporidium, a chlorine-resistant parasite, can cause illness after ingestion of as few as 10 oocysts, and can remain infectious for up to 6 months in moist environments (8). In this outbreak investigation, detection of identical subtypes of C. hominis, a species primarily restricted to humans (9), in the stool specimens of patients and in water samples from the sand filters and drinking fountain implicated ingestion of fecally contaminated splash-feature and drinking fountain water as the cause of the illnesses. Because reported exposures occurred during July 23--August 10 and splash park water collected on August 20 tested positive for Cryptosporidium, initial contamination of splash park water by an ill visitor likely caused persistent contamination of the splash park system and resulted in ongoing transmission. Similar outbreaks have occurred at other splash parks that lacked ultraviolet or ozone treatment systems that can inactivate Cryptosporidium (1,3). Splash park operators cannot rely solely upon high-flow sand filtration and chlorine disinfection to protect patrons from Cryptosporidium.
The findings in this report are subject to at least four limitations. First, reservations at the on-site pavilion represented a small percentage of daily attendance at the splash park; the total number of visitors to the splash park during the study period could not be determined, nor could the total number of cryptosporidiosis cases associated with the splash park among nontallied visitors. Second, limited staff resources might have led to selection bias by restricting interviews to those persons able to be contacted most quickly, perhaps biasing the study toward persons more likely to be at home and ill. Third, a statewide cryptosporidiosis outbreak involving multiple recreational water venues was occurring at the same time as the municipal splash park outbreak, and ill persons might have been exposed to other contaminated sources of recreational water, potentially confounding the results. Finally, despite an engineering investigation, the specific source of drinking water contamination could not be determined. Although failed backflow prevention devices might have allowed contaminated splash park water to enter the municipal drinking water line supplying the drinking fountain, most ill person (27/40) did not have exposure to the drinking fountain.
The outbreak described in this report involved a recently constructed, unregulated splash park, with contributing factors related to design and operation that prior consultation with health department staff might have identified and corrected. State and local governments should consider including splash parks in the pool code and requiring preconstruction health department consultation, supplemental disinfection technology (e.g., ultraviolet light), appropriate hygiene facilities, and education of splash park operators and the public. Furthermore, research on splash park design and operation is needed to develop engineering and operational guidelines specific to these facilities.
Regulation without education is unlikely to reduce substantially the risk for recreational water illness outbreaks. Splash parks are relatively new, and operator knowledge of appropriate disinfection and maintenance requirements might be inadequate (10); public health officials and industry associations should make regular efforts to educate operators. Additionally, splash park operators and public health officials should work jointly to educate visitors about prevention of recreational water illness. Persons using splash park and other water park facilities are the primary source of contamination, and even water in well-maintained and treated recreational water venues can transmit Cryptosporidium. Posted signs should guide patrons to wash young children's bottoms with soap in the shower before splash park entry, refrain from drinking the splash-feature water, discourage children from sitting on top of splash features, and change diapers only in designated areas. Persons with diarrhea should be prohibited from entering recreational water venues. Behavioral restrictions, however, might not be enforceable at splash parks that have unrestricted and unmonitored public access.
Acknowledgments
The findings in this report are based, in part, on contributions by H Ezell, D Irons, F Isenberg, B Tramontin, Central District Health Dept; E Huffe, City of Meridian; C Greenwalt, C Hahn, MD, S Mundt, S Radwin, T Shanahan, K Turner, K Vlcek, E Zager, Idaho Dept of Health and Welfare; D Lee, Idaho Dept of Environmental Quality; S Bailey, G Dodo, S Harris, DVM, J Parker, Environmental Protection Agency; M Beach, PhD, M Hlavsa, J Yoder, and L Xiao, DVM, PhD, National Center for Zoonotic, Vector-Borne and Enteric Diseases, and K Bisgard, DVM, Office of Workforce and Career Development, CDC.
References
- CDC. Outbreak of gastroenteritis associated with an interactive water fountain at a beachside park---Florida, 1999. MMWR 2000;49:565--8.
- Jones M, Boccia D, Kealy M, et al. Cryptosporidium outbreak linked to interactive water feature, UK: importance of guidelines. Euro Surveill. 2006;11:126--8.
- Schaffzin JK, Keithly J, Johnson G, et al. Large outbreak of cryptosporidiosis associated with a recreational water spraypark---New York, 2005 [Abstract]. Proceedings of the 55th Annual Conference of the Epidemic Intelligence Service; 2006; Atlanta, GA: US Department of Health and Human Services, CDC; 2006.
- CDC. Surveillance for waterborne-disease outbreaks---United States, 1997--1998. MMWR 2000;49(No. SS-4).
- Kebabjian RS. Interactive water fountains: the potential for disaster. J Environ Health 2003;66:24, 29--30.
- Environmental Protection Agency. Method 1623: Cryptosporidium and Giardia in water by filtration/IMS/FA. Washington, DC: Environmental Protection Agency, Office of Water; 2005. Available at http://www.epa.gov/nerlcwww/1623de05.pdf.
- Xiao L, Ryan UM. Molecular epidemiology. In: Fayer R, Xiao L, eds. Cryptosporidium and cryptosporidiosis. 2nd ed. Boca Raton, FL: CRC Press and IWA Publishing; 2008:119--71.
- Huang DB, White AC. An updated review on Cryptosporidium and Giardia. Gastroenterol Clin North Am 2006;35:291--314, viii.
- Morgan-Ryan UM, Fall A, Ward LA, et al. Cryptosporidium hominis n. sp. (Apicomplexa: Cryptosporidiidae) from Homo sapiens. J Eukaryot Microbiol 2002;49:433--40.
* EPA method 1623 (available at http://www.epa.gov/microbes/1623de05.pdf) is a laboratory method for detection of the genera Cryptosporidium and Giardia by use of concentration, immunomagnetic separation, and immunofluorscence assay microscopy.
FIGURE. Number of cryptosporidiosis cases,* by dates of exposure at a municipal splash park and illness onset --- Idaho, July--August 2007
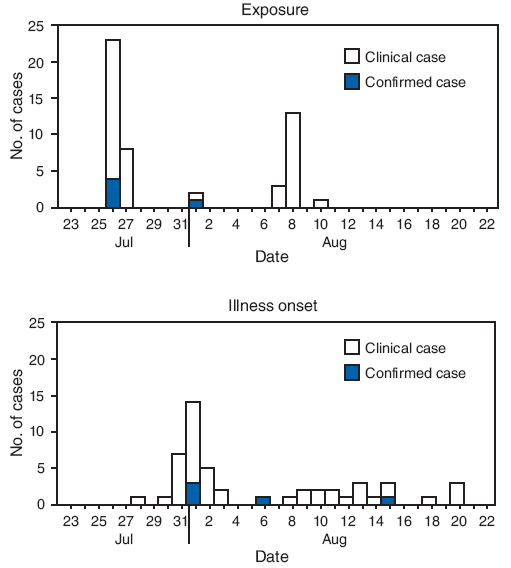
* A clinical case of cryptosporidiosis was defined as three or more loose stools in 24 hours, or four or more symptoms consistent with gastroenteritis (i.e., abdominal cramps, nausea, vomiting, fever, or body aches) in a person within 1--12 days after visiting the municipal park. A confirmed case was defined as illness in a person with an immunofluorescence assay positive stool test result for Cryptosporidium.
Alternative Text: The figure above shows the number of cryptosporidiosis cases, by dates of exposure at a municipal splash park and illness onset in Idaho from July through August 2007. Most of the exposures that were investigated occurred July 26. For most clinical and confirmed cases, illness onset occurred August 1. The median time from exposure to onset of illness was 6 days (range: 1-14 days).
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services. |
All MMWR HTML versions of articles are electronic conversions from typeset documents. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr) and/or the original MMWR paper copy for printable versions of official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Date last reviewed: 6/10/2009


