 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Racial Disparities in Total Knee Replacement Among Medicare Enrollees --- United States, 2000--2006An estimated 45% of U.S. adults might be at risk for developing symptomatic knee osteoarthritis during their lifetimes, with whites and blacks at equal risk for this common disabling condition (1). Total knee replacement (TKR) is an effective method of reducing pain and improving physical function among those with disabling knee osteoarthritis; however, whites have been more likely to undergo the procedure than blacks (2--4). As a result, a Healthy People 2010 objective* calls for eliminating racial disparities in the rate of TKR among persons aged >65 years (5). To monitor progress toward achieving this objective, CDC analyzed national and state TKR rates for Medicare enrollees for the period 2000--2006, stratified by sex, age group, and black or white race. From 2000 to 2006, the TKR rate overall in the United States increased 58%, from 5.5 to 8.7 per 1,000 population, with similar increases among whites (61%) and blacks (56%). However, the TKR rate for blacks was 37% lower than the rate for whites in 2000 (3.6 versus 5.7 per 1,000 population) and 39% lower in 2006 (5.6 versus 9.2 per 1,000 population). Health-care providers and public health agencies might help reduce this disparity by widely distributing TKR information that is tailored to the education and literacy levels and culture of patients with symptomatic knee osteoarthritis. Health-care providers should conduct, as routine practice, thorough discussions regarding knee pain symptoms and loss of physical function with older patients of all races who might be candidates for TKR (2). National and state TKR rates for Medicare enrollees were calculated using 2000--2006 hospital claims and enrollment record data obtained from the Centers for Medicare and Medicaid Services. Analysis was restricted to U.S. residents in the 50 states and District of Columbia (DC) who were aged >65 years, entitled to Medicare Part A, and not members of managed care organizations. TKR rates were calculated per 1,000 members of this group, using population estimates on July 1 of the given year. Eligible TKR procedures were defined as International Classification of Diseases, Ninth Revision, Clinical Modification code 81.54 (total knee replacement) on hospital claims records from acute care, short-term hospitals. Partial knee replacements were excluded because they represent only 8% of all knee replacement procedures (6). Annual TKR rates and 95% confidence intervals were calculated for adults aged >65 years overall and by age group (65--74, 75--84, and >85 years), sex, black or white race, and state. For this report, estimates by race are presented only for blacks and whites because Medicare race/ethnicity data for other populations (e.g., Asians and Hispanics) are underreported and might produce misleading results (7). Unadjusted national and state estimates were calculated to describe the actual disparity in each jurisdiction for program planning and resource allocation (8). Age-adjusted national rates using the 2000 projected U.S. population† also were calculated to monitor the trend in TKR black/white disparity. Percentage changes in TKR rates from 2000 to 2006 were calculated for blacks and whites, and percentage differences between blacks and whites undergoing TKR were calculated for both years. In 2000, a total of 26,585,955 Medicare enrollees met the study inclusion criteria; in 2006, the total was 28,382,683. The number of hospitalizations for TKR among Medicare enrollees in the study increased from 145,242 in 2000 to 248,267 in 2006 (Table 1), and the overall TKR rate increased 58% (from 5.5 to 8.7 per 1,000 population). Similar increases were observed by sex, age group, and black or white race (Table 1). In both years, the total number of procedures performed was highest among those aged 65--74 years, but the TKR rate was highest among those aged 75--84 years. TKR rates increased in all states from 2000 to 2006, with the greatest increases in Arkansas (84%), Mississippi (84%), and Delaware (83%), and the lowest increases in Iowa (35%), New Mexico (35%), and Idaho (38%). In 2006, TKR rates ranged from 13.9 in Utah to 4.5 in Hawaii. TKR rates were 37% lower among blacks than whites (3.6 versus 5.7 per 1,000 population) in 2000, and 39% lower in 2006 (5.6 versus 9.2) (Table 2, Figure). In both years, the black/white disparity was lower among women (23% and 28%) than among men (63% and 60%). In 2006, blacks had a lower TKR rate than whites in all 50 states and DC; the smallest black/white disparities were in DC (11%), Delaware (18%), Massachusetts (18%), and Nevada (18%), and the largest were in Illinois (52%) and Pennsylvania (49%). From 2000 to 2006, the black/white disparity increased across all three age groups, among women (but not among men), and in 19 states (Table 2). Reported by: MG Cisternas, MA, MGC Data Svcs, Carlsbad, California. L Murphy, PhD, JB Croft, PhD, CG Helmick, MD, Div of Adult and Community Health, National Center for Chronic Disease Prevention and Health Promotion, CDC. Editorial Note:Racial disparity in TKR procedures is an important social and public health problem, underscored by adoption of a Healthy People 2010 objective to eliminate racial disparities in TKR procedures. The findings in this report, however, confirm that little or no progress was made toward achieving this objective from 2000 to 2006. Although the numbers and rates of TKR procedures increased among Medicare enrollees in all demographic groups from 2000 to 2006, the disparity in rates between whites and blacks persisted in the nation overall and increased in 19 states. The findings of an increase in the overall rate of TKR procedures in the United States and the substantial and continuing black/white disparities in TKR are consistent with previous reports. One report examining rates of knee and hip replacement, bypass surgery, and angioplasty from 1997 to 2001 in New York and Pennsylvania Medicare populations found an increase in the white/nonwhite disparity for joint replacements (9). An analysis of 1998--2000 Medicare data also indicated racial disparity in TKR rates (3). Rates in that study differ somewhat from those in this report, likely because of the substantial increase in the number of TKR procedures since 2000, the different geographic areas examined (i.e., nation and state compared with selected hospital referral regions), and restriction of the study population in this report to Medicare enrollees aged >65 years who were not in a managed care organization, instead of the entire Medicare enrollee population. The precise causes of black/white disparities in TKR are unclear and likely multifactorial. The disparities are not explained by varying risk for knee osteoarthritis (1). Likewise, disparate access to health care probably does not explain the disparities. Several reports have indicated that racial disparity in TKR procedures persists even after adjusting for access to clinical care (2). However, differing knowledge, attitudes, and beliefs regarding TKR might play some role. Lower outcome expectations have been associated with unwillingness to undergo TKR; these lower expectations might result from communication gaps with health-care providers or inaccurate information from peers (2). Also, the likelihood of undergoing a joint replacement increases if a member of the patient's social network has undergone a successful joint replacement (2). Although no evidence has been presented showing racial differences in functional status after undergoing TKR, non-white Medicare beneficiaries are more likely to undergo surgery in hospitals that have fewer TKR procedures and where adverse TKR outcomes are more common (10). Negative TKR outcomes might influence members of social networks not to seek TKR. The likelihood of undergoing TKR increases with increased education (2). One study of U.S. adults found racial disparity in joint replacement use during 1998--2004 among persons aged >65 years but not among persons aged 51--64 years (4), a difference that might be attributable, in part, to a narrower education gap between blacks and whites at younger age levels. The findings in this report are subject to at least three limitations. First, the study data were collected from Medicare hospital claims and thus depend on the accuracy of physician or administrative reporting and procedure coding. However, these data are the only available national source of hospital procedure information with complete black and white race data for persons aged >65 years. Second, all hospitalizations were analyzed, but access to individual identifiers was prohibited; therefore, some persons might have been counted twice if they underwent TKR surgery on each knee at two separate times in the same year. Finally, the analysis does not include persons in managed care organizations, a standard exception in Medicare analyses, because these organizations do not release specific claims data; in 2004, approximately 17% of all Medicare enrollees were members of managed care organizations. Racial disparity between blacks and whites persists in TKR procedures, and the precise underlying reasons are unclear. A combined public health and clinical strategy to address racial disparity in TKR might include wider distribution of information in various public settings and equipping health-care providers with resources that enable them to have TKR discussions that are thorough and tailored to the understanding, needs, and concerns of their patients (2). References
* The initial Healthy People objective was developmental and lacked a baseline and target to enable measurement of progress. That objective read, "Eliminate racial disparities in the rate of total knee replacements." In 2006, the objective was revised to read, "Eliminate racial disparities in the rate of total knee replacements among persons aged 65 years and older. Target: 0 percent." † Additional information available at http://www.cdc.gov/nchs/data/statnt/statnt20.pdf. Table 1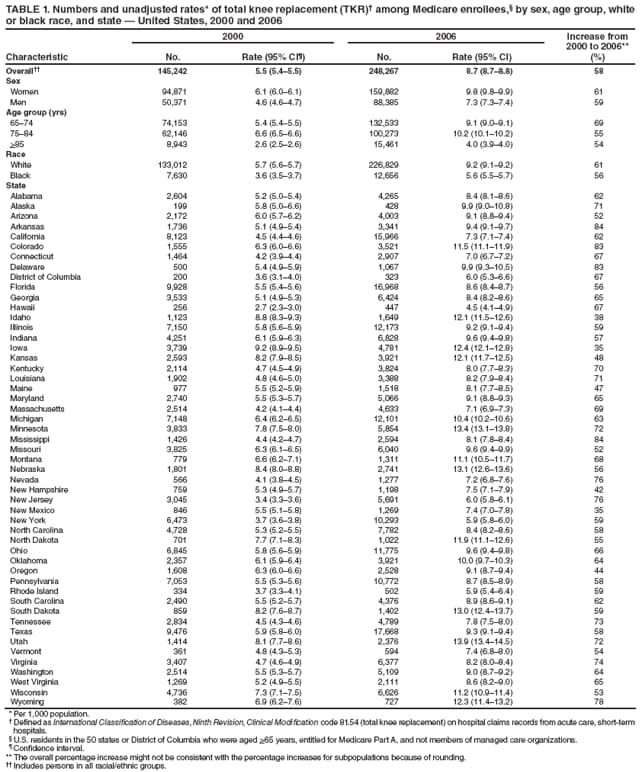 Return to top. Table 2  Return to top. Figure  Return to top.
All MMWR HTML versions of articles are electronic conversions from typeset documents. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr) and/or the original MMWR paper copy for printable versions of official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Date last reviewed: 2/19/2009 |
|||||||||
|