 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Worker Illness Related to Ground Application of Pesticide --- Kern County, California, 2005In California, suspected pesticide and work-related illnesses and injuries are reportable conditions. The Occupational Health Branch (OHB) of the California Department of Health Services (CDHS) conducts surveillance of work-related pesticide illness with support from the National Institute for Occupational Safety and Health (NIOSH) and the U.S. Environmental Protection Agency (EPA). On May 12, 2005, CDHS received a report from the California Department of Pesticide Regulation (CDPR) of a suspected pesticide incident in Kern County involving 27 farmworkers (age range: 21--61 years; median: 32.5 years) and six emergency responders (age range: 28--51 years; median: 33.5 years). CDHS investigated this incident by conducting a site visit; reviewing medical and meteorologic records; and interviewing affected workers, pesticide applicators, and the farmworker employer. Findings indicated that workers became ill from drift of a pyrethroid pesticide (cyfluthrin) that was being applied in a neighboring field. Pyrethroid pesticide applicators should always operate in a manner that ensures workers are not exposed. On May 12 at 7:00 a.m., a commercial pesticide application team was spraying in a citrus orchard to control thrip, a small insect that feeds on oranges. The pesticide solution contained 32 ounces of cyfluthrin (pyrethroid, EPA toxicity category I), 84 ounces of spinosad (EPA toxicity category III), 18.5 gallons of petroleum oil (EPA toxicity category III), and 1,800 gallons of water. The pesticide was sprayed from three enclosed ground rig applicator tractors that traveled up and down rows and turned around on a dirt road that borders the field. In a neighboring grape vineyard southeast of the pesticide application, 27 farmworkers (23 female) were suckering (i.e., pruning unwanted shoots), lifting, and tying grape vines. Although employers are required by CDPR to notify their workers when they are within a quarter mile of cyfluthrin application, notification of farmworkers in the neighboring vineyard was not required because they worked for a different employer. A supervisor for the pesticide applicators observed the workers in the grape vineyard and suspended application. The applicator supervisor spoke with the farmworker supervisor, but the substance of their conversation is unknown. The farmworkers continued to work, and spraying resumed approximately 20 minutes later. Shortly thereafter, some of the workers noticed a chemical odor, began feeling ill, and stopped working. A 911 telephone call was made, and a hazardous material (HAZMAT) team arrived at 7:55 a.m. Twenty-three workers (all female) were decontaminated on site by the HAZMAT team. They were then transported by ambulances to local hospitals. Four other workers (all male), who had been lifting grape vines in a location further from the spraying, were identified later that day and transported by their supervisor to medical care the following day as a precaution. After evaluation in emergency departments, all 27 farmworkers were discharged home. CDHS conducted in-person interviews in Spanish with the farmworkers and telephone interviews in English with the emergency responders and reviewed medical records from emergency department and clinic visits. Data were abstracted and coded according to a standardized case definition for pesticide-related illness (1). Symptoms most commonly reported by the 27 farmworkers were headache (96%), nausea (89%), eye irritation (70%), muscle weakness (70%), anxiety (67%), and shortness of breath (64%) (Table). Illness severity was classified according to a severity index for acute pesticide-related illness (2). Illness severity was moderate in five (19%), low in 20 (74%), and not applicable (i.e., less than two symptoms) in two (7%) farmworkers (2). Because of the known toxicity of the different substances applied, these effects were attributed primarily to cyfluthrin. Illness symptoms were not reported by the applicators, who were wearing appropriate protective equipment. Foliage samples obtained by CDPR from the citrus orchard southeast of the pesticide spraying indicated cyfluthrin levels of 1.14 ppm. Neither foliage samples obtained from the grape vineyard nor clothing samples obtained from the farmworkers had measurable levels of cyfluthrin. CDHS is conducting follow-up with these workers to assess any potential persistent effects associated with acute cyfluthrin exposure. Six emergency responders (four male) responded to the incident and were evaluated in emergency departments. Health effects were reported by four of six emergency responders and included respiratory (four), skin (three), and eye (two) symptoms. The illness severity rating was low in four of six emergency responders and, in two others, was not applicable (2). Reported by: R Das, MD, B Materna, PhD, Occupational Health Branch, G Windham, PhD, Environmental Health Investigations Branch, California Dept of Health Services. J Beckman, M Marcellini, MS, Public Health Institute, Oakland, California. K Carrigan, MD, Univ of California, San Francisco. M Ibarra, California Dept of Pesticide Regulation. A Sumner, MD, EIS Officer, CDC. Editorial Note:The incident described in this report highlights two potential occupational hazards in agriculture: pyrethroid toxicity and pesticide drift. In this incident, drift of the pyrethroid compound cyfluthrin was determined to be the cause of symptoms in all 27 farmworkers and four of six emergency responders. This finding is substantiated by the short distance between the site of pesticide application and the farmworkers; the detection of cyfluthrin on citrus foliage samples southeast of the spray position, suggesting that the pesticide drifted in the direction of the farmworkers; the sudden onset of symptoms coinciding with the application; and symptoms among both farmworkers and response workers that were consistent with those caused by pyrethroid pesticides. Wind direction and speed, measured at a weather station approximately 7 miles from the pesticide application site, is highly variable in the area where the incident occurred and likely contributed to the incident. Cyfluthrin is a type II pyrethroid that increased in use 1,100% in California from 1990 (4,099 lbs. applied) to 2003 (47,610 lbs. applied) (3). Pyrethroid pesticides are synthetic derivatives of natural pyrethrin insecticides. Both pyrethrins and pyrethroids act on insects by prolonging the inactivation of sodium channels in their nervous systems. Because mammals rapidly detoxify these compounds, humans are less susceptible to systemic effects by this mode of action. However, most human health effects caused by pyrethroids are the result of effects on sodium channels on nerves, in skin, and other organs. At high doses, signs of poisoning attributable to type II pyrethroids include profuse salivation and pulmonary edema, clonic seizures, opisthotonos (i.e., the spine is bent forward such that a supine body rests on its head and heels), coma, and death (4,5). At lower doses, commonly observed effects include paresthesia, erythema, dizziness, headache, fatigue, irritability to sound and touch, and skin, eye, upper respiratory tract, and gastrointestinal irritation (5,6). Symptoms typically improve within 24--48 hours in the absence of continued exposure. The inactive ingredients, which include solvents, also might have accounted for some of the reported symptoms. Illness caused by pyrethroid pesticides is diagnosed on the basis of exposure history and symptoms; erythema of exposed skin also might be evident. Urine metabolites are an indicator of exposure but are impractical for clinical evaluation because they are not measured by most clinical laboratories and because analysis requires knowledge of the exact parent compound (7). Moreover, urine metabolites do not correlate with exposure dose or symptoms. Treatment consists of decontamination and symptomatic therapy. Topical vitamin E cream can alleviate dermal paresthesia. During 1998--2003 in California, 12% (297 of 2,470) of occupational pesticide illness reports were attributed to pesticide drift (3). Because weather patterns are unpredictable, pesticide drift can occur even when applications are begun during calm periods. In this incident, pesticide drifted onto workers in a grape vineyard who had not been notified of a pesticide application in a neighboring citrus orchard. Inadequate communication between the applicators and farmworkers might have resulted in continued spraying despite the presence of workers in the grape vineyard. Employers are required to give notification of cyfluthrin application only to their own employees. Neither the applicators nor the citrus grower were required by law to provide notification to the farmworkers, who worked for a different employer. Even when not required, CDHS recommends that workers in adjacent areas should be notified about scheduled pesticide applications. Furthermore, pesticide applications should cease if workers are observed in neighboring areas. Pyrethroid pesticides are in widespread use for both agricultural and structural applications. Although considered to be a safer alternative to many other pesticides, pyrethroid pesticides such as cyfluthrin can cause pesticide illness even at low doses. Evaluating physicians should be knowledgeable regarding the potential for occupational illness caused by pesticide exposure, signs and symptoms, and methods of treatment. Nontoxic, sustainable methods of pest control should be encouraged for primary prevention of pesticide illness. References
Table 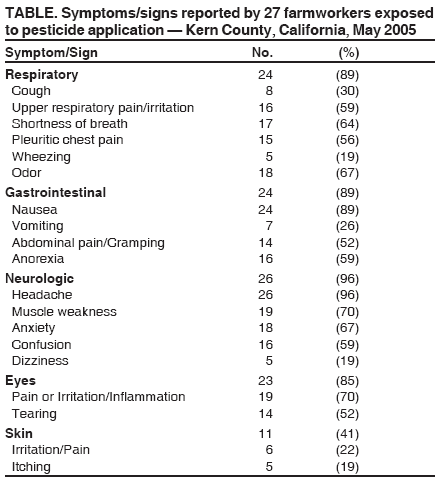 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Date last reviewed: 5/4/2006 |
|||||||||
|