 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Outbreak of Cutaneous Bacillus cereus Infections Among Cadets in a University Military Program --- Georgia, August 2004Although Bacillus cereus is known mainly as an agent of food poisoning, other infections caused by this organism have been documented in immunocompromised patients, including sepsis, meningitis, pneumonia, and wound infections (1,2). Certain populations are at increased risk for B. cereus infection, including cancer patients, neonates, intravenous drug users, and patients with a history of trauma, surgery, or catheterization (3--6). Primary cutaneous disease attributed to B. cereus in immunocompetent persons or in non--health-care settings rarely has been reported (7). This report is the first to document such an outbreak. On August 24, 2004, a local health department in Georgia received a call from a university health center describing 90 cadets with nonpruritic, impetigo-like lesions on their scalps; B. cereus was the common organism among the three patients whose lesions were cultured. The cases occurred during the freshman military orientation week that preceded the start of the fall term. The Georgia Division of Public Health (GDPH) conducted an investigation to determine the source of the infections, identify associated risk factors, and implement control measures. This report summarizes the results of the outbreak investigation, which identified receiving a short haircut at the start of orientation week, sharing sunscreen during the week, and membership in Company B as strongly associated with having scalp lesions. Recommendations to the university included changing the type of haircut required, increasing time allowed for showering, and issuing individual sunscreen. The results of this investigation underscore the need for military programs to incorporate good hygiene and infection-control measures into school orientation events. GDPH reviewed the events of orientation week, investigated cases of scalp dermatitis, collected environmental samples, and conducted a cohort study of participants in the military program during four site visits to the university. University personnel provided a schedule of orientation activities and a tour of each event location. Medical records from patients were reviewed and clinical findings discussed with university health-care staff. Patients were interviewed, and available clinical isolates were sent to the Georgia Public Health Laboratory for confirmation. Samples, including talc, Barbicide® disinfectant, and swabs of electric clippers, were collected from two barbershops providing haircuts to cadets. Soil and water samples were collected from event sites, and swabs were taken of shared helmets and sunscreen. Five patients donated their hats for the environmental and laboratory investigation. CDC analyzed the environmental samples and characterized bacterial isolates by biochemical analysis, 16S rRNA gene sequencing (8), and multilocus sequence typing (MLST) (9). After the initial investigation, GDPH conducted a cohort study of all cadets in the military program at the university. GDPH distributed questionnaires to all 660 cadets, including upperclassmen, 3 weeks after orientation week. The cadets were asked about demographic information, company and dormitory assignment, clinical symptoms, orientation event participation, exposure to soil and water, and hygiene practices, including laundry, bathing, and shared products. A case was defined as an occurrence of scalp lesions in a cadet treated with oral cephalexin from the school health center during August 10--30, 2004. Measures of association were estimated using multivariate logistic regression to control for confounding. The 4-year military program at the university had 660 students (292 freshman and 368 upperclassmen) organized into seven discrete companies. Cadets lived in five separate dormitories, two per room, organized by company, sex, and class year. Each floor shared a bathroom and a common living room. Orientation directly involved 292 freshmen; 115 upperclassmen supervised the events. Orientation started with a short haircut for all 255 freshman males at one of two civilian barbershops. Haircuts were performed by one of eight barbers in random order using electric clippers without a scalp guard. The third day of orientation week, the cadets completed an obstacle course involving immersion in mud and river water. On the final day, participants were required to rappel from rock walls and participate in survival training exercises. Helmets were worn and sunscreen was shared among cadets during these activities. Ninety-four (14%) of 660 cadets had scalp lesions, and one cadet was infected twice during the period from the start of orientation to when the questionnaire was administered. Thirty-three patients sought care at the student health center on the fourth day of orientation week, and 57 sought care on the fifth day. Five more cases, including the recurrent case, occurred 1 week after the start of school (Figure). All patients participated in orientation week; all were male and ranged in age from 16 to 24 years. The majority of patients were freshmen (84/94; 89%) and received a haircut on the first day of orientation (89/94; 95%). Approximately one third of the patients (33/94; 35%) were in Company B. The index patient noted onset of symptoms on the third day of orientation. Yellow sticky discharge followed by honey-colored crusts on the crown of his head were noted. Lesions were nonpruritic. Other patients had similar lesions with the same distribution. Infections resolved within 48 hours with the use of antibacterial soap and oral cephalexin (5-day prescription). Health-care providers obtained samples for culture from lesions of three cadets (Table). B. cereus was the only common organism isolated from all three patients and was identified by using biochemical tests and 16S rRNA gene sequencing. When analyzed by MLST, all three clinical B. cereus isolates were indistinguishable. B. cereus also was cultured from two separate barbershop clippers (two isolates), soil from the school grounds and orientation events (five isolates), and helmets (two isolates) worn during rappelling exercises. Five environmental isolates (three soil samples and two clippers) matched the clinical isolates by 16S rRNA. MLST was performed on these isolates, resulting in four unique sequence types (three from the soil samples and one from the two clippers), with no matches to the clinical B. cereus sequence type. The response rate for the cohort study was 73% (483/660); the response rate for freshmen was 84% (248/292). Of the respondents, 423 (88%) were male, and 248 (51%) were freshmen, which was representative of the entire cohort. The median age was 19 years, and 405 (84%) cadets were white. After adjusting for sex, freshman class status, and participation in orientation week, the multivariate logistic regression model indicated a statistically significant association between having scalp lesions and receiving a haircut (adjusted odds ratio [AOR] = 10.6; 95% confidence internal [CI] = 2.3--49.3, p<0.01), membership in Company B (AOR = 9.7; CI = 3.4--27.8, p<0.01), and sharing sunscreen (AOR = 2.7; CI = 1.3--5.4, p<0.01). Other risk factors examined included demographic information, exposure to soil and water, and hygiene practices (e.g., laundry, bathing, and use of shared products). Reported by: K Arnold, MD, C Drenzek, DVM, M Salter, MPH, Georgia Div of Public Health. MJ Arduino, DrPH, J Noble-Wang, PhD, Div of Healthcare Quality Promotion; A Hoffmaster, PhD, JE Gee, PhD, P Wilkins, PhD, J Jordan, R Morey, M Daneshvar, PhD, Div of Bacterial and Mycotic Diseases, National Center for Infectious Diseases; C Shuler, DVM, EIS Officer, CDC. Editorial Note:Bacillus cereus is a recognized bacterial pathogen in humans. Nongastrointestinal infections are usually the result of a breakdown in natural protective barriers such as the skin or immune system (1,2,5). The findings in this report indicate that immunocompetent persons can be vulnerable to cutaneous B. cereus infections when skin is compromised. Isolation of three indistinguishable B. cereus isolates from three patients on two separate days suggested that this was a common-source outbreak and not a laboratory contaminant, even though the environmental source of B. cereus was not identified during the investigation. All but five cases were diagnosed on two concurrent days, making person-to-person transmission unlikely. Transmission most likely occurred from an exposure at the beginning of the orientation week. The short haircut likely caused microabrasions, compromising the protective effect of scalp epidermis. Exposure to mud, sun, and sunscreen further provided an environment suitable for bacterial growth. The findings in this report are subject to at least three limitations. First, only three clinical samples were available for culture. Because of the number of cases and the positive response to therapy, the health-center staff treated cases empirically before GDPH involvement. Second, other risk factors and potential confounders might not have been identified during the site visits. Finally, cadets were asked about their orientation exposures nearly 3 weeks after the events occurred; recall bias might have influenced the findings. As a result of this investigation, GDPH made recommendations to the university military program for future orientations to minimize the risk for another outbreak. These included 1) changing the type of haircut required for male cadets that would allow for more hair and less injury to the scalp, 2) allowing adequate time for personal hygiene, and 3) distributing individual packets of sunscreen and discouraging sharing of sunscreen. These recommendations were implemented during the 2005 orientation activities; no skin infections were reported. University military programs should establish infection-control practices including good hygiene as part of their organized orientation events. Acknowledgments The findings in this report are based, in part, on contributions from P Blake, MD, M Tobin-D'Angelo, MD, Georgia Div of Public Health. References
Table 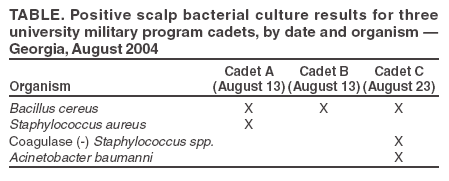 Return to top. Figure 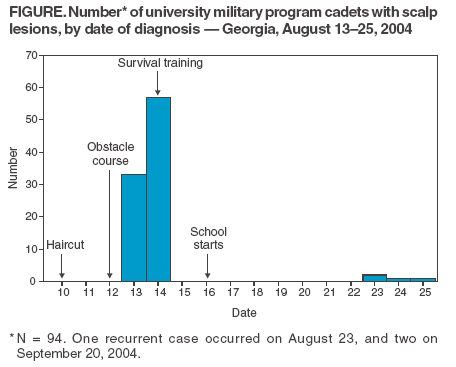 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Date last reviewed: 12/7/2005 |
|||||||||
|