 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Racial/Ethnic Disparities in Infant Mortality --- United States, 1995--2002A national health objective for the year 2000 was to reduce the infant mortality rate (IMR) in the United States to 7.0 deaths per 1,000 live births among infants aged <1 year (1,2). The national health objective for 2010 targets a rate of 4.5 infant deaths per 1,000 live births (3); an overarching goal calls for eliminating disparities among racial and ethnic populations. To examine racial and ethnic disparities in IMRs, data were analyzed from the National Vital Statistics System for the period 1995--2002. IMRs were calculated by race/ethnicity of the mother in each of the 50 states and the District of Columbia (DC). During 1995--2002, the overall IMR in the United States declined from 7.6 infant deaths per 1,000 live births in 1995 to 6.8 in 2001, and then increased to 7.0 in 2002 (Figure) (4--6). On the basis of data for 1995--2002 combined, the target of 4.5 infant deaths per 1,000 live births had been achieved by few racial/ethnic populations in few states. To reach the target in all racial/ethnic populations, strategies should identify and address those factors that contribute to high IMRs and disparities among populations. Data for this report were obtained from the linked birth/infant death data sets for 1995--2002 maintained by CDC's National Center for Health Statistics. These data sets link birth and death certificate information registered in all 50 states and DC for infants aged <1 year who died in the United States (4). Rates by race and Hispanic origin of the mother were calculated by using the linked data sets because race and ethnicity information about the mother from the birth certificate is more accurate than information about the infant from the death certificate (6). Annual data for 1995--2002 were combined to maximize the number of events and statistical reliability of rates for racial/ethnic populations in the 50 states and DC. During 1995--2002, IMRs declined for all racial/ethnic populations; however, the decrease for infants of American Indian/Alaska Native mothers was not statistically significant. In addition, little fluctuation was noted in the relative differences in IMRs between different racial/ethnic populations (Figure). A total of 225,534 infant deaths were reported in the United States during 1995--2002. By race/ethnicity of the mother, reported death totals were as follows: non-Hispanic white, 110,982; non-Hispanic black, 65,339; Hispanic, 35,447; Asian/Pacific Islander, 7,315; American Indian/Alaska Native, 2,915. Based on IMRs for 1995--2002 combined, for infants of non-Hispanic white mothers in DC, Massachusetts, New Hampshire, and New Jersey, the 2010 target of 4.5 infant deaths per 1,000 live births had already been achieved (Table). In addition, this target had been reached for infants of Asian/Pacific Islander mothers in eight states (Connecticut, Massachusetts, Missouri, New Jersey, New York, Oregon, Pennsylvania, and Texas). However, the target had not been achieved in any state for infants of non-Hispanic black, Hispanic, or American Indian/Alaska Native mothers. Reported by: TJ Mathews, MS, Div of Vital Statistics; KG Keppel, PhD, Office of Analysis and Epidemiology, National Center for Health Statistics, CDC. Editorial Note:Reducing the overall IMR in the United States is consistent with the first overarching goal of Healthy People 2010, which is to increase the years and quality of healthy life (3). Eliminating differences in IMRs is consistent with the second overarching goal, to eliminate health disparities (3). The findings in this report indicate that, from 1995 to 2001, the overall IMR declined 11% in the United States (from 7.6 to 6.8 infant deaths per 1,000 live births), before increasing to 7.0 in 2002*. A further decline of 36% overall is needed to reach the target IMR of 4.5 infant deaths per 1,000 live births in 2010, and even greater declines are required for certain racial/ethnic populations to reach the target. Whereas IMRs for most racial/ethnic populations declined from 1995 to 2002, little change was noted in the relative differences in IMRs among racial/ethnic populations. The findings in this report are subject to at least three limitations. First, the validity of differences in rates depends on the quality of the data. Linkage of birth and infant death records approaches 100% in most states (4), and reporting of the mother's race is virtually complete. However, variation exists among states regarding the reporting of Hispanic origin of the mother on birth certificates (7). Second, even with 8 years of data combined, reliable IMRs for all racial/ethnic populations in each state and DC could not be obtained because of small population sizes, especially among American Indians/Alaska Natives. Finally, racial and ethnic compositions of women of childbearing age at the state level might have changed from 1995 to 2002. Strategies to reduce IMRs and eliminate disparities among racial/ethnic populations should consider various factors that might differ by race/ethnicity. Such factors might include infant age at death, cause of death, mother's age and health, multiple births, low birthweight, premature births, assisted reproductive technology, prenatal visits, and access to health-care services. To help identify root causes of high IMRs and develop new strategies for reducing IMRs, in 2004, a State Infant Mortality Collaborative (8) was formed, which includes CDC, the Association of Maternal and Child Health Programs, and teams from five states (Delaware, Hawaii, Louisiana, Missouri, and North Carolina). References
* Data suggest that the increase in IMR in 2002 might be largely attributed to an increase in the number of infants, across most racial/ethnic populations, who were born at extremely low birthweights (i.e., <1 pound 10.5 ounces [750 grams]) and, therefore, had less chance for survival (5).
Table 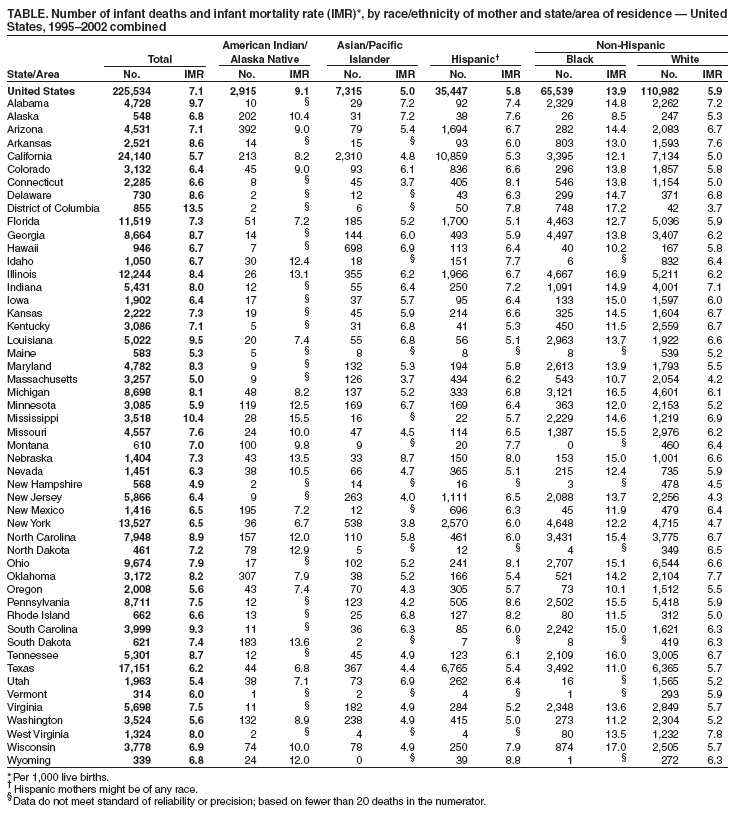 Return to top. Figure 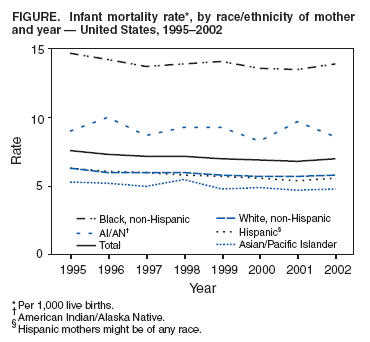 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Date last reviewed: 6/9/2005 |
|||||||||
|