 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Outbreaks of Pertussis Associated with Hospitals --- Kentucky, Pennsylvania, and Oregon, 2003Please note: An erratum has been published for this article. To view the erratum, please click here. Pertussis outbreaks have been reported in various settings, including sports facilities, summer camps, schools, and health-care facilities. Mild and atypical manifestations of pertussis among infected persons and the lack of quick and accurate diagnostic tests can make pertussis outbreaks difficult to recognize and therefore difficult to control. Outbreaks among health-care workers (HCWs) are of special concern because of the risk for transmission to vulnerable patients (1). This report describes three pertussis outbreaks among HCWs and patients that occurred in hospitals in Kentucky, Pennsylvania, and Oregon in 2003. These outbreaks illustrate the importance of complying with measures to reduce nosocomial infection when evaluating or caring for patients with acute respiratory distress or cough illness of unknown etiology. Case DefinitionsA clinical case of pertussis is defined as a cough illness lasting at least 2 weeks with one of the following: paroxysm of coughing, inspiratory "whoop," or posttussive vomiting, without other apparent cause (2). In addition, for the outbreaks described in this report, persons with cough lasting for >14 days were also considered to represent clinical cases of pertussis. A confirmed case was defined as 1) a cough illness of any duration with isolation of Bordetella pertussis, or 2) a case that met the clinical case definition and was either confirmed by a polymerase chain reaction (PCR) assay positive for B. pertussis DNA or had epidemiologic linkage to a confirmed case (2). In addition, sera from several patients with suspected pertussis were submitted to the Massachusetts State Laboratory Institute (MSLI) for serologic testing to support diagnoses.* Case InvestigationsKentucky. In early August 2003, an infant aged 2 months, who was born at 26 weeks' gestation and hospitalized in the intermediate care nursery (ICN) since birth, exhibited cough and apnea. Two days later, the infant was transferred to a neonatal intensive care unit (NICU) and ventilated mechanically. Seven days later, pertussis was suspected; 3 days later, nasopharyngeal (NP) secretions tested positive for B. pertussis DNA by PCR. The infant was treated with azithromycin (10 mg/kg/day on day 1 and 5 mg/kg/day on days 2--5), and droplet precautions were initiated in the NICU. A resident (physician A) in her first trimester of pregnancy examined the infant daily for 5 days in mid-August and did not wear a procedural or surgical mask. She experienced face-to-face exposure within 3 feet of the infant and was therefore designated as a close contact†. Nine days after initial exposure to the infant, physician A exhibited rhinorrhea and, 4 days later, a cough. Physician A declined recommended azithromycin prophylaxis. NP secretions obtained from the physician 4 days after symptom onset tested positive by PCR for B. pertussis DNA, and B. pertussis was isolated by culture. The source of pertussis in the infant might have been one of four ICN nurses who provided care to the infant and who had onset of a pertussis-compatible cough illness during the 3-week period preceding the infant's illness. NP secretions obtained from these nurses more than 4 weeks after cough onset were negative for B. pertussis DNA by PCR and negative for B. pertussis by culture; however, three of the nurses had levels of IgG antibody to pertussis toxin that met MSLI criteria for a positive result (i.e., >20 µg/ml) (3), indicating response to recent B. pertussis infection. Azithromycin prophylaxis was administered to 72 exposed patients and 72 HCWs who were identified as close contacts. No additional cases were identified. Pennsylvania. In early September 2003, an infant aged 3 weeks was admitted to the pediatric unit at hospital A for 1 day before being transferred to a referral hospital. The infant had cough, posttussive vomiting, and fever for 5 days. Pertussis infection was considered unlikely in the differential diagnosis, the patient was not tested for pertussis, and droplet precautions were not observed by staff. NP secretions were obtained for culture from the infant at the referral hospital, and B. pertussis was isolated 16 days later. Pediatrician B, who cared for the infant at hospital A, had onset of a cough illness 9 days after exposure. Even though he remained symptomatic, the pediatrician continued to treat patients without wearing a mask and was in contact with other HCWs, family members, and friends. Twenty-two days after his initial exposure, NP secretions obtained from pediatrician B were positive for B. pertussis DNA by PCR. Further investigation identified seven other pertussis cases in HCWs (a respiratory therapist, a radiograph technician, and five student nurses) who had been exposed to the infant at hospital A. In addition, nine of their HCW contacts had cough illnesses lasting >14 days. The first seven HCWs were tested too late (i.e., >3 weeks after symptom onset) and were negative; their nine contacts were tested within 2 weeks of symptom onset but were negative by culture and by PCR. In addition, two children who had been examined by pediatrician B tested positive for B. pertussis DNA by PCR. To prevent further transmission, hospital infection-control personnel screened exposed employees for cough illness and treated all symptomatic HCWs with a 5-day course of azithromycin (500 mg on day 1 and 250 mg on days 2--5), and these HCWs were excluded from work for 5 days. A total of 307 close contacts of the symptomatic HCWs, including other HCWs, household members, patients, residents of an institution for mentally impaired persons, and residents of a dormitory for student nurses, received prophylaxis with a 5-day course of azithromycin. In addition to notifying exposed patients by letter and by telephone, the hospital established an informational telephone hotline and conducted press conferences to inform patients and health-care providers of potential exposures. Oregon. In late September 2003, physician C treated an infant aged 12 months with PCR-confirmed pertussis in the pediatric ICU. Physician C, who wore a mask while providing care to the infant, had been exposed to a colleague who had prolonged cough illness since mid-September. The colleague was subsequently found to have elevated IgG anti--pertussis-toxin antibody levels (i.e., >20 µg/mL, as measured by the MSLI assay) (3) consistent with recent pertussis infection. Approximately 2 weeks after treating the infant, physician C had onset of a cough illness; 2 weeks later, the physician's NP secretions tested positive for B. pertussis DNA by PCR. Physician C was treated with a 5-day course of azithromycin (500 mg on day 1 and 250 mg on days 2--5) and was excluded from work for 5 days. The hospital infection-control program identified 129 close contacts of physician C, including 22 pediatric ICU patients, 78 employees, and 29 medical students and physicians. One exposed patient had severe cough illness and tested positive for B. pertussis DNA by PCR, and three employees had pertussis-like illness. The patient with confirmed pertussis and three symptomatic contacts were treated with a 5-day course of azithromycin; the remaining 125 contacts accepted prophylaxis. Because of increased awareness among staff and active case-finding by hospital infection-control personnel, three additional pertussis cases unrelated to the cases described previously were identified among employees, including a medical assistant from the perinatal clinic who might have exposed as many as 300 pregnant women, a surgical physician assistant who might have exposed 26 patients and 17 staff members, and a nurse midwife who might have exposed 17 patients and 21 staff members. An NP specimen from one of the employees tested positive by PCR, but the source of infection was unknown. The other two symptomatic employees reported exposure to their children who had recent PCR-confirmed pertussis. All three employees were treated, and their contacts were offered prophylaxis with azithromycin. The hospital used e-mail with a link to an Internet-based questionnaire to survey approximately 14,000 employees, students, and volunteers for recent onset of cough illness; 209 employees with cough illness responded, and 189 employees were interviewed. Azithromycin was recommended for 90 persons with cough illness of >7 days' duration. NP secretions were obtained from 64 survey respondents; all tests were negative for B. pertussis DNA by PCR. No additional linked cases among hospital employees were identified. Reported by: K Bryant, MD, Univ of Louisville; K Brothers, MD, Univ of Louisville School of Medicine; K Humbaugh, MD, Louisville Metro Health Dept, Kentucky. V Kistler, Allentown Health Bur; S Stites, S Madeja, Bethlehem Health Bur; JA Jahre, MD, SJ Schweon, B Coyle, MD, C Kalman, St. Luke's Hospital, Bethlehem; TL Burger, Lehigh Valley Hospital, Lehigh Valley; P Lurie, MD, Div of Infectious Disease Epidemiology; H Stafford, P Tran, MEd, Div of Immunizations; T Metcalf, J Naugle, W Miller, J Bart, DO, Bur of Community Health Systems, Pennsylvania Dept of Health. P Lewis, MD, R Taplitz, MD, M Post, MS, A Ashby, T Soden, T Clover, Oregon Health and Sciences Univ, Portland; K Segnitz, Multnomah County Health Dept; H Gillette, MPH, Oregon Health Svcs. T Tiwari, MD, FB Pascual, MPH, TV Murphy, MD, KM Bisgard, DVM, JS Moran, MD, Epidemiology and Surveillance Div, National Immunization Program; A Calugar, MD, EIS Officer, CDC. Editorial Note:Despite high childhood coverage for pertussis vaccination (4), reported pertussis incidence in the United States has increased from a low of 1,248 cases (0.54 per 100,000 population) in 1981 to an annual average of 9,431 cases during 1996--2003 (average annual rate: 3.3 per 100,000 population) (5). During 1996--2004, the majority of pertussis patients were either aged <6 months (35.1%) (i.e., too young to have received the 3-dose primary series) or aged >7 years (60.7%) (i.e., too old to receive a pertussis vaccination) (6). Adolescents and adults, including HCWs, might become susceptible to pertussis because of waning immunity. No pertussis vaccine is approved in the United States for persons aged >7 years; however, in 2004, two pharmaceutical companies submitted biologics license applications to the Food and Drug Administration (FDA) for two tetanus toxoid and reduced diphtheria toxoid and acellular pertussis vaccine adsorbed (Tdap) products, one for persons aged 10--18 years and the other for persons aged 11--64 years.§ This report highlights two primary difficulties in the diagnosis of pertussis. First, diagnosis might be delayed or missed because symptoms are atypical. In adolescents and adults, symptoms during the catarrhal stage are most often nonspecific, but the disease is already highly communicable (2). In infants, diagnosis might be delayed when the presentation is respiratory distress with apnea without the typical cough. Second, sensitive and specific diagnostic tests for pertussis are not readily available in many settings; culture, the standard test, has diminishing sensitivity with progression of the classic symptoms of the infection. PCR for pertussis is not standardized, and false-positive and false-negative results can occur (2). In addition, no serologic test for pertussis has yet been validated and made available nationally, although CDC and FDA are developing such a test (7). Because droplet transmission of pertussis can occur at the first contact with an ill patient, HCWs and hospital infection-control services should take measures to prevent hospital transmission (Box). Many nosocomial outbreaks might be prevented by HCWs' observing droplet precautions (i.e., wearing procedural or surgical masks and hand washing) (8). Delay in recognizing pertussis can result in spread of disease to HCWs, patients, and other contacts. HCWs should suspect pertussis in unvaccinated or partially vaccinated infants with respiratory distress (e.g., apnea or cough) and obtain NP secretions for culture. Isolation precautions are recommended for confirmed and suspected cases of pertussis (2). Erythromycin is recommended for treatment and prophylaxis of pertussis (1). However, because erythromycin frequently causes gastrointestinal disturbance, many patients do not complete the recommended 2-week course. Azithromycin was used during all the outbreaks described in this report because it causes fewer and milder side effects than erythromycin and its longer half-life means that fewer daily doses are required, thereby increasing the potential for patient compliance. A recent study that compared azithromycin administered as 10 mg/kg (maximum: 500 mg) on day 1 followed by 5 mg/kg (maximum: 250 mg) on days 2--5 with a 7-day treatment of erythromycin demonstrated equivalence between the two treatments (9). Nosocomial pertussis outbreaks can result in substantial public health and economic costs (10). Public health professionals and hospital decision-makers should consider potential savings and benefits from implementing effective infection-control strategies and from selective pertussis vaccination of HCWs when adult vaccines become available in the United States. References
* MSLI has validated and standardized an enzyme-linked immunosorbent assay (ELISA) for IgG antibodies to pertussis toxin that is used to confirm pertussis in Massachusetts (3). † For all outbreaks cited in this report, close contacts were defined as those persons who experienced face-to-face contact within 3 feet of a pertussis patient, including those who shared a room or living space with a pertussis patient or who were directly cared for by an HCW with pertussis. § Additional information is available at http://www.gsk.com/press_archive/press2004/press_07072004.pdf and http://www.us.aventispasteur.com/news/20040811_ADACEL.pdf.
Box 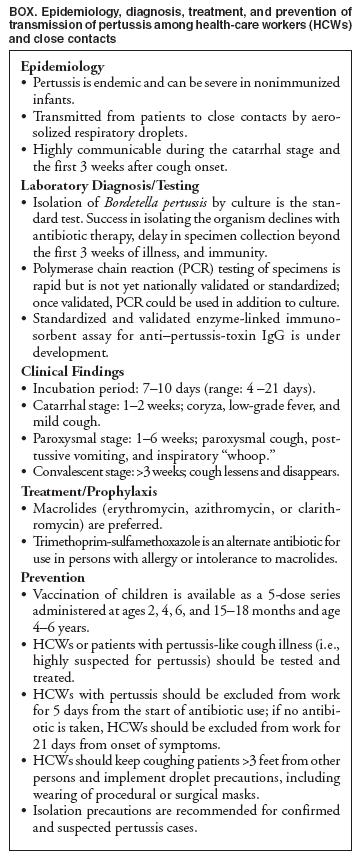 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 1/27/2005 |
|||||||||
This page last reviewed 1/27/2005
|