 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Serious Psychological Distress Among Persons with Diabetes --- New York City, 2003"Depression, anxiety, and other disorders causing serious psychological distress (SPD) frequently complicate the health care of persons with diabetes (1--3)." To assess the prevalence and effects of SPD among adults with diabetes, the New York City Department of Health and Mental Hygiene (DOHMH) analyzed data from approximately 10,000 adults who participated in the 2003 New York City Community Health Survey (CHS). The results indicated that 1) adults with diabetes were twice as likely to have SPD as those without diabetes, and 2) adults with both SPD and diabetes were more likely than those with only diabetes to live in poverty, report poor health, lack access to health care, and to have lost a spouse or partner to separation, divorce, or death. An integrated program of physical and mental health care that addresses socioeconomic barriers and improves access to treatment might improve the overall health of persons with diabetes and SPD. CHS is a random-digit--dialed telephone survey of noninstitutionalized New York City adults aged >18 years, conducted by DOHMH. The findings described in this report are from interviews in 2003 with 9,802 respondents (response rate: 59% of the 16,752 households contacted); a total of 9,590 persons provided complete data and were included as participants in the study. Interviews were conducted in 23 languages; the study was approved by an institutional review board. The survey was adapted from the Behavioral Risk Factor Surveillance System (BRFSS) survey and National Health Interview Survey. Diabetes was determined by using the modified BRFSS question, "Have you ever been told by a doctor that you have diabetes?" Respondents with positive responses that were not pregnancy related were classified as having diabetes. SPD was determined by using the K6 scale, a psychometrically validated, epidemiologic screening measure that is highly correlated with diagnostic measures of major depressive disorder, generalized anxiety disorder, schizophrenia, and other mental disorders (4). Respondents were asked how often during the preceding 30 days they felt "sad," "nervous," "restless," "hopeless," "worthless," or that "everything was an effort." Responses to these six feelings were measured on a scale of 0--4 (range: 0--24). Responses were summed and participants with scores >13 were classified as having SPD (5). Analyses were conducted by using statistical analysis software to account for the complex survey design. Prevalence estimates were adjusted to the 2000 U.S. standard census distribution, and 95% confidence intervals (CIs) were generated. Logistic regression was used to compute age-adjusted odds ratios (AORs) and to determine whether diabetes was an independent risk factor for SPD. Among all 9,590 participants, 498 had SPD, an age-adjusted prevalence of 5.0% (95% CI = 4.5--5.6). Among the 857 (9.0%) participants with diabetes, 80 had SPD, a prevalence of 10.4% (CI = 7.3--14.7). After controlling for age, sex, race/ethnicity, marital status, and household income, participants with diabetes were twice as likely as participants without diabetes to have SPD (AOR = 1.9; CI = 1.4--2.8). Adults with diabetes and SPD were more likely than adults with only diabetes to be divorced, separated, or widowed (48.7% versus 25.3%) or to have household incomes below $25,000 (70.2% versus 42.8%) (Table). Moreover, adults with diabetes and SPD reported poorer health-care utilization than adults with only diabetes. Only 11% of adults with diabetes and SPD had private insurance, compared with 41.6% of adults with only diabetes. Adults with both conditions also were more likely than adults with only diabetes to report not filling a prescription or seeing a doctor for a medical problem because of cost (42.0% versus 16.5% and 47.1% versus 23.1%, respectively). Adults with both conditions were also more than twice as likely as adults with only diabetes to use an emergency department as their usual source of health care (25.6% versus 9.8%) (Table). Self-reported health status was worse for adults with both diabetes and SPD, compared with adults with only diabetes. Fair or poor health was reported by 78.2% of adults with diabetes and SPD, compared with 39.8% of those with only diabetes. In addition, adults with both diabetes and SPD were three times as likely than those with only diabetes (64.2% versus 22.2%) to report >3 days during the preceding 30 days, when poor physical health limited their usual activities, and seven times as likely (63.3% versus 9.1%) to report similar limitations attributed to poor mental health (Table). Reported by: KH McVeigh, PhD, F Mostashari, MD, LE Thorpe, PhD, Div of Epidemiology, New York City Dept of Health and Mental Hygiene. National Center for Chronic Disease Prevention and Health Promotion, CDC. Editorial Note:Diabetes and other chronic diseases (e.g., hypertension and asthma) have been associated with higher rates of SPD (1--3,6,7). The findings in this report are consistent with previous studies of diabetes that have suggested SPD occurs twice as often among persons with diabetes as among the general population, usually in the form of depression or depressive symptomatology (1--3). The findings regarding the use of health-care services by persons with diabetes and depression compared with persons with only diabetes are consistent with other studies that have associated having diabetes and depression with poor physical and mental functioning, increased use of the emergency department, and poor adherence to medication regimens (8,9). Pharmacologic and nonpharmacologic mental health treatments have been shown to reduce depressive symptomatology in persons with both diabetes and depression; however, evidence conflicts regarding whether they improve glycemic control (10). The findings in this report are subject to at least three limitations. First, the sample represents only noninstitutionalized adults with telephones. Second, the cross-sectional nature of the study prevents determining whether SPD preceded or followed the onset of diabetes. Finally, the data are self-reported, and measures of glycemic control, self-care practices, severity of diabetes, and diagnostic measures to distinguish the exact type of SPD were not available. Persons with comorbid diabetes and SPD face formidable economic and social obstacles to receiving appropriate health care. Increased use of more effective methods for detecting and managing depression and other mental disorders might be particularly beneficial for persons with diabetes. Research is needed to assess the effects of these methods on diabetes and mental health outcomes. References
Table 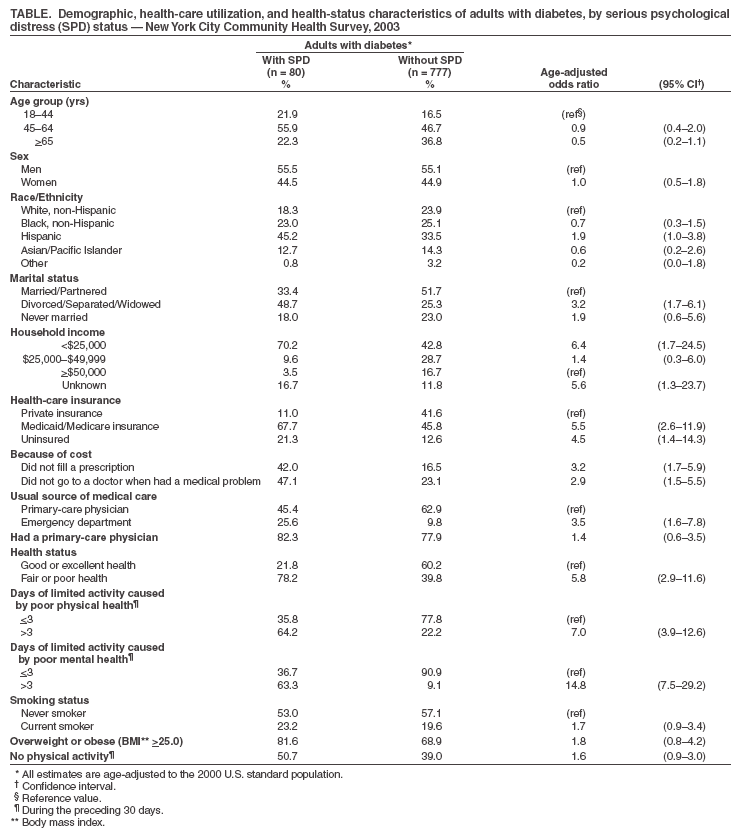 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 11/23/2004 |
|||||||||
This page last reviewed 11/23/2004
|