 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Breast- and Cervical-Cancer Screening Among Korean Women --- Santa Clara County, California, 1994 and 2002Asians account for an increasing proportion of the U.S. population (1). Koreans are the fifth largest Asian subpopulation, totaling 1.2 million in 2000 (1). In Santa Clara County (2000 population: 1.7 million), California, Koreans constitute 1.3% of the population (2). In 1994 and 2002, two population-based surveys were conducted among Korean women (2000 population: approximately 12,000) in Santa Clara County regarding breast- and cervical-cancer screening. The results were contrasted with two surveys of the general population of California women conducted during the same years. This report summarizes the findings of those surveys, which indicated that Korean women received less frequent breast- and cervical-cancer screening compared with all California women. This report also assesses compliance with the 2010 national health objectives for Papanicolaou (Pap) tests and mammography screening*. Multifaceted community programs that include culturally and linguistically sensitive education of community members and their health-care providers, along with improved health-care access, will be required to achieve the 2010 national health objectives. During August 1994--February 1995 and February--June 2002, the Center for Family and Community Health (CFCH) at the University of California, Berkeley, and Asian Health Services (AHS) conducted two household telephone surveys among Korean women in Santa Clara County. These results were compared with results for all California women from the 1994 and 2002 California Behavioral Risk Factor Survey (BRFS) and with the 2010 national health objectives for Pap tests and mammography screening. The surveys of Korean women were adapted from the 1993 California BRFS and modified for cultural sensitivity and appropriateness. Questionnaires were developed in English, translated into Korean, back-translated into English, and pretested. In 1994 and 2002, 94.2% and 93.0%, respectively, of the interviews were administered in Korean. Approximately 500 Korean surnames were identified, and Korean surname--based telephone lists were purchased from commercial sources. In 1994, a total of 5,079 listed telephone numbers with Korean surnames were sampled; 501 (9.8%) were eligible, 4,385 (86.3%) were ineligible, and 193 (3.8%) were of unknown eligibility. Most ineligible telephone numbers represented households without a Korean woman (71.5%) or were incorrect, disconnected, or nonworking (20.4%). The estimated survey response rate was 79.5%. In 2002, a total of 10,785 listed telephone numbers with Korean surnames were sampled; 626 (5.8%) were eligible, 9,180 (85.1%) were ineligible, and 979 (9.1%) were of unknown eligibility. Most ineligible telephone numbers represented households without a Korean woman (68.7%) or were incorrect, disconnected, or nonworking (24.6%). The estimated survey response rate was 66.5%. Interviewers spoke in Korean and switched to English if the respondent did not reply in Korean. The survey was described as a "study about health and immigration among Koreans." Respondents were eligible for the study if they self-identified as either Korean, Korean American, or of Korean origin. Both surveys consisted of two phases; in phase 1, one Korean woman aged >18 years was selected randomly within each eligible household and, in phase 2, to ensure an oversample of older women, additional Korean women aged >50 years were selected randomly from eligible households. In 1994, a total of 414 interviews were completed; in 2002, a total of 458 interviews were completed. Results were weighted to account for the probability of selection of the respondent and for the age distribution of Korean women in Santa Clara County in the 1990 Census for the 1994 survey and in the 2000 Census for the 2002 survey. Because of complex survey samples, SUDAAN was used to estimate sampling errors. For each pair of comparable estimates, t-tests were conducted, and estimates were examined to determine statistical significance (p<0.05). From 1994 to 2002, four statistically significant changes in sociodemographic characteristics were observed: 1) the percentage of women aged 18--29 years decreased from 29.3% to 18.1%, 2) the percentage with some college education increased from 61.7% to 71.7%, 3) the percentage who immigrated during the 5 years preceding the survey increased from 9.9% to 19.3%, and 4) the percentage who spoke little or no English increased from 61.0% to 77.2%. Thus, in 2002 compared with 1994, Korean women were more likely to be middle-aged, college educated, and recent immigrants who spoke little or no English. In 1994, 79.2% of Korean women in Santa Clara County reported having at least one routine checkup during their lifetimes, and 40.5% had routine checkups during the preceding year (Table). An estimated 65.0% had at least one Pap test during their lifetimes, and 56.6% had Pap tests during the preceding 3 years. Approximately 66.3% of Korean women had performed breast self-examinations at least once during their lifetimes, and 23.6% performed breast self-examinations monthly. Among Korean women aged >50 years, 40.9% had at least one clinical breast examination during their lifetimes, 29.2% had clinical breast examinations during the preceding 2 years, 43.3% had at least one mammogram during their lifetimes, and 28.7% reported having mammograms during the preceding 2 years. In 2002, six statistically significant improvements in screening practices among Korean women were observed: 1) 87.6% of women reported having at least one routine checkup during their lifetimes, 2) 55.4% reported routine checkups during the preceding year, 3) 55.4% of women aged >50 years reported having clinical breast examinations during their lifetimes, 4) 41.0% had clinical breast examinations during the preceding 2 years, 5) 77.9% had at least one mammogram during their lifetimes, and 6) 58.9% reported having mammograms during the preceding 2 years. In 1994 and again in 2002, Korean women in Santa Clara County were less likely to receive any preventive screening than all women in California (Table). The preventive screenings included routine checkups, Pap tests, breast self-examinations for all women, and clinical breast examinations and mammograms for women aged >50 years. Although certain preventive screenings increased over time for Korean women, screening rates were higher in the general population of California women. Korean women in Santa Clara County have yet to achieve the 2010 national health objectives for Pap tests and mammography screening; objectives for breast self-examinations or clinical breast examinations have not been established. In 2002, 74.8% of Korean women aged >18 years had received at least one Pap test during their lifetimes, and 63.0% received Pap tests during the preceding 3 years. Among Korean women aged >50 years, 58.9% had received mammograms during the preceding 2 years. Reported by: JM Moskowitz, PhD, G Kazinets, PhD, IB Tager, MD, Center for Family and Community Health, Univ of California, Berkeley; J Wong, MPH, Asian Health Svcs, Oakland, California. Editorial Note:The findings in this report indicate that among Korean women who resided in Santa Clara County in 1994 and 2002, breast- and cervical-cancer screening frequencies had not reached the 2010 national health objectives; however, certain improvements in screening practices were observed. From 1994 to 2002, mammography screening for women aged >50 years increased among Korean women. In addition, during this period, routine checkups increased for Korean women, and those aged >50 years were more likely to have received clinical breast examinations. In 1994 and 2002, Korean women were less likely to receive preventive screenings, compared with women in the California general population. Cultural and linguistic factors and health-care access and use might explain some of these differences. Previous research identified independent correlates of breast- and cervical-cancer screening among Korean women (4,5). Those who had regular medical checkups and private health insurance were more likely to have received a recent mammogram and clinical breast examination (4), and those who had regular medical checkups and public health insurance were more likely to receive a recent Pap test (5). Having a non-Korean doctor was associated with increased likelihood of having a recent Pap test, mammogram, and clinical breast examination, compared with women who had a Korean doctor (6). The findings in this report are subject to at least three limitations. First, the use of Korean surname--based telephone lists might exclude from the survey persons of Korean origin who resided in households without telephones, who did not list their telephone numbers, or who did not have Korean surnames. Second, because of the small sample sizes for Korean women, modest increases in screening were not statistically significant. Finally, self-reports of preventive screening might be subject to reporting biases. CFCH and AHS implemented a 4-year community intervention to improve breast- and cervical-cancer screening among Korean women in neighboring Alameda County (7). The intervention included educational workshops conducted in Korean churches and other community venues, a media campaign that used financial incentives to encourage screening, and a poster campaign. Culturally appropriate educational interventions, better health-care access, and health-care provider training might help improve breast- and cervical-cancer screening in Asian populations. Acknowledgments This report is based in part on contributions by the Korean Community Advisory Board; Y Ahn, H Choi, S Jun, S Kang, PhD, S Lee, K Min, Asian Health Svcs; A Lew, MPH, Los Angeles County Office of AIDS; B Wismer, MD, Tom Waddell Health Center; A Chen, MD, Alameda Alliance for Health, California. Health Promotion Disease Prevention Research Center Program, Div of Adult and Community Health, National Center for Chronic Disease Prevention and Health Promotion, CDC. References
* The objectives call for 97% of women aged >18 years to receive Pap tests (objective no. 3-11a), 90% to receive Pap tests during the preceding 3 years (objective no. 3-11b), and 70% of women aged >40 years to receive mammograms during the preceding 2 years (objective no. 3-13) (3). Table 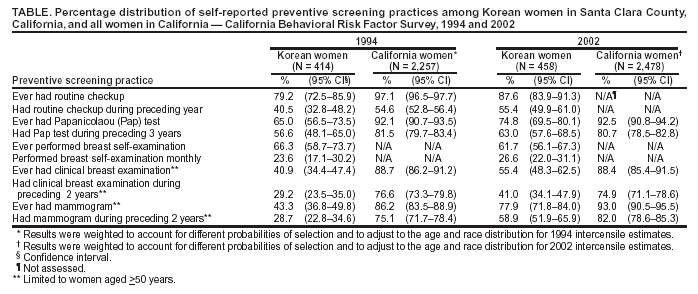 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 8/26/2004 |
|||||||||
This page last reviewed 8/26/2004
|