 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Tuberculosis Transmission in Multiple Correctional Facilities --- Kansas, 2002--2003Tuberculosis (TB) is a substantial health concern in correctional facilities; inmates and employees are at high risk, and TB outbreaks can lead to transmission in surrounding communities (1--3). The Advisory Council for the Elimination of Tuberculosis (ACET) recommends that all correctional facilities have a written TB infection--control plan (TBICP) (4). In September 2002, after diagnosis of smear-positive pulmonary TB in a prison inmate, the Kansas TB Control Program, with assistance from CDC, initiated a 6-month contact investigation. This report summarizes the results of that investigation, which determined that, while symptomatic for TB, the inmate had resided in three different jails and a state prison, placing hundreds of employees and other inmates at risk for TB infection. The circumstances of this case underscore the need for effective TBICPs to be implemented by trained employees in jails and prisons and for establishment of mechanisms to facilitate information-sharing between correctional facilities and local and state health departments. Case ReportIn October 2001, a U.S.-born man aged 36 years who was living temporarily in a California homeless shelter had a productive cough with hemoptysis. In December 2001, a physician at the shelter examined the man, suspected TB or neoplasia, and recommended a chest radiograph; however, the man did not follow the recommendation. In January 2002, the man returned to his residence in Kansas. Shortly after arrival, he turned himself in to police on an outstanding arrest warrant. He was held in jail A for 3 days before being transferred to jail B. While in jail B, he received a medical evaluation, and bronchial asthma was diagnosed. A tuberculin skin test (TST) was not administered, nor was a chest radiograph obtained. After 7 weeks in jail B, the man was released in March 2002. In June 2002, the man was convicted of a crime and again placed in jail A for 3 days. He was then transferred to jail C, a large overflow facility, pending sentencing. During the 6 weeks the man was in jail C, 125 transferred inmates passed through the facility. In August 2002, after being held for a total of 14 weeks in three jails, none of which had a TBICP or had provided TB screening for inmates or employees, the man was sentenced and transported to a Kansas state prison. During routine processing of entering inmates, he answered affirmatively to six of seven questions regarding TB symptoms. The state prison had a TBICP in place, and a medical evaluation was indicated on the basis of the man's answers; however, he was not referred for medical evaluation. Following the prison's TBICP procedure for entering prisoners who are to be serially TB screened, medical staff performed a two-step TST, which was read as 0 mm induration on both occasions. The new inmate was then placed among the general prison population. Medical staff at the state prison did not see the inmate again until 4 weeks later, when he was scheduled to receive chronic care for asthma. At this medical examination, he received a chest radiograph that showed a cavitary lesion of the right lower lobe. Despite having TB symptoms, he was placed back with the general prison population and scheduled for a computerized tomography (CT) scan 2 weeks later to rule out neoplasia. After the CT scan indicated cavitary lesions consistent with TB, the man, now the TB index patient, was placed in airborne infection isolation (AII), and sputum samples were collected. The AII room was newly constructed and in working condition, according to maintenance and monitoring documentation. However, because the recommended N95 respirators (5) were not available, prison health staff used surgical masks when in the AII room with the index patient. The first laboratory result from the index patient of 4+ smear-positive Mycobacterium tuberculosis was reported in late September, 6 weeks after he had arrived at the prison facility. Contact InvestigationA contact investigation conducted in Kansas and Missouri identified 318 of an estimated 800 possible contacts of the index patient during the infectious period, defined as the time from symptom onset to diagnosis, October 2001--September 2002. Of these contacts, two (0.6%) received a diagnosis of TB disease. These two patients had been cellmates of the index patient, one in jail A and the other in jail C. Tests of samples from these patients and the index patient determined they had M. tuberculosis isolates with a matching 10-band restriction fragment-length polymorphism pattern. The three isolates also had matching spacer oligonucleotide typing and mycobacterial interspersed repetitive unit patterns. Of 318 contacts identified, 256 were tested, and 47 (19.1%) of those received diagnoses of latent TB infection (LTBI); 60 contacts could not be located or refused follow-up. Two (4.1%) had a previously documented positive TST. Sixty (23.4%) contacts had a previously documented negative TST, and six (10.0%) of these had a positive TST during investigation screening. Among 196 contacts with no previously documented TST, 41 (20.9%) had a positive TST during the investigation screening (Table). The majority of infections among jail and prison employees occurred in jail B (TST reaction rate: eight of 36 [22.2%]) and jail C (TST reaction rate: five of 32 [15.6%]), compared with jail A (TST reaction rate: one of 14 [7.1%]) and the state prison (TST reaction rate: one of 58 [1.7%]). All three jails had an open-cell design with multiple inmates per cell; the state prison had single-occupancy cells with solid walls and doors. Reported by: P Griffin, D McClenahan, J VandeVelde, Kansas Tuberculosis Control Program; G Pezzino, MD, Kansas Dept of Health and Environment. R Funk, DVM, M Kitt, MD, EIS officers, CDC. Editorial Note:During 1992--2002, the TB rate in Kansas increased from 2.2 per 100,000 population to 3.3, the largest increase among all 50 states and the District of Columbia; in the majority of states, the TB rate declined (6). Although the contribution of correctional facilities to the TB burden in Kansas is unknown, a study in Tennessee reported that 43% of persons identified with TB in the city of Memphis had previous contact with a single urban jail and no other identified common exposure (3). As a result of the investigation findings described in this report, the Kansas TB Control Program worked with prisons, jails, and local health departments to provide guidance for developing or improving TBICPs and providing TB education and baseline TSTs for all correctional employees. This guidance has improved communication among all agencies to coordinate the return to the community of inmates receiving TB medications. Outbreak investigators were limited in their ability to determine the extent of TB transmission directly attributable to the index patient because of lack of previously documented TST results and the large number of contacts who could not be located or refused follow-up. Compared with the general population, inmates have higher TB prevalence, associated with their higher prevalence of human immunodeficiency virus, increased illicit substance use, and lower socioeconomic status [SES]. The risk for TB is known to increase with lower SES, with crowded living conditions having the greatest impact (7). Overcrowding enhances the likelihood of infectious droplet nuclei transmission and has been correlated with TST conversion in the Maryland state correctional system (8). Cell design and overcrowding might have been factors in TB transmission in these three Kansas jails. However, the impact of overcrowding and ventilation could not be assessed directly in this investigation because facility surveys were not conducted. Early identification and treatment of persons with TB disease remains the most effective means of preventing disease transmission. With the assistance of state and local health departments, correctional facilities should develop formal TBICPs (Box). Health departments should provide assistance to correctional facilities in developing TBICPs and conducting contact investigations, thereby controlling transmission within facilities and the surrounding communities. Employee education and continuous monitoring and evaluation of these policies should be part of every TBICP. In addition, correctional facilities should maintain a tracking system for inmate TB screening and treatment and establish a mechanism for sharing this information with local and state health departments and other correctional facilities (4). Acknowledgments The findings in this report are based in part on contributions from county health departments, prison health services, Kansas Dept of Corrections. Missouri Tuberculosis Control Program. References
Table 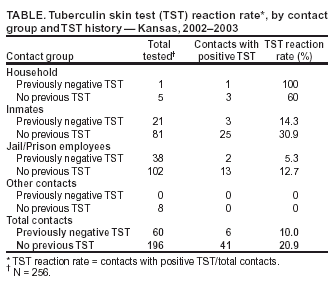 Return to top. Box  Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 8/19/2004 |
|||||||||
This page last reviewed 8/19/2004
|