 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Infant Health Among Puerto Ricans --- Puerto Rico and U.S. Mainland, 1989--2000Although the overall U.S. infant mortality rate (IMR) declined dramatically during the 1900s, striking racial/ethnic disparities in infant mortality remain (1,2). Infant health disparities associated with maternal place of birth also exist within some racial/ethnic populations (3,4). Eliminating disparities in infant health is crucial to achieving the 2010 national health objective of reducing the infant death rate to 4.5 per 1,000 live births (objective 16-1c) (5). Hispanics comprise the largest racial/ethnic minority population in the United States. Among U.S. Hispanics, considerable heterogeneity exists in infant health, with the poorest outcomes reported among Puerto Rican infants (6). This report compares trends during the previous decade in IMRs and major determinants of these rates such as low birthweight (LBW), preterm delivery (PTD), and selected maternal characteristics among infants born to Puerto Rican women on the U.S. mainland (50 states and the District of Columbia) with corresponding trends among infants born in Puerto Rico. The findings indicate that despite having lower prevalence of selected maternal risk factors, Puerto Rico--born infants are at greater risk for LBW, PTD, and infant death than mainland-born Puerto Rican infants. This report also highlights a persistent disparity in IMRs and an emerging disparity in LBW and PTD rates between Puerto Rico--born infants and mainland-born Puerto Rican infants. Future research should focus on identifying factors responsible for these disparities to improve infant health in Puerto Rico. Linked birth/infant death files for the 50 states, the District of Columbia, and Puerto Rico for 1989--1991 and 1998--2000 were used to assess IMR trends. Natality files for 1990--2000 were used to examine trends in rates of LBW (<2,500 g), PTD (<37 weeks' gestation), and selected maternal characteristics among live-born infants. Analyses were limited to infants born to Puerto Rican women (i.e., those born in Puerto Rico, those born on the mainland to Puerto Rico--born mothers, or those born on the mainland to mothers who reported being of Puerto Rican ethnicity). Infants born in Puerto Rico to women not born either in Puerto Rico or on the mainland were excluded. Four subpopulations of Puerto Rican infants were examined initially: infants born in Puerto Rico to Puerto Rico--born mothers, infants born in Puerto Rico to mainland-born mothers, infants born on the mainland to Puerto Rico--born mothers, and infants born on the mainland to mainland-born mothers of Puerto Rican ethnicity. However, because maternal place of birth was not associated substantially with infant health outcomes, data are shown for Puerto Rico--born and mainland-born infants without regard to maternal place of birth. Chi square tests were used to compare differences in the prevalence of infant and maternal characteristics and differences in IMRs among the groups. Low Birthweight and Preterm DeliveryIn 1990, Puerto Rico--born infants were 1.03 times more likely to be of LBW than mainland-born infants, and in 2000, this disparity increased to 1.2 (Figure). From 1990 to 2000, the LBW rate for Puerto Rico--born infants increased 18.0%, from 9.2% to 10.9%; for mainland-born infants, the LBW rate increased 3.7%, from 8.9% to 9.3%. Similar differences in LBW rate increases were observed when analyses were restricted to full-term and singleton births. The increase in the LBW rate among Puerto Rico--born infants was associated predominantly with an increase in the percentage of infants with an intermediate LBW (ILBW; 1,500--2,499 g); however, a small increase also was observed in the percentage with a very low birthweight (VLBW; <1,500 g) (Table 1). In 2000, Puerto Rico--born infants were less likely than mainland-born infants to be of VLBW (ratio = 0.7) but more likely to be of ILBW (ratio = 1.3) (Table 1). In 1990, Puerto Rico--born infants were less likely than mainland-born infants to be born preterm (ratio = 0.9) (Figure). From 1990 to 2000, the PTD rate among Puerto Rico--born infants increased 29.3% (from 11.6% to 15.0%), and that among mainland-born infants increased 0.9% (from 13.3% to 13.4%). As a result, in 2000, Puerto Rico--born infants were 1.1 times more likely than mainland-born infants to be born preterm. Similar differences in PTD rates were observed when analyses were limited to singleton births. The increase in the PTD rate among Puerto Rico--born infants was attributable primarily to an increase in the rate of moderately preterm births (32--36 weeks' gestation), although the rate of very preterm births (<32 weeks' gestation) also increased slightly (Table 1). In 2000, despite higher rates of LBW and PTD among Puerto Rico--born infants, their mothers were less likely than mothers of mainland-born infants to report selected maternal risk factors, including receiving late/no prenatal care, having <12 years of education, not being married, having plural births, and using tobacco (Table 1). The prevalence of first trimester prenatal care and the percentage of mothers aged <19 years at their infant's birth were similar for the two groups (Table 1). The prevalence of these maternal characteristics did not differ by maternal place of birth. Infant MortalityFrom 1989--1991 to 1998--2000, the combined IMR for Puerto Rico--born and mainland-born infants declined approximately 24%. The 1989--1991 IMR for Puerto Rico--born infants was 1.3 times greater than that for mainland-born infants (13.4 versus 10.4 per 1,000 live births) and remained 1.3 times higher during 1998--2000 (10.2 versus 7.9) (Table 2). However, the absolute difference in IMR between Puerto Rico--born and mainland-born infants declined from 3.1 per 1,000 live births during 1989--1991 to 2.3 during 1998--2000. IMRs across subpopulations defined by birthweight and gestational age were higher in both periods among Puerto Rico--born infants than among mainland-born infants. Except for postneonatal and VLBW mortality rates, IMRs among Puerto Rico--born infants declined more rapidly than among mainland-born infants in all infant age, birthweight, and gestational age subpopulations from 1989--1991 to 1998--2000 (Table 2). During 1998--2000, the greatest differences in IMRs between Puerto Rico--born infants and mainland--born infants were among those in the LBW and preterm subpopulations. Reported by: R Varela, MD, R Perez, MD, Puerto Rico Dept of Health. B Sappenfield, MD, A Duerr, MD, S Hillis, PhD, Div of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion; JA Martin, MPH, SJ Ventura, MA, National Center for Health Statistics; AM Grant, PhD, MK Whiteman, PhD, EIS officers, CDC. Editorial Note:Puerto Rico--born infants are at greater risk for LBW, PTD, and death than Puerto Rican infants born on the mainland. From 1989--1991 to 1998--2000, the overall infant mortality declined approximately 24% for Puerto Rican infants; however, the disparity in rates between infants born in Puerto Rico and those born on the mainland remained fairly constant. Disparities in LBW and PTD rates emerged during this period because of large increases among Puerto Rico--born infants. These disparities in infant health do not appear to be associated with the prevalence of late/no prenatal care, <12 years education, nonmarital births, plural births, or tobacco use. The higher risk for LBW, PTD, and death among infants born in Puerto Rico might reflect differences in the prevalence of other potential risk factors that are less accurately reported (e.g., alcohol consumption and maternal weight gain) or not reported at all in vital statistics (e.g., infection, stress, socioeconomic status, social support, nutrition, and quality of prenatal and perinatal care). The decline in IMR for Puerto Rican infants during the previous decade parallels declining rates for other racial/ethnic populations in the United States (7). Despite this decline, the 1998--2000 IMRs for Puerto Rico--born infants (10.2 per 1,000 live births) and for mainland-born infants (7.9) remain considerably higher than that for non-Hispanic U.S. mainland whites (5.8) (7). In addition, in 2000, the incidence of LBW and PTD among both Puerto Rico--born and mainland-born Puerto Rican infants was greater than that among infants in any other U.S. Hispanic origin group or U.S. racial/ethnic group, except non-Hispanic blacks. Therefore, a disparity in infant health exists not only between Puerto Rican infants born in Puerto Rico and Puerto Rican infants born on the mainland, but also between all Puerto Rican infants and infants from other U.S. racial/ethnic populations. The findings in this report are subject to at least two limitations. First, although underreporting of vital events is unlikely in Puerto Rico (6), risk factors such as maternal tobacco use might be reported less completely in Puerto Rico than on the mainland. Second, because Hispanic origin is not recorded on birth certificates in Puerto Rico, this study was based on records for infants born either in Puerto Rico or on the mainland; mainland-born infants were defined as having Puerto Rican ethnicity if their mothers were born in Puerto Rico or reported being Puerto Rican. This report highlights a continuing disparity in infant mortality rates and an emerging disparity in LBW and PTD rates between Puerto Rico--born infants and infants born on the mainland to Puerto Rican mothers. These differences should be considered in the planning and implementation of efforts to reduce IMRs among Puerto Ricans. The higher birthweight- and gestational age--specific IMRs in Puerto Rico contribute more to the overall higher IMR in Puerto Rico than do the differences in birthweight and gestational age distributions between Puerto Rico-- and mainland-born infants (8). Efforts to reduce IMR in Puerto Rico should focus on reducing mortality rates among LBW and preterm infants, perhaps by examining existing perinatal services. Additional opportunities might exist for lowering the overall IMR if the underlying causes of the increases in the prevalence of LBW and PTD can be identified and prevented. Improving infant health in Puerto Ricans will most likely require interventions at the individual, provider, and health-care system levels. References
Table 1  Return to top. Table 2 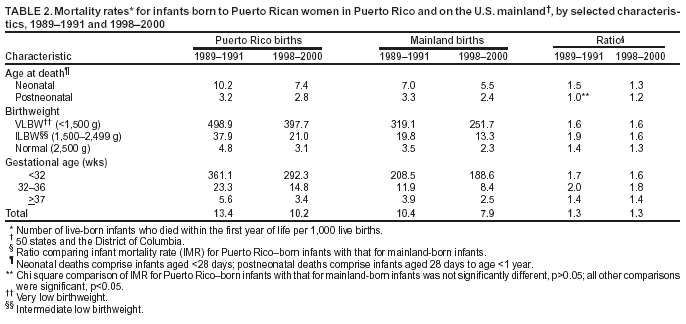 Return to top. Figure 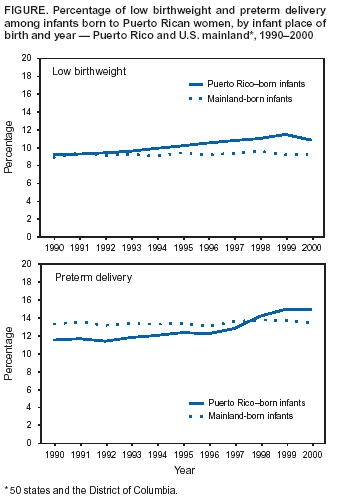 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 10/23/2003 |
|||||||||
This page last reviewed 10/23/2003
|