 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Recognition of Illness Associated With Exposure to Chemical Agents --- United States, 2003Since September 11, 2001, concern has increased about potential terrorist attacks involving the use of chemical agents. In addition, recent cases involving intentional or inadvertent contamination of food with chemicals have highlighted the need for health-care providers and public health officials to be alert for patients in their communities who have signs and symptoms consistent with chemical exposures (1--3). For example, in February 2003, a Michigan supermarket worker was charged with intentionally contaminating 200 lbs. of meat with a nicotine-containing insecticide (3). Although intentional release of chemical agents might be an overt event (i.e., one whose nature reveals itself), such as release of a nerve agent in a subway or a large explosion of a chemical container, a chemical release might instead be a covert event (i.e., an unrecognized release in which the presence of ill persons might be the first sign of an exposure), such as deliberate contamination of food, water, or a consumer product. To increase the likelihood that health-care providers will recognize a chemical-release--related illness and that public health authorities will implement the appropriate emergency response and public health actions, CDC identified examples of chemical-induced illness (Table) and created appropriate guidance for health-care providers and public health personnel. This report summarizes the epidemiologic clues and clinical signs or patterns of illness that might suggest covert release of a chemical agent. CDC is working to develop national surveillance capabilities for detecting chemical-release--related illnesses. A covert release of a chemical agent might not be identified easily for at least five reasons. First, symptoms of exposure to some chemical agents (e.g., ricin) might be similar to those of common diseases (e.g., gastroenteritis). Second, immediate symptoms of certain chemical exposures might be nonexistent or mild despite the risk for long-term effects (e.g., neurocognitive impairment from dimethyl mercury, teratogenicity from isotretinoin, or cancer from aflatoxin). Third, exposure to contaminated food, water, or consumer products might result in reports of illness to health-care providers over a long period and in various locations. Fourth, persons exposed to two or more agents might have symptoms not suggestive of any one chemical agent (i.e., a mixed clinical presentation). Finally, health-care providers might be less familiar with clinical presentations suggesting exposure to chemical agents than they are with illnesses that are treated frequently. Epidemiologic Clues Suggesting a Covert Chemical ReleaseEpidemiologic clues that might suggest the covert release of a chemical agent include 1) an unusual increase in the number of patients seeking care for potential chemical-release--related illness; 2) unexplained deaths among young or healthy persons; 3) emission of unexplained odors by patients; 4) clusters of illness in persons who have common characteristics, such as drinking water from the same source; 5) rapid onset of symptoms after an exposure to a potentially contaminated medium (e.g., paresthesias and vomiting within minutes of eating a meal); 6) unexplained death of plants, fish, or animals (domestic or wild); and 7) a syndrome (i.e., a constellation of clinical signs and symptoms in patients) suggesting a disease associated commonly with a known chemical exposure (e.g., neurologic signs or pinpoint pupils in eyes of patients with a gastroenteritis-like syndrome or acidosis in patients with altered mental status). Various chemical agents could be used as covert weapons, and the actual clinical syndrome will vary depending on the type of agent, the amount and concentration of the chemical, and the route of the exposure. However, certain clinical presentations might be more common with a covert chemical release. Certain syndromes are associated with groups of chemical agents with similar toxic properties that have been used previously, have high toxicity, or are easily available (Table) (4--10). Reported by: M Patel, MD, J Schier, MD, M Belson, MD, C Rubin, DVM, P Garbe, DVM, Div of Environmental Hazards and Health Effects; J Osterloh, MD, Div of Laboratory Sciences, National Center for Environmental Health, CDC. Editorial Note:Health-care providers, public health agencies, and poison control centers might be the first to recognize illness, treat patients, and implement the appropriate emergency response to a chemical release. Familiarity with general characteristics of a covert chemical release and recognition of epidemiologic clues and syndromic presentations of chemical agent exposures could improve recognition of these releases and might reduce further morbidity and mortality. Public health agencies and health-care providers might render the most appropriate, timely, and clinically relevant treatment possible by using treatment modalities based on syndromic categories (e.g., burns, respiratory depression, neurologic damage, and shock). Treating exposed persons by clinical syndrome rather than by specific agent probably is the most pragmatic approach to the treatment of illness caused by chemical exposures. State and local health departments should educate health-care providers to recognize unusual illnesses that might indicate release of a chemical agent. Strategies for responding to intentional chemical releases include 1) providing information or reminders to health-care providers and clinical laboratories; 2) encouraging reporting of acute poisonings to local poison control centers, which can guide patient management and facilitate notification of the proper health agencies, and to the local or state health department; 3) initiating surveillance for incidents that potentially involve the covert release of a chemical agent; 4) implementing the capacity to receive and investigate any report of such an event; 5) implementing appropriate protocols, including potentially accessing the Laboratory Response Network for Bioterrorism, to collect and transport specimens and to store them appropriately before laboratory analysis; 6) reporting immediately to CDC and local law enforcement if the results of an investigation suggest the intentional release of a chemical agent; and 7) requesting CDC assistance when necessary. To begin developing national surveillance capabilities for detecting chemical-release--related illnesses, CDC is collaborating with the American Association of Poison Control Centers to use its Toxic Exposure Surveillance System to identify index cases, evolving patterns, or emerging clusters of hazardous exposures. Identification of early markers for chemical releases (e.g., characteristic symptom complexes, temporal and regional increases in hospitalizations, or sudden increases in case frequency or severity) will enable public health authorities to respond quickly and appropriately to an intentional chemical release. CDC materials for emergency and health-care personnel, including a list of chemical agents and biologic toxins and their expected clinical syndromes, are available at http://www.bt.cdc.gov/agent/agentlistchem.asp. Additional information about responding to chemical attacks is available from the U.S. Army Medical Research and Materiel Command at http://www.biomedtraining.org/progmat.htm, the U.S. Army Medical Research Institute of Chemical Defense at http://ccc.apgea.army.mil, and CDC and the Agency for Toxic Substances and Disease Registry at http://www.atsdr.cdc.gov/mhmi.html. References
Table 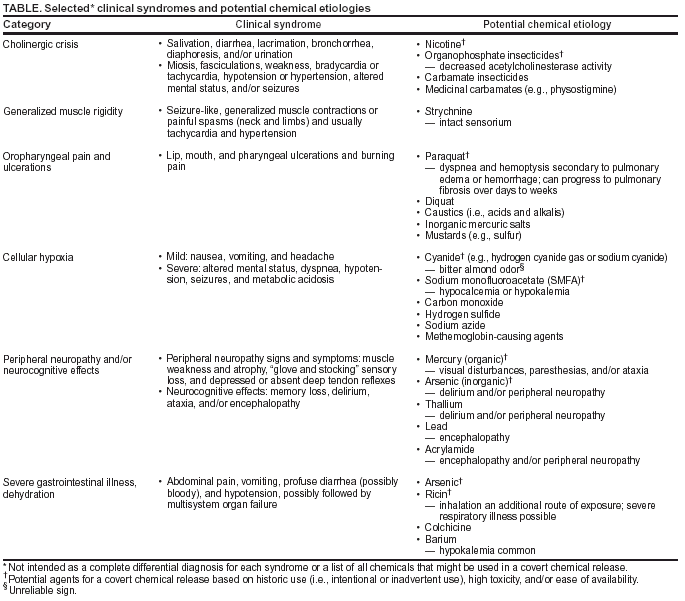 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 10/2/2003 |
|||||||||
This page last reviewed 10/2/2003
|