 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Knowledge, Attitudes, and Behaviors About West Nile Virus --- Connecticut, 2002Since West Nile virus (WNV) was first recognized in the United States in 1999, the geographic distribution has widened progressively, and the resulting human morbidity and mortality has increased (1). The cornerstones of WNV control and prevention are 1) surveillance with sustained and integrated mosquito control to detect the presence of WNV in areas where humans are at risk and 2) public education on the use of personal protective behaviors (PPBs) and peridomestic mosquito control to reduce the risk for mosquito bites (2). In Connecticut, strategies to improve public education and WNV-risk awareness consist of issuing graded warnings after assessing local surveillance findings during the transmission season. In 2002, three of the 17 Connecticut patients with confirmed WNV infection reported having used any PPBs. To assess knowledge, attitudes, and behaviors about WNV during the transmission season, the Connecticut Department of Public Health added questions about WNV to its Behavioral Risk Factor Surveillance System (BRFSS) survey conducted during August--November 2002. This report summarizes the results of that analysis, which indicate that general awareness of WNV and knowledge of elderly persons being at risk for more severe illness were high; however, awareness of local surveillance findings was poor, and belief in the local presence of WNV did not predict the use of PPBs. The findings underscore the need for continued public education about the risk for WNV infection and the use of PPBs and the need for regular systematic evaluations of knowledge, attitudes, and behaviors to refine and improve public health messages effectively. BRFSS is a state-based, random-digit--dialed telephone survey of the noninstitutionalized, civilian population aged >18 years. The set of WNV questions included a question about knowledge of age groups at higher risk for severe illness; a question about how worried a person was about getting WNV; two questions about awareness of local dead bird or mosquito surveillance findings; four questions about PPBs to protect against mosquito bites during July and August, the months of peak risk in Connecticut; and a question about how often a person spent >30 minutes outdoors in the evening during July and August. PPB questions included avoiding outdoor areas where mosquitoes are present, avoiding outdoor activities, wearing long-sleeved shirts and long pants, and using insect repellent on skin or clothes. Descriptive and analytic analyses were performed by using SAS version 8.2 and SUDAAN version 7.5. Data were adjusted to account for differing probabilities of selection and to match the state population of adults by age and sex. A total of 1,791 interviews were completed; response rate was 61%. The median age of respondents was 47 years (range: 18--97 years); 21% were aged 50--65 years, 20% were aged >65 years, 52% were female, 82% were white, and 98% were English-speaking. Overall, 1,617 (96%) respondents believed that elderly persons were more likely than others to have severe illness from WNV infection, and 1,249 (63%) believed the same to be true for infants. A total of 906 (56%) respondents were at least "a little" worried about getting WNV infection (10% "very" and 46% "a little"). A total of 19% of persons living in towns with positive WNV surveillance findings in 2002 were aware that WNV had been detected in their area. To protect themselves from mosquitoes, 60% of respondents reported that they sometimes or always avoided outdoor areas with mosquitoes, 39% avoided outdoor activities, 51% wore long-sleeved shirts and long pants, and 57% used insect repellent on skin or clothes (Table 1). The majority (77%) of respondents sometimes or always used at least one PPB, and 45% always used at least one PPB; 59% sometimes or always used at least two PPBs, and 15% never used any PPBs. Of the 291 persons aged >65 years who believed they were more likely to have severe illness, 61% always used at least one PPB, 68% sometimes or always used at least two, and 17% never used any. Multivariable logistic regression analyses were used to examine four outcome variables, including sometimes or always using insect repellent, always using at least one PPB, sometimes or always using at least two PPBs, and never using any of the four PPBs (Table 2). Using insect repellent was significantly associated with being aged <50 years, being a little or very worried about getting WNV, and more often spending >30 minutes outdoors in the evenings. Always using at least one PPB was significantly associated with being female, being aged >65 years, having a lower annual income ($25,000--$75,000), and being a little or very worried about getting WNV. Sometimes or always using two or more PPBs also was significantly associated with being female and being a little or very worried about getting WNV. Never using PPBs was significantly associated with being male and not being worried about getting WNV. Reported by: ML Adams, L LoBianco, L Wilcox, JL Hadler, MD, Connecticut Dept of Public Health. KS Griffith, MD, EIS Officer, CDC. Editorial Note:The findings in this report document high awareness of WNV and knowledge of elderly persons being at risk for severe illness. Persons aged >50 years were more likely than persons aged 18--49 years to always use at least one PPB. In addition, nearly half of all respondents reported always using some form of personal protection, and reported use of PPBs was much higher among respondents than among persons with confirmed WNV infection. However, awareness of local WNV surveillance findings was poor, and, in contrast to concern about getting WNV infection, belief in the local presence of WNV was not a predictor of use of PPBs. Although public announcements of local surveillance findings should continue, additional methods of communicating the changing levels of risk and appropriate levels of concern should be explored. The findings in this report are subject to at least four limitations. First, BRFSS relies on the use of self-reporting, which does not allow for validation of responses. Second, extensive public health outreach and education on the use of PPBs has occurred in Connecticut during the preceding 15 years, primarily because of the emergence and recognition of Lyme disease. Therefore, Connecticut residents might have a higher reported baseline use of and/or might be more responsive to public health messages concerning PPBs. Third, questions about the use of PPBs were asked specifically about behaviors during July and August; therefore, behaviors during September and October and how behaviors might have changed during the transmission season were not evaluated. Finally, because BRFSS is a telephone survey, data were not collected from persons who use cellular phones exclusively or who do not have a telephone. The use of PPBs is the most effective means of controlling exposure to WNV infection and might depend on several factors, including an understanding of the disease and how exposure occurs, personal perception of risk, and acceptability of using available measures. The WNV epidemics of 2002 and 2003 underscore the need for continued public education, especially regarding personal protection. Additional efforts should be made to evaluate knowledge, attitudes, and behavior and to use this information to refine and improve public health messages and the effectiveness with which they are delivered. In Connecticut in 2003, questions about WNV were again added to BRFSS to monitor the use of PPBs and the effectiveness of health-education efforts. References
Table 1 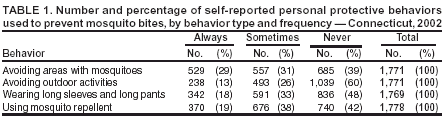 Return to top. Table 2 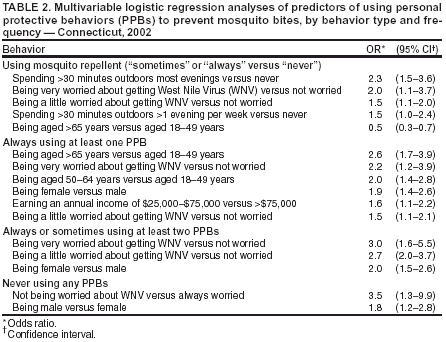 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 9/18/2003 |
|||||||||
This page last reviewed 9/18/2003
|