 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Syndromic Surveillance for Bioterrorism Following the Attacks on the World Trade Center --- New York City, 2001Immediately after the September 11, 2001, terrorist attacks on the World Trade Center (WTC), the New York City Department of Health and Mental Hygiene (NYCDOHMH) was concerned about the possibility of a secondary attack with a biologic agent. Because NYCDOHMH lost communications as a result of the attacks, concern arose that this disruption would affect the ability to recognize a bioterrorist event. To address this concern, NYCDOHMH quickly implemented a syndromic surveillance system in hospital emergency departments (EDs) to identify a large-scale bioterrorist event and other health conditions related to the WTC attacks. This report describes the operational and maintenance aspects of conducting syndromic surveillance for bioterrorism (BT) and demonstrates the limitations of drop-in systems that rely on manual data collection. Health departments that are establishing early warning systems for BT should consider seeking routinely collected electronic data. On the evening of September 11, NYCDOHMH, in collaboration with epidemiologists from CDC, began planning for the immediate implementation of an ED-based syndromic surveillance system. The system design was based on drop-in surveillance systems deployed by CDC at the World Trade Organization Ministerial (Seattle, Washington) in 1999, the Superbowl (Tampa, Florida) in 2001, and other venues. A total of 15 New York City (NYC) emergency departments (EDs) were selected as sentinel sites on the basis of their patient volumes and locations; all agreed to participate. A one-page form was created for coding each ED visit into one of 12 syndromes; seven symptoms represented clinical presentations that might result from exposure to a bioterrorist agent, four represented possible sequelae of the WTC attacks (non-BT), and a "none of the above" category represented patients who did not have either (Table). On the basis of their clinical judgment, health-care providers were asked to choose the syndrome that best represented the patient's primary diagnosis. The form also recorded the patient's name, hospital, medical record number, sex, date, age, home postal code, work postal code, and whether the patient was in the vicinity of the WTC on September 11. By the use of a modification of the CUSUM method (1), citywide and hospital aberrations were calculated, and a modification of SaTScan (2) was used to detect spatial patterns by hospital and home postal code. To account for fluctuations in ED volume, daily counts of each syndrome of interest were divided by the "none of the above" category. This Syndrome to None Ratio (SNR) was then used in the CUSUM and SaTScan analyses. Both techniques compared the daily ratio to its cumulative baseline by hospital, hospital cluster, or postal-code cluster. Alarms were generated when the SNR was significantly higher for the day in question compared with the recent past. The patient's name was not entered into the database but was obtained from medical records to investigate alarms. On the evening of September 13, medical epidemiologists visited each ED to orient and train hospital staff. Field teams composed of up to three CDC Epidemic Intelligence Service Officers (EISOs) per hospital were dispatched on September 14 and provided 24-hour coverage at 15 hospitals for the initial 2 weeks and 18-hour coverage at 12 hospitals for the remainder of the 30-day surveillance period. Each team performed data entry onsite, ensured form completion when necessary, and conducted follow-up of patients to investigate alarms. Data were sent to NYCDOHMH's temporary headquarters by 9:00 a.m. each morning. Data collection and analysis were begun on September 13. Completeness of reporting was monitored by dividing the number of daily records by the daily ED census obtained from each hospital's logbook. During September 13--October 12, a total of 68,546 ED visits were recorded. A low completion of forms occurred on September 13 before the deployment of EISOs and again on September 28, when the change in surveillance occurred. Patient visits were recorded from every NYC home postal code. Coverage, as determined by the ratio of visits by patients from the same postal code to the population of that area, was highest in Manhattan and the Bronx and lowest in Queens. Completeness of reporting ranged from 72% to 97% (mean: 90%) during the first 2 weeks, when hospital surveillance staffing was 24 hours per day, and from 65% to 90% (mean: 82%) during the second 2 weeks, when 18-hour ED surveillance coverage was employed. A total of 48,769 (71.1%) visits were coded as "none of the above," followed by 13,890 (20.3%) in the non-BT syndrome group, 4,421 (6.4%) in the potential BT syndrome group, and 1,467 (2.1%) with no code checked. Over the 30-day surveillance period, the mean SNR for trauma was the highest of any syndrome (18.6%), followed by exacerbation of a chronic respiratory condition (7.6%). Diarrhea/gastroenteritis and upper- and lower-respiratory infections with fever were the most common syndromes possibly associated with BT, with mean SNRs of 4.4% and 4.2%, respectively. Respiratory infection and rash were reported most often in children, with 1,323 (67%) respiratory syndrome visits and 63 (59%) rash syndrome visits occurring among children aged <15 years. Persons aged 25--64 years accounted for 298 (80%) inhalational visits and 673 (75%) anxiety visits. Binary logistic odds ratios (ORs) and 99.9% confidence intervals (CIs) were calculated to compare SNRs with patients reporting proximity to the WTC on the day of the attacks (i.e., if the patient was south of Canal Street). The analyses were repeated for home postal codes within a 2-mile radius of the WTC. Persons who were near the WTC on September 11 or resided in the area, as defined by a 2-mile radius around the site, were no more likely to have a syndrome of BT interest than those without such proximity. Persons reporting proximity to the WTC on September 11 were 61.5 (99.9% CI=44.7--84.7) times more likely to visit an ED for smoke/dust inhalation than the "none of the above" category compared with patients not reporting such proximity. ORs for anxiety, trauma, and asthma were 8.3 (99.9% CI=6.2--11.0), 1.9 (99.9% CI=1.6--2.2), and 1.8 (99.9% CI=1.4--2.3), respectively. The only significant OR for home postal code within 2 miles of the WTC was for smoke/dust inhalation, with ED visits from these postal codes having a 2.4 (99.9% CI=1.7--3.4) greater likelihood of this syndrome compared with the "none of the above" category. Two types of alarms were investigated: 1) individual hospital-level alarms as determined by CUSUM and 2) geographically localized alarms by postal code and hospital as determined by SaTScan. A total of 91 alarms were registered for the five syndromes of BT interest (respiratory, rash, gastrointestinal, neurologic, and sepsis), 53 by CUSUM, and 38 by SaTScan. At least one alarm occurred on 24 of the 27 surveillance analysis days. Gastrointestinal (n=26) and respiratory (n=25) alarms were the most frequent syndromes triggering an investigation. Approximately 7% of alarms were attributed to errors in coding and data entry. Single cases of botulism-like illness and unexplained death with fever were detected and investigated. Evaluations of alarms did not reveal any similarity in the cases or final diagnoses suggestive of a natural outbreak or bioterrorist attack. Reported by: J Ackelsberg, MD, S Balter, MD, K Bornschelgel, MPH, E Carubis, B Cherry, VMD, D Das, MPH, A Fine, MD, A Karpati, MD, M Layton, MD, F Mostashari, MD, B Nivin, MPH, V Reddy, MPH, D Weiss, MD, New York City Dept of Health and Mental Hygiene. L Hutwagner, MS, GM Seeman, Div of Public Health Surveillance and Informatics, Epidemiology Program Office; J McQuiston, DVM, Div of Viral and Rickettsial Diseases; T Treadwell, DVM, Bioterrorism Preparedness and Response Program, National Center for Infectious Diseases; J Rhodes, PhD, EIS Officer, CDC. Editorial Note:This report highlights the need for more experience with and evaluation of syndromic surveillance. Immediately after the attacks on the WTC, public health officials in NYC went on heightened alert for a bioterrorist attack. A drop-in surveillance system at sentinel EDs was established quickly and sustained during the immediate aftermath and was useful in assuring both public health and government officials that no large-scale aerosolized biologic agents had been released in NYC. The syndromes of BT concern comprised a minority (6.4%) of ED visits observed. Using SNR as the measure for comparison was necessary to account for differences in ED volume based on day of week and the reduction in participating hospitals that occurred after the first 2 weeks. The 68,547 visits recorded during the 30-day surveillance were an adequate sampling, comprising 23% of the average monthly citywide ED visits (Greater New York Hospital Association unpublished data, 2001). Visits were concentrated in Manhattan, particularly in the immediate vicinity of the WTC. Proximity to the WTC was strongly associated with ED visits for smoke/dust inhalation, presumably because of the tremendous amount of particulate matter released by the explosion and collapse of the WTC buildings. No syndrome of BT interest was associated with either measure of proximity. Several challenges and limitations in conducting syndromic surveillance were revealed in this effort. First, the system required significant technical and staff resources, especially for the ED-based staff, which would have severely disrupted NYCDOHMH core public health activities were it not for the deployment of approximately 45 EISOs from CDC. Field staff required cell phones with two-way radios, daily transportation to and from hospitals, and data-processing support from NYCDOHMH-based staff. The number of staff needed to operate the system was not sustainable beyond the 30-day period. Second, rapid implementation required personnel to resort to manual data entry, resulting in coding errors. Both these errors and insufficient baseline data contributed to false alarms. Third, the parameters of this system assumed that patients with prodromal symptoms of an illness caused by a bioterrorist agent would seek care in EDs. Although the system was in place, it did not detect the outbreak of anthrax among recipients of anthrax-contaminated letters in NYC in mid-September (3). Six of the seven patients diagnosed with cutaneous anthrax in NYC did not seek care in EDs; however, syndromic surveillance in NYC was not designed to detect single cases or cutaneous cases but rather an outbreak due to an aerosolized release of a biologic agent, in which early recognition could prevent mortality. Fourth, a total of 15 EDs were chosen as sentinel sites to be geographically representative of the NYC population. However, some areas of the city were not well represented, and the system could not account for potentially exposed persons residing outside of the five NYC boroughs. Finally, because investigations of alarms revealed substantial heterogeneity of symptoms and diagnoses within syndromes, deciding when to pursue investigations with chart review was especially difficult. Although trained hospital staff reviewed medical records and received clinical status updates, only time-consuming laboratory tests provided assurance that no agent of BT concern was implicated. Therefore, it difficult to determine whether such ED-based systems can detect a large-scale bioterrorist attack before clinicians report suspected or confirmed cases. Although costly and resource intensive, this EISO-based system was warranted given the unprecedented nature of the WTC attacks, the concerns about a secondary attack with a biologic agent, and the need to rapidly establish a surveillance system to monitor unusual disease occurrences or clusters due to the breakdown of NYCDOHMH's routine communication systems. The system has been replaced by an expanded and automated syndromic surveillance system using electronic ED chief complaint logs. As more state and local health departments are implementing syndromic surveillance systems, public health officials should consider adopting a regional approach with standardized coding algorithms; expansion of data sources to include laboratory, radiology, and outpatient information; and discussions about collaborative methods for rapidly investigating statistically generated aberrations. Acknowledgments The findings in this report are based on data and services contributed by emergency department and infection control staff at the 15 sentinel New York City hospitals, the emergency response teams of the New York City Department of Health and Mental Hygiene, and EIS officers from CDC. References
Table 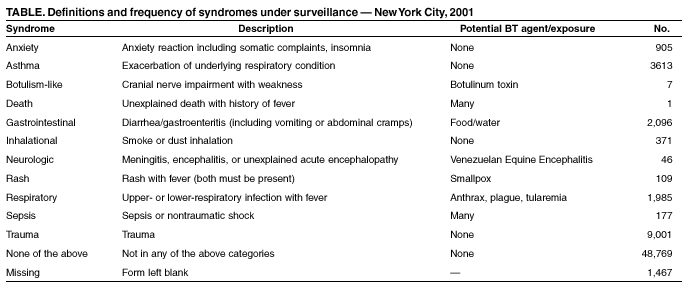 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 9/9/2002 |
|||||||||
This page last reviewed 9/9/2002
|