 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Invasive Cervical Cancer Among Hispanic and Non-Hispanic Women --- United States, 1992--1999During 1973--1999, both the incidence of and death rates for cervical cancer decreased approximately 50% in the United States (1). For 2002, approximately 13,000 new cases of invasive cervical cancer are expected, and approximately 4,100 women will die of the disease (2). Although invasive cervical cancer can be prevented by regular screening (3), the prevalence of Papanicolaou (Pap) testing remains relatively low among minority populations such as Hispanic women (4). To characterize the incidence of invasive cervical cancer, CDC analyzed incidence data for Hispanic and non-Hispanic women during 1992--1999 in 11 geographic areas with population-based registries (5). This report summarizes the results of this analysis, which indicate that the incidence of invasive cervical cancer decreased for Hispanic and non-Hispanic women. However, among women aged >30 years, cervical cancer incidence for Hispanic women was approximately twice that for non- Hispanic women. To lower the incidence of invasive cervical cancer, local health organizations should provide culturally appropriate public health interventions that encourage participation in readily accessible cervical cancer-- screening programs. Data were obtained from the Surveillance, Epidemiology, and End Results (SEER) Program of the National Cancer Institute (5). Microscopically confirmed invasive cervical cancer cases (International Classification of Diseases for Oncology, Second Edition, codes C532--C539) were selected. SEER*Stat version 4.2 (5) was used to compute incidences per 100,000 women and age-adjusted to the 2000 U.S. standard population by 5-year age groups. To test for significant trends, linear regression was used to determine the estimated annual percent change (EAPC) and the 95% confidence interval (CI). The chi-square test was used to determine whether differences in incidences were significant. Invasive disease confined to the cervix was categorized as localized; cancers that had spread beyond the cervix to regional nodes or metastasized to other sites were categorized as advanced. During 1992--1999, a total of 14,759 invasive cervical cancer cases were diagnosed (53% localized, 40% advanced, and 7% unstaged). After excluding 235 cases of persons with unknown ethnicity, the analysis included data from 14,524 invasive cervical cancer cases; 3,166 (22%) were among Hispanic women, and 11,358 (78%) were among non-Hispanic women. The incidence for invasive cervical cancer was 16.9 per 100,000 women (95% CI=16.2--17.5) for Hispanic women and 8.9 (95% CI=8.8--9.1) for non-Hispanic women (Table). Regardless of the stage of disease at diagnosis, incidences for Hispanic women were approximately twice those for non-Hispanic women in each year during 1992--1999 (Table). Overall incidences significantly decreased an average of 4.4% per year for Hispanic women and 2.0% per year for non-Hispanic women (Table). Incidences of localized-stage cancer declined 3.3% per year for Hispanic women (EAPC=-3.3; 95% CI=-6.0-- -0.6); the decline for non-Hispanic women was not significant (EAPC=-1.3; 95% CI=-2.9--0.4). Incidences of advanced-stage cancer declined 4.5% per year for Hispanic women (EAPC=-4.5; 95% CI=-6.9-- -2.0); the decline for non-Hispanic women was not significant (EAPC=-2.1; 95% CI=-4.4--0.2). Analyses of invasive cervical cancer incidences by age and stage at diagnosis indicated that, except for women aged 20--29 years, incidences for Hispanic women were significantly higher than those for non-Hispanic women, regardless of stage at diagnosis (Figures 1 and 2). For both Hispanic and non-Hispanic women, approximately 30% of all new invasive cervical cancers diagnosed among women aged <50 years were at an advanced stage; among women who were aged >50 years, advanced-stage cervical cancer represented 52% of new diagnoses. Reported by: LR Armstrong, PhD, HI Hall, PhD, PA Wingo, PhD, Div of Cancer Prevention and Control, National Center for Chronic Disease Prevention and Health Promotion; S Kassim, MD, EIS Officer, CDC. Editorial Note:The findings in this report indicate that in a population defined by 11 SEER registry areas, overall incidences of invasive cervical cancer are decreasing but that incidences remain relatively high for Hispanic women aged >30 years and for non-Hispanic women aged >50 years. The findings also indicate that women who have cervical cancer diagnosed at age >50 years are more likely to have advanced-stage cervical cancer. Analyses of cervical cancer incidence by stage at diagnosis contribute to the assessment of the impact of screening programs. Cervical cancer screening identifies precancerous lesions and prompts early treatment to prevent advanced-stage cancer and death (6). Risk factors for cervical cancer include early onset of sexual activity, having multiple sex partners, human papillomavirus infection, and smoking. However, the most important determinant of invasive cervical cancer occurrence is infrequent or no cervical cancer screening (6). The decrease in incidence of localized and advanced-stage cervical cancer for both Hispanic and non-Hispanic women in the United States reflects the widespread use of cervical cancer--screening services (6). Recent data indicate that increases in cervical cancer screening are greater for Hispanics than for non-Hispanics (National Cancer Institute, Division of Cancer Control and Population Science, unpublished data, 2002). To increase access to screening services for women who lack health insurance or who are underinsured, the Breast and Cervical Cancer Mortality Prevention Act was enacted in 1990 (7). During the 1990s, all states, territories, and Indian tribes, in collaboration with CDC, established cervical cancer--screening programs (7). Hispanics constitute the largest ethnic minority group in the United States, representing 12.5% of the general population (2000 U.S. Census Bureau, http://factfinder.census.gov). Overall, the incidence of cancer among Hispanics differs from those of other U.S. population groups (8). For invasive cervical cancer, analyses of the SEER data for 1988--1992 indicated that the incidence for Hispanic women was second only to that of Vietnamese women, which was more than twice the incidence for Hispanics (9). Analysis of the 1998 National Health Interview Survey indicated that the prevalence of Pap testing within the preceding 3 years was 80% for non-Hispanic white women, 83% for non-Hispanic black women, and 74% for Hispanic women (4). Barriers to using screening services among Hispanic women include older age, low education, low household income, and lack of health insurance (10). Nonuse of other screening tests (10) and unrecognized social-cultural factors also might play a role. Research is needed to better understand barriers to screening practices. The higher incidence of invasive cervical cancer among both Hispanic and non-Hispanic women aged >50 years and the greater likelihood that they have advanced disease might be a result of the low use of screening services among this population. Across all states, the use of Pap tests ranged from 84% to 93% among women of reproductive age (aged 18--44 years) and from 75% to 91% among older women (4). The findings in this report are subject to at least three limitations. First, SEER registries cover approximately 14% of the U.S. population and might not be representative of the general U.S. population (5). Second, although the U.S. Hispanic population comprises diverse communities, Hispanics identified by SEER registries represent 25% of the U.S. Hispanic population and are largely of Mexican origin (9). Third, the classification "non-Hispanic women" includes other minority groups (e.g., Asians/Pacific Islanders and blacks) who also have high incidences of cervical cancer. In the United States, the use of Pap tests has had an important impact on cervical cancer morbidity and mortality. The findings in this report suggest that Hispanic women aged >30 years and non-Hispanic women aged >50 years need improved access to screening services. To decrease incidence of advanced-stage cervical cancer, public health programs should target women with culturally appropriate interventions that encourage screening. For women with abnormal Pap test results, appropriate diagnostic and treatment services also should be accessible. References
Table  Return to top. Figure 1 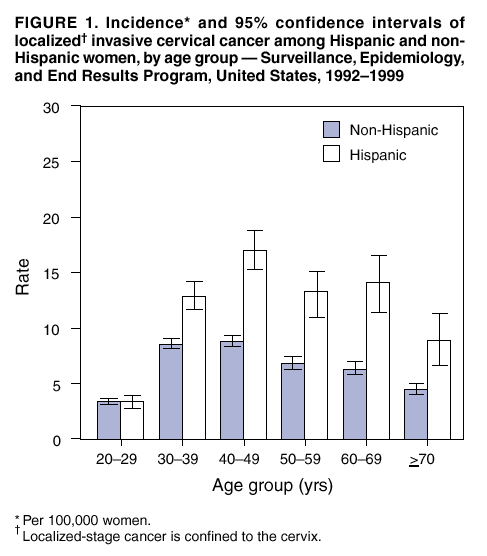 Return to top. Figure 2 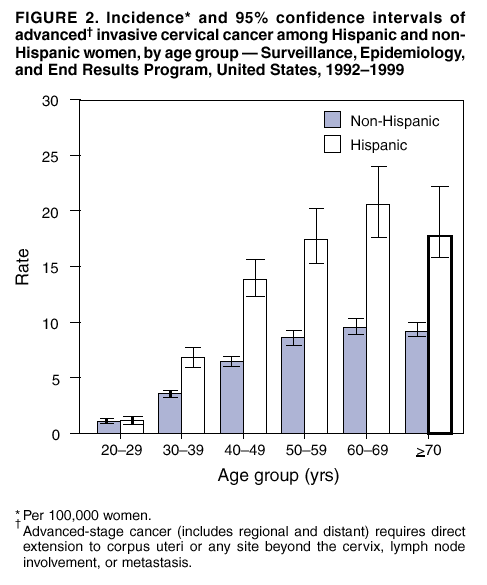 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 11/27/2002 |
|||||||||
This page last reviewed 11/27/2002
|