 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Hypothermia-Related Deaths --- Utah, 2000, and United States, 1979--1998Hypothermia is a medical emergency that is completely preventable (1). Hypothermia occurs when persons are exposed to ambient cold temperatures without appropriate protection for extended periods of time (1). The clinical definition of hypothermia is a core body temperature <95 F (35 C) (1). This report describes cases of hypothermia-related deaths in Utah during 2000 and describes unintentional hypothermia-related deaths in the United States during 1979--1998. The Utah cases illustrate risk factors and environmental conditions associated with hypothermia. Case ReportsCase 1. In February 2000, a man aged 50 years was found dead in an alley behind local businesses in urban Utah. The high temperature that day had been 50 F (10 C), and the low temperature had been 36 F (2 C) with 0.1 inch of precipitation. The decedent was a transient who overused alcohol. His postmortem blood alcohol level was 0.36 g/dL. The death certificate listed the cause of death as hypothermia attributed to acute and chronic alcoholism. Case 2. In March 2000, a man aged 27 years with a history of schizophrenia was found dead in a remote area of Utah. An investigation determined that his vehicle had become stuck in mud and he had become wet and cold while attempting to extricate the vehicle. The death certificate listed the cause of death as hypothermia. Case 3. In October 2000, a boy aged 2 years was left alone by his father in a vehicle in a remote area of Utah for approximately 45 minutes. When the father returned, the child was missing. Six days later, the child was found dead. During the 6 days the child was missing, snow and rain fell in the area. The high temperature on the first day the child was missing was 54 F (12 C), and the low temperature was 27 F (-3 C). The death certificate listed the cause of death as hypothermia attributed to exposure to low environmental temperatures. Case 4. In December 2000, a woman aged 74 years with Alzheimer disease wandered away from her nursing home in Utah. She was wearing her nightgown, was last seen alive at 6:30 a.m., and was found dead 3 hours later. The high temperature that day was 15 F (-9 C), and the low temperature was -2 F (-19 C) with snow on the ground. The death certificate listed the cause of death as hypothermia attributed to exposure to low environmental temperatures. United StatesU.S. data were obtained from the Compressed Mortality File (CMF), maintained by CDC's National Center for Health Statistics, and were prepared in accordance with the external cause-of-death codes from the International Classification of Diseases, Ninth Revision (ICD-9). CMF contains information from death certificates filed in the 50 states and the District of Columbia. During 1979--1998, a total of 13,970 deaths were attributed to hypothermia (ICD-9 codes E901.0, E901.8, and E901.9; excludes human-made cold E901.1). The death rate attributed to hypothermia for males is approximately three times that for females for every age group except for persons aged <15 years, and the elderly have the highest rates of death attributed to hypothermia (Figure 1). During 1979--1998, Utah reported 91 deaths attributed to hypothermia, with an age-adjusted rate of 0.4 per 100,000 population. During the same period, Illinois reported the most deaths (859), with an age-adjusted rate of 0.4. Alaska had the highest age-adjusted rate of 2.9, with 250 deaths attributed to hypothermia. Reported by: TC Grey, MD, Office of the Medical Examiner, R Rolfs, MD, Acting State Epidemiologist, Utah Dept of Health. MA Chambers, Western Regional Climate Center, Reno, Nevada. AS Niskar, MPH, Div of Environmental Hazards and Health Effects, National Center for Environmental Health, CDC. Editorial Note:The findings in this report indicate that hypothermia-related deaths in the United States increase with age and that rates are highest among men. In the cases presented in this report, all decedents had one or more risk factors for hypothermia-related death (e.g., aged >65 years, alcohol use, homelessness, and mental illness). The warning signs of hypothermia include shivering, confusion and disorientation, memory loss, drowsiness, exhaustion, fumbling hands and poor coordination, slurred speech, and numbness (1,2). Shivering is a sign that the body is losing heat and shivering decreases as body temperature falls; a person who shivers persistently should return indoors. Severe hypothermia results in unconsciousness, shallow breathing, weak pulse, and death. Warning signs of hypothermia in an infant include bright red, cold skin and lethargy. Persons with signs or symptoms of hypothermia should seek medical attention immediately (2). Until medical care becomes available, the person should be moved into a warm room or shelter and wet clothing removed. The center of the body should be warmed first, including the chest, neck, head, and groin using an electric blanket or skin-to-skin contact under loose, dry layers of blankets, clothing, towels, or sheets. Warm, nonalcoholic beverages can help increase body temperature, but they should not be given to an unconscious person. If the person does not appear to be breathing, does not have a pulse, and appears to be unconscious, cardiopulmonary resuscitation (CPR) should be administered in conjunction with warming efforts until the person responds or medical attention is available. Even if the person appears to be dead, CPR should be provided because, in some cases, persons with hypothermia who appear dead can be resuscitated. Alcohol use, homelessness, vehicle breakdown, psychiatric disorders, and Alzheimer disease are all risk factors associated with hypothermia. Factors such as neuromuscular disease, arthritis, hypothyroidism, malnutrition, beta-blocker use, neuroleptic use, and alcohol use decrease the body's ability to produce heat (1,3). Factors that can result in increased body heat loss include psoriasis, dermatitis, burns, dehydration, decreased subcutaneous fat, and alcohol use. Loss of body thermo-regulation can occur with central nervous system pathology, trauma, stroke, Parkinson disease, neuropathies, and spinal cord injuries. Elderly persons are more likely to have one or more risk factors, placing them at especially high risk for hypothermia. Children are particularly susceptible to hypothermia (4). Infants need sufficient blankets and clothing for insulation (1). Persons participating in outdoor activity might have impaired judgment from hypothermia, causing them to remain unprotected in situations of dangerous cold (1,5). An extremely cold environment is not necessary for hypothermia (1,6). Persons who participate in outdoor activities during cold weather should take precautions to avoid hypothermia. Persons can maximize heat production by voluntary muscular activity, shivering, eating to maintain calorie intake, and drinking nonalcoholic beverages to stay hydrated. Heat loss can be minimized by wearing a hat that does not retain moisture, a scarf or knit mask to cover the face and mouth, sleeves that are snug at the wrist, mittens, water-resistant coat and shoes to stay dry, and several layers of loose-fitting clothing (2,6). The outer layer of clothing should be tightly woven and wind resistant to reduce body heat loss caused by wind. Wool, silk, or polypropylene inner layers of clothing will hold more body heat than cotton. Persons who feel too warm should remove extra layers of clothing because excess perspiration will increase heat loss. In high wind, use of goggles can protect the corneas from freezing. Persons should avoid overexertion and overheating because of potential dehydration and the wetting effect of perspiration. Swimmers need insulating swimwear in cold water. Vehicle-safety precautions also can help prevent hypothermia (1,2). Vehicles should be equipped with cold weather gear for use during a breakdown. Travelers stranded during a winter storm should remain in their vehicle, stay awake, and wrap their entire bodies in extra clothing, blankets, or newspapers to stay warm. The motor and heater should be run for approximately 10 minutes per hour and one window should be opened slightly to let in air while making sure that snow is not blocking the exhaust pipe to reduce the risk for carbon monoxide poisoning. Persons should move their arms and legs to improve circulation and stay warmer, and avoid eating unmelted snow because it will lower body temperature. Public health prevention strategies for reducing hypothermia-related deaths include educating the public and health-care providers about heat preservation strategies and providing outreach programs that identify and protect persons at risk (e.g., the elderly, young children, mentally and physically disabled persons, persons with psychiatric disorders, and homeless persons) (1). Community outreach programs should check on these risk groups frequently to discourage prolonged exposure to cold and to ensure properly heated dwellings. Many hypothermia-related deaths might only be prevented with improvement in overall medical and social support services for vulnerable populations. Public health prevention strategies for reducing hypothermia should be part of a broader social support program to provide support services to populations at risk. References
Figure 1 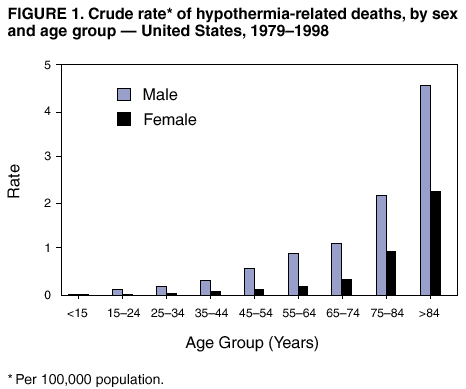 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 1/31/2002 |
|||||||||
This page last reviewed 1/31/2002
|