 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. State-Specific Prevalence of Current Cigarette Smoking Among Adults and the Proportion of Adults Who Work in a Smoke-Free Environment --- United States, 1999Tobacco use in the United States causes approximately 430,000 deaths each year, including an estimated 3000 deaths from lung cancer among nonsmokers exposed to environmental tobacco smoke (ETS) (1). In addition, an estimated 62,000 coronary heart disease deaths annually among nonsmokers exposed to ETS (2). The detrimental health effects of exposure to ETS are well documented and include, in addition to lung cancer and coronary heart disease among adults, low birthweight and sudden infant death syndrome from exposure during and after pregnancy and asthma, bronchitis, and pneumonia in children (2). This report summarizes the 1999 prevalence of current cigarette smoking among adults by state and the proportion of persons who work indoors and who report that their workplaces have smoke-free policies. The findings indicate that in 1999, adult smoking prevalence differed more than two-fold across states (13.9%--31.5%) and that the proportion of persons who reported that their workplace had an official smoke-free policy ranged from 61.3%--82.1%. As the respondents' level of education increased, they were more likely to report working under a smoke-free policy. State- and sex-specific prevalences of current cigarette smoking among adults were obtained from the Behavioral Risk Factor Surveillance System (BRFSS), a state-based, random-digit--dialed telephone survey of the noninstitutionalized U.S. population, aged >18 years. The 1999 BRFSS was conducted in the 50 states, the District of Columbia (DC), and Puerto Rico (PR). To determine current cigarette smoking, respondents were asked, "Have you ever smoked at least 100 cigarettes in your entire life?" and "Do you now smoke cigarettes every day, some days, or not at all?" Current smokers were defined as those who reported having smoked >100 cigarettes during their lives and who currently smoked every day or some days. Because BRFSS data were state-specific, median values rather than a national average were reported. Estimates were weighted to the age, race, and sex distribution of each state's population, and 95% confidence intervals were calculated by using SUDAAN. To assess workplace smoking policies, respondents who work indoors most of the time were asked: "Which of the following best describes your place of work's official smoking policy for indoor public or common areas, such as lobbies, rest rooms, and lunch rooms?" and "Which of the following best describes your place of work's official smoking policy for work areas?" Possible responses included "not allowed in any work (or public/common) areas," "allowed in some work (or public/common) areas," "allowed in all work (or public/common) areas," and "no official policy." A smoke-free policy was defined as a policy that did not permit smoking in the common, public, or work areas of the workplace. The percentage of respondents who reported smoke-free workplace policies was calculated and reported by state and by respondents' education level. In 1999, the adult prevalence of current cigarette smoking differed more than twofold across the states (range: 13.9%--31.5%), with a median of 22.7% (Table 1). Current cigarette smoking prevalence was highest in Nevada (31.5%), Kentucky (29.7%), and Ohio (27.6%) and lowest in Utah (13.9%), Hawaii (18.6%), California (18.7%), Massachusetts (19.4%), and Minnesota (19.5%). Smoking prevalence in PR (13.7%) was lower than the overall prevalence in the 50 states. The median smoking prevalence among men was 24.2% (range: 16.6%--33.9%) and among women was 20.9% (range: 11.4%--30.3%). Current smoking prevalence was highest among men in Kentucky (33.9%) and women in Nevada (30.3%); Utah had the lowest current smoking prevalence among both men (16.6%) and women (11.4%). Respondents in 17 states and DC were asked questions on the protection provided by official workplace nonsmoking policies (Table 2). Among respondents who primarily worked indoors (median: 75.2%), the proportion who reported an official workplace policy that addressed smoking in public, common, or work areas ranged from 87.1%--97.1% (median: 92.3%); the proportion who did not know the policies or refused to answer ranged from 0.1%--1.4% (median: 0.7%). The proportion of respondents who reported a smoke-free workplace policy ranged from 61.3% in Mississippi to 82.0% in DC (median: 73.0%). The proportion increased as the level of education increased: among high school graduates or less education, the range was 48.2%--82.4% (median: 63.2%); among those with some college education, the range was 60.7%--84.5% (median: 72.4%); and among college graduates or more education, the range was 68.9%--89.1% (median: 84.1%). Reported by the following BRFSS coordinators: S Reese, MPH, Alabama; P Owen, Alaska; B Bender, MBA, Arizona; G Potts, MBA, Arkansas; B Davis, PhD, California; M Leff, MSPH, Colorado; M Adams, MPH, Connecticut; F Breukelman, Delaware; I Bullo, District of Columbia; S Hoecherl, Florida; L Martin, MS, Georgia; F Reyes-Salvail, MS, Hawaii; J Aydelotte, MA, Idaho; B Steiner, MS, Illinois; L Stemnock, Indiana; J Davila, Iowa; C Hunt, Kansas; T Sparks, Kentucky; B Bates, MSPH, Louisiana; D Maines, Maine; A Weinstein, MA, Maryland; D Brooks, MPH, Massachusetts; H McGee, MPH, Michigan; N Salem, PhD, Minnesota; D Johnson, MS, Mississippi; J Jackson-Thompson, PhD, Missouri; P Feigley, PhD, Montana; L Andelt, PhD, Nebraska; E DeJan, MPH, Nevada; L Powers, MA, New Hampshire; G Boeselager, MS, New Jersey; W Honey, MPH, New Mexico; C Baker, New York; Z Gizlice, PhD, North Carolina; L Shireley, MPH, North Dakota; P Pullen, Ohio; K Baker, MPH, Oklahoma; K Pickle, MPH, Oregon; L Mann, Pennsylvania; Y Cintron, MPH, Puerto Rico; J Hesser, PhD, Rhode Island; M Wu, MD, South Carolina; M Gildemaster, South Dakota; D Ridings, Tennessee; K Condon, MS, Texas; K Marti, Utah; C Roe, MS, Vermont; K Carswell, MPH, Virginia; K Wynkoop Simmons, PhD, Washington; F King, West Virginia; K Pearson, Wisconsin; M Futa, MA, Wyoming. Cardiovascular Health Br, Div of Adult and Community Health, National Center for Chronic Disease Prevention and Health Promotion; Office on Smoking and Health, National Center for Chronic Disease Prevention and Health Promotion, CDC. Editorial Note:The prevalence of smoking among adults leveled off in the 1990s following a steady decline since the mid-1960s (3), and a wide range of smoking prevalence persists among states. Both Utah and PR have achieved the national health objective for 2000 of reducing the prevalence of cigarette smoking in adults to <15% (4). BRFSS data on smoking in PR are being reported for the first time. PR's overall median prevalence of 13.7% was lower than the 26.9% prevalence among persons of Puerto Rican descent living in the United States (CDC, unpublished data, 2000). Additional research is needed to clarify whether the twofold difference can be attributed to factors related to acculturation among persons from PR residing the United States or to other factors specific to the population sampled in PR. The exclusion of 25% of households that do not have telephones in PR also could have contributed to the difference in prevalence estimates. The proportion of respondents who reported that smoking was not permitted in either the public or work areas in the Current Population Survey (CPS) increased from 46.5% in 1992--1993 to 63.7% in 1995--1996 (5). The 1999 BRFSS findings suggest that the proportion of respondents who report a smoke-free environment continues to increase. In addition, the association between increasing level of education and working in a smoke-free workplace is consistent with findings from CPS (5). Findings from the 1992--1993 CPS also showed substantial differences in the proportion of workers who reported smoke-free policies among various occupational groups (6). The findings in this report are subject to at least four limitations. First, smoking data are based on self-reports without biochemical verification. Second, previous studies have shown that persons with less than a high school education have higher rates of smoking (7); however, sample size considerations led to the combining of respondents with less than a high school education and high school graduates. Third, respondents' definitions of "official policy" may vary, and the validity of self-report of workplace policies is unknown. Fourth, PR's smoking prevalence was determined from a sample of households with telephones, which represents approximately 75% of the population (D. Zavala, MD, Puerto Rico Department of Health, personal communication, 2000). Momentum to regulate public smoking began to increase in 1990 when the Environmental Protection Agency released its publication draft Risk Assessment on Environmental Tobacco Smoke (ETS), classifying ETS as a Group A carcinogen that can cause lung cancer in nonsmokers (5). Government and private business policies that limit smoking in public workplaces have become increasingly common and restrictive (5). In 1999, laws restricting smoking in government work sites were in effect in 43 states and DC: 11 prohibit smoking, and two require either no smoking or designated smoking areas with separate ventilation (7). Twenty-one states have laws restricting smoking in private work sites, but only one requires either no smoking or separate ventilation for smoking areas (7). During 1998--1999, 79% of work sites with >50 employees had formal policies that prohibited smoking or limited it to separately ventilated areas (8). Information on the prevalence of smoking policies in workplaces with <50 employees, where most U.S. adults work, is not readily available (7). In addition to reducing smoking by adolescents and adults, public health initiatives should reduce exposure to ETS. Healthy People 2010 contains objectives related to reducing the proportion of nonsmokers exposed to environmental smoke, increasing the proportion of work sites with restrictive policies, and increasing the number of states with smoke-free indoor air laws (8). Policy approaches, including the voluntary adoption of work site restrictions, enactment of restrictive clean indoor air laws, and enforcement of restrictions are effective in reducing the number of persons exposed to ETS (7). Smoke-free workplace policies reduce exposure of nonsmokers to ETS and increase the likelihood that smokers in these settings will smoke fewer cigarettes or quit (7). Persistent disparities in exposure to ETS at the work place must be addressed (8). To meet the national ETS-related objectives for 2010, states need to implement comprehensive programs that protect nonsmokers from ETS and follow the recommendations in the CDC report Best Practices for Comprehensive Tobacco Control Programs and the 2000 Surgeon General's report on reducing tobacco use (7,9). References
Table 1  Return to top. Table 2 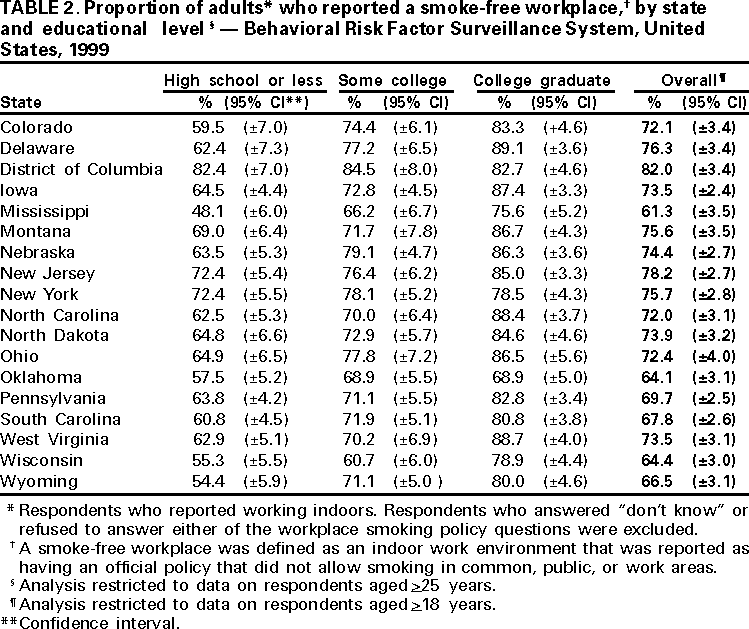 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 11/2/2000 |
|||||||||
This page last reviewed 5/2/01
|