 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Progress Toward Global Dracunculiasis Eradication, June 2000In 1986, an estimated 3 million persons were infected with dracunculiasis (Guinea worm disease) and another 120 million were at risk for infection (1). That year and in 1991, the World Health Assembly called for the eradication of dracunculiasis (2,3), and as a result of the implementation of the Dracunculiasis Eradication Program (DEP)*, the annual incidence was reduced by approximately 95% by 1995 (4). This report updates the status of the eradication program as of June 2000, which indicates that dracunculiasis has been eliminated from seven of 20 countries where it was endemic in 1995; however, in parts of Africa, particularly Sudan, dracunculiasis remains a serious public health problem. For surveillance purposes, village-based health workers search for infected persons in each village with endemic disease and complete a register that provides the basis for monthly zonal, district, and national surveillance reports (5). During 1999, dracunculiasis was endemic in 13 countries in Africa†. These countries reported 96,293 cases in 10,914 villages. Of the total number of cases, Sudan reported 66,097 (69%) cases in 7271 villages; 2606 of the known villages with endemic disease in Sudan were not accessible to program surveillance. Outside Sudan, 93% of 3068 villages reported monthly; in Sudan, 44% of 4892 accessible villages reported monthly. Outside Sudan, 20% of all villages with endemic disease reported 1 case each. Seven of the 13 countries with endemic disease reported <500 cases each in 1999 (Figure 1). During January--June 2000, the number of cases reported by all countries except Sudan was 12,097, 18% less than the 14,828 cases reported during the same period in 1999. The rate of reduction in all countries outside of Sudan was 35% except in Ghana, which reported a slight increase in cases during the first half of 2000. Niger reported 59% fewer cases during January--June 2000. Benin, Cote d'Ivoire, Ethiopia, Mali, Mauritania, and Uganda have reduced the number of cases by an average of 55% during January-- June 2000. Nigeria reported 35% fewer cases during January--June 2000 than during the same period in 1999. All programs attempt to control the spread of disease using case containment (i.e., patients were not allowed to contaminate water and transmit infection) aimed at detecting cases within 24 hours of emergence of the worm and instituting prevention measures immediately. Approximately 62% of the case-patients reported outside of Sudan during 1999 were contained; 68% were contained during January--June 2000. The long-standing civil war in Sudan is the primary reason for the high rate of dracunculiasis in the southern part of that country; however, the 10 northern states of Sudan have reported 66% fewer cases during the first 6 months of 2000 compared with the same period last year (21 versus 61 cases); 16 (76%) of the 21 cases were contained. Reported by: Global 2000, The Carter Center, Atlanta, Georgia. World Health Organization Collaborating Center for Research, Training, and Eradication of Dracunculiasis. Div of Parasitic Diseases, National Center for Infectious Diseases, CDC. Editorial Note:Dracunculiasis is a parasitic infection acquired by drinking water from ponds contaminated by copepods (water fleas) that contain immature forms of the parasite. A year after entering the infected person, the 40-inch (1 meter) worm(s) emerge, usually on the lower limbs through skin wounds that frequently become contaminated secondarily. Reinfection can occur if the person again drinks contaminated water. No effective treatment exists; however, two countries in which dracunculiasis was endemic at the beginning of the program (Pakistan and India) have been certified by the World Health Organization (WHO) to have interrupted transmission. WHO also has certified the absence of transmission from almost all countries outside Africa (Figure 2) (6). All countries with endemic disease are required to submit a report to the International Commission for the Certification of Dracunculiasis Eradication, documenting the absence of indigenous cases of the disease for at least 3 consecutive years to be recommended for certification. Most eradication programs have begun listing villages with endemic disease in descending order of number of cases reported to help monitor the status of interventions. Nylon filters have been distributed to all households in 47% of villages with known endemic disease, including 67% outside Sudan. The larvicide Abate®§ (temephos) (American Home Products, Princeton, New Jersey) is being used in approximately 35% of villages with endemic disease outside Sudan, and 43% of villages with endemic disease outside Sudan have access to at least one source of safe drinking water (Table 1). Health education and community mobilization activities (e.g., radio announcements; posters; town criers; and talks by religious, political, and traditional leaders) aimed at persons in villages endemic with disease or at high risk for disease have been intensified. The current goal of DEP is to eliminate transmission in all remaining countries with endemic disease outside Sudan by 2001. An estimated 3 to 4 years of intense activities will be required to halt dracunculiasis transmission after a peace agreement is signed in Sudan. To attain these targets, ministries of health in the remaining countries with endemic disease must make dracunculiasis eradication a top national, regional, and local public health priority. The infection can be prevented by teaching at-risk persons to filter their drinking water through a finely woven cloth, to avoid entering sources of water when worms are emerging, by treating water sources with Abate to kill copepods, or by providing clean drinking water from sources such as borehole wells. Each national program needs to intensify supervision and motivation of village-based health workers, ex tend and diversify efforts to educate and mobilize villagers in communities with endemic disease, advocate for provision of safe water sources to villages with endemic disease, monitor the status of all interventions, and ensure that active surveillance is maintained in all communities with endemic disease and in areas at risk for dracunculiasis. References
* Program partners include The Carter Center, CDC, United Nations Children's Fund (UNICEF), the World Health Organization (WHO), ministries of health in countries where dracunculiasis is endemic, private industry, and many other donors, including the Bill and Melinda Gates Foundation. † Benin, Burkina Faso, Central African Republic, Cote d'Ivoire, Ethiopia, Ghana, Niger, Nigeria, Mali, Mauritania, Sudan, Togo, and Uganda. § Use of trade names and commercial sources is for identification only and does not constitute endorsement by CDC or the U.S. Department of Health and Human Services. Table 1 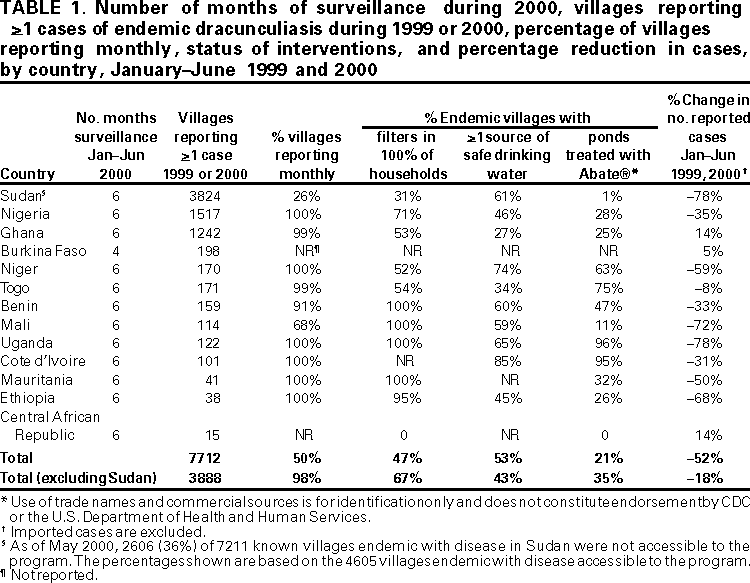 Return to top. Figure 1 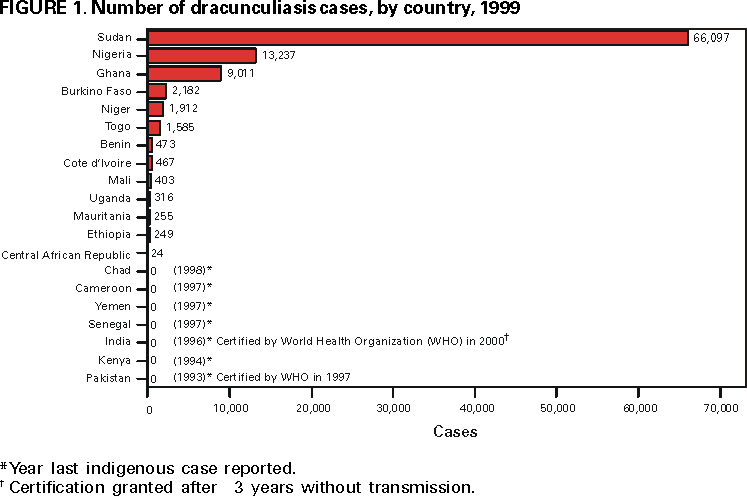 Return to top. Figure 2 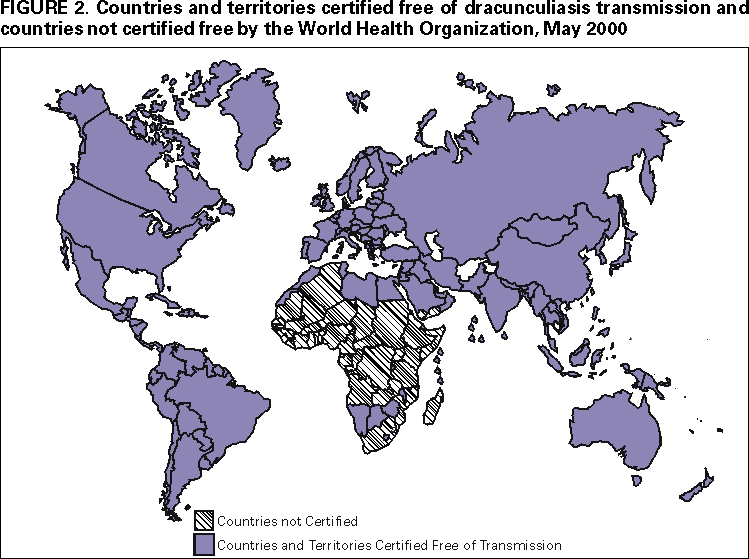 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 8/17/2000 |
|||||||||
This page last reviewed 5/2/01
|