 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Use of Hospital Discharge Data to Monitor Uterine Rupture --- Massachusetts, 1990--1997Uterine rupture (UR), a potentially life-threatening condition for both mother and infant, occurs in <0.1% of all pregnant women and <1% of women attempting vaginal birth after cesarean section (VBAC) (1--4). During 1990--1997, the proportion of vaginal deliveries among women who had previous cesarean sections (CS) in Massachusetts increased 50%, from 22.3% to 33.5% (5). Concern about a corresponding increase in UR prompted the Massachusetts Department of Public Health and CDC to initiate a statewide investigation that included an assessment of the validity and reliability of International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) (6), codes in hospital discharge data to identify UR cases. This report summarizes the results of the investigation, which indicate that ICD-9-CM codes related to UR, designed before increased concern about UR, lack adequate specificity for UR surveillance and have not been applied consistently over time. Using 1990--1997 state hospital discharge data, suspected UR cases were identified based on three ICD-9-CM diagnostic codes (6). Suspected cases were defined as women discharged from Massachusetts hospitals from 1990 through 1997 with an ICD-9-CM diagnostic code in any of the 10 diagnostic fields of 665.0 ("rupture of uterus before onset of labor"), 665.1 ("rupture of uterus during labor," including "rupture of uterus not otherwise specified"), or 674.1 ("disruption of cesarean wound," including "dehiscence or disruption of uterine wound"). Women with and without a history of CS were included. The four-digit ICD-9 codes 665.0 and 665.1 are contained within the larger three-digit category of code 665, "other obstetrical trauma," that also includes "damage from instruments." In addition, the ICD-9-CM index directs coders to use 665.1 for "laceration of the uterus, obstetrical trauma not elsewhere classifiable (NEC)," a frequent incidental complication that occurs during delivery of the fetus through the uterine incision. To identify cases of UR, hospital medical records of suspected cases, including registration sheets, discharge summaries, and surgical reports, were obtained and reviewed by two clinicians to confirm a UR. UR was defined as any unintentional disruption of the uterine wall in a pregnant woman regardless of cause, size, degree of severity, or location and was described in the hospital chart as a rupture, dehiscence, separation, window, or rent. URs occurring in women with and without prior CS scars were included. Incidental extensions or lacerations of a uterine incision during a CS, postpartum separation of the uterine scar resulting from infection, or extremely thin lower uterine segments without disruption of the uterine wall were not considered URs. Positive predictive values (PPVs) were calculated as the number of confirmed cases divided by the number of reviewed suspected cases multiplied by 100. PPVs were calculated for codes 665.0 and 665.1 combined, for code 674.1, and for all three codes combined, by year and overall. From 1990 through 1997, 1244 suspected cases were identified. Of these, 608 (48.8%) had ICD-9-CM code 665.0 or 665.1, 629 (50.5%) had code 674.1, and seven (1.0%) were coded with both 665.1 and 674.1 (Table 1). Of the 1207 (97.0%) hospital records that were reviewed, 480 (39.8%) cases were confirmed as URs. Among the confirmed cases of UR, 442 (92.1%) occurred among women with at least one previous CS, 33 (6.9%) among women with an unscarred uterus, and five (1.0%) among women who had another type of uterine scar (e.g., myomectomy). The average PPV during the 8-year period was 50.7% for ICD-9-CM codes 665.0 and 665.1 and 28.6% for code 674.1. The overall PPV of the three codes was 39.8%. The number of suspected UR cases coded with 665.0 or 665.1 increased steadily from 1990 through 1997. However, the number of confirmed cases and PPV increased during 1990--1994, but from 1994 through 1997 the number fluctuated while PPV declined. The number of suspected and confirmed cases and the PPV of ICD-9-CM code 674.1 remained relatively stable during the same time period. Of the 726 suspected cases confirmed as nonruptures, 694 (95.6%) of the charts contained enough information to identify a reason for the use of one of the three diagnostic codes for UR. Codes were used correctly in 81.3% of the nonrupture charts to record a condition that falls within the ICD-9-CM definitions. Among the 19.7% of records where the codes were not used correctly, 14.0% were miscoded (i.e., a condition was recorded that should have been coded with a different ICD code), 4.0% were data entry errors, and 0.6% could not be categorized because no condition mentioned in the chart appeared to be related to one of the three ICD-9-CM codes (Table 2). Reported by: J Weiss, ScD, A Nannini, PhD, S Fogerty, MEd, Bur of Family and Community Health, Massachusetts Dept of Public Health; B Sachs, MD, Beth Israel Deaconess Medical Center; F Frigoletto, MD, D Roberts, MD, Massachusetts General Hospital; S Ringer, MD, Brigham and Women's Hospital, Boston; S DeJoy, CNM, JP O'Grady, MD, Baystate Medical Center, Springfield; G Kraus, MD, Anna Jaques Hospital, Newburyport; J Weber, CNM, Midwives of the Merrimack Valley, North Andover, Massachusetts. Div of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion; Div of Applied Public Health Training, Epidemiology Program Office; and an EIS Officer, CDC. Editorial Note:Administrative information, such as hospital discharge data, is often used for surveillance purposes. This study indicates that hospital discharge data alone cannot be used to monitor trends in UR because ICD-9-CM codes lack the required specificity and consistency in application. However, even though the PPV of codes 665.0 and 665.1 was higher than the PPV of code 674.1, the number of URs would have been undercounted by one third without including records with diagnostic code 674.1. The purpose of the ICD-9 and the ICD-9-CM classification systems is to place conditions into relevant categories for statistical purposes (6,7). ICD-9-CM is adapted from ICD-9, which was published in 1977 before concern about rising CS rates. It was not designed to monitor UR as a complication of labor; therefore, the low overall PPVs can be explained by including other conditions in ICD-9-CM codes 665.0, 665.1, and 674.1. Reasons for the decline in the PPV of ICD-9-CM codes 665.0 and 665.1 during 1994--1997 are unclear but may represent changes in coding practices, an actual shift in clinical outcomes, or a combination of both. Coding practices may have been affected by obstetric coding guidelines issued in 1995 by CDC's National Center for Health Statistics to standardize the application of ICD-9-CM codes across facilities, and by changes in obstetric reimbursement policies that may have encouraged more extensive reporting. Clinical outcomes may have been affected by a decline in the proportion of births delivered by CS and an increase in VBACs. International Classification of Diseases and Related Health Problems, 10th Revision (ICD-10) was published in 1992, also before increased concern about URs, and is scheduled to replace ICD-9-CM for coding of morbidity in 2005. However, ICD-10 does not address the lack of specificity of codes to identify UR cases accurately (8). Future revisions to ICD-10 and ICD-10-CM should include a code specifically for "uterine rupture associated with previous CS scar." An alternate data source for monitoring URs will be the revised national standard certificate of live birth, scheduled to go into use in 2003. It will contain a checklist for maternal morbidity including UR. This data source will need to be validated for its sensitivity and specificity through medical records review. VBAC generally is considered safe practice, and 75% of women attempting a VBAC are successful (2). However, the greatest risk factor for UR is labor among women with a previous CS. The findings in this report indicate that the number of URs increased from 1990 to 1994, with a notable increase from 1993 to 1994. This pattern is similar to the change in the proportion of VBACs among women with a previous CS. Data to estimate the frequency of VBAC attempts are unavailable; therefore, the risk for UR among women attempting VBAC is unknown. The incidence of UR may have been higher than that reported in this study. The negative predictive value of the three diagnostic codes is unknown because the probability that persons who were not reported to have a UR were free of UR could not be ascertained. In addition, the severity of UR varies from inconsequential to catastrophic; therefore, minor cases may remain clinically undetected and unreported. The need to monitor and assess the competing risks for morbidity associated with different methods of delivery will continue to be important. References
Table 1  Return to top. Table 2 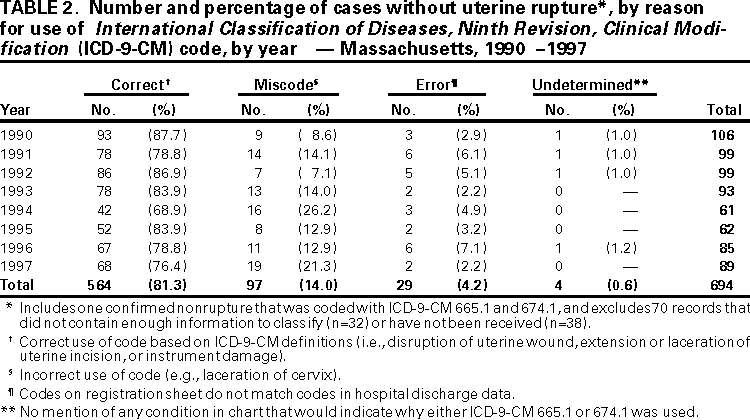 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 3/30/2000 |
|||||||||
This page last reviewed 5/2/01
|