 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Outbreak of Cryptosporidiosis Associated with a Water Sprinkler Fountain -- Minnesota, 1997Cryptosporidiosis associated with recreational water exposure is becoming recognized more frequently (1). This report summarizes the investigation of a large outbreak of cryptosporidiosis associated with exposure to a water sprinkler fountain at the Minnesota Zoo. The initial cases were not diagnosed as cryptosporidiosis by the health-care system despite patients seeking care, underscoring the need for increased awareness of cryptosporidiosis and routine laboratory diagnostic practices among health-care providers. On July 10, 1997, the Minnesota Department of Health (MDH) was notified by a parent about four cases of gastroenteritis among a group of 10 children whose only common exposure was a birthday party at the Minnesota Zoo on June 29. The zoo provided MDH with a list of registered groups that had visited the zoo during June 28-30; group members were contacted and interviewed about illness and zoo exposures. Initially, cases were defined as vomiting or diarrhea (defined as three or more loose stools during a 24-hour period) in persons who visited the zoo. Of 120 zoo visitors identified through the registered groups, 11 (9%) had illnesses that met the case definition. All had played in a water sprinkler fountain at the zoo, compared with seven (6%) of 109 controls (relative risk=undefined; p less than 0.001). Cryptosporidium oocysts were identified in nine of 10 stool specimens of case-patients tested at MDH. Two of the laboratory-confirmed case-patients had submitted stool samples previously for ova and parasite examination to their health-care providers; both samples were reported as negative for parasites. The fountain was closed on July 11, and MDH issued a public statement advising persons who had visited the zoo and subsequently developed diarrheal illness to contact their physician and MDH. The public statement also stated that children who developed diarrhea after exposure to the fountain should not visit swimming beaches, swimming and wading pools, and other recreational water facilities until at least 2 weeks after recovery from diarrheal symptoms. MDH requested that all clinical laboratories in Minnesota specifically test all stools submitted for ova and parasite examination for Cryptosporidium, particularly during the outbreak. A standard questionnaire was used to document illness history and zoo exposures in persons responding to the public statement. A revised case definition included persons with vomiting or diarrhea persisting at least 3 days, with onset 3-15 days after exposure to the zoo fountain. A total of 369 cases were identified, including the initial 11 cases; 73 (20%) were laboratory confirmed. Petting zoo exposure was reported by 191 (58%) of 332 case-patients, including 37 (55%) of 67 laboratory-confirmed cases. Age data were available for 351 case-patients; the median age was 6 years (range: 0-65 years), and 333 (95%) case-patients were aged less than or equal to 10 years. All but one of the 369 patients reported diarrhea; 317 (86%), abdominal cramps; 287 (78%), vomiting; 233 (63%), fever; and 11 (3%), bloody stools. The median duration of illness was 7 days. Six (2%) patients were hospitalized. Reported dates of fountain exposure for case-patients were from June 24 through July 11 (Figure_1). Exposure dates for confirmed case-patients were from June 28 through July 1, with 68 (93%) exposures occurring from June 29 through July 1 (Figure_1). The median incubation period after fountain exposure was 6 days. In addition to case-patients with fountain exposure, nine laboratory-confirmed cases of cryptosporidiosis were identified among household contacts of case-patients with fountain exposure. The implicated water sprinkler fountain was designed and built as a decorative display in 1994. The fountain is comprised of 14 nozzles arranged in five rows and submerged beneath metal grates. The nozzles sprayed jets of water vertically approximately one to six feet. The water drained through the grates, collected in trenches, passed through a sand filter, was chlorinated, and then recirculated. The zoo routinely replaced the water every Monday, Wednesday, and Friday, but the filter was not flushed. Environmental health inspectors from MDH recommended the fountain not be used as an interactive play area. The zoo subsequently erected a fence around the fountain plaza and reopened it as a decorative display only. Water samples collected on July 14 were negative for Cryptosporidium oocysts. The source of contamination of the fountain was not established, but contamination by a child wearing a diaper and playing in the fountain was suspected. Animals (including ruminants) in a petting zoo approximately 50 yards from the fountain tested negative for Cryptosporidium before being placed in the petting area and again during the outbreak investigation. A 1997 survey of all clinical laboratories serving Minnesota residents indicated that 13 (22%) of 59 laboratories that perform ova and parasite examinations on site routinely test for Cryptosporidium as part of ova and parasite examinations (i.e., without a specific request from a physician). In a 1997 survey of physicians in Minnesota, 44 (79%) of 56 physicians who thought that their laboratory always tested for Cryptosporidium as part of an ova and parasite examination were incorrect. Reported by: VC Deneen, MS, PA Belle-Isle, CM Taylor, LL Gabriel, JB Bender, DVM, JH Wicklund, MPH, CW Hedberg, PhD, MT Osterholm, PhD, State Epidemiologist, Minnesota Dept of Health. Div of Parasitic Diseases, National Center for Infectious Diseases; Div of Applied Public Health Training, Epidemiology Program Office; and an EIS Officer, CDC. Editorial NoteEditorial Note: The findings in this report document a novel recreational water source for cryptosporidiosis. Outbreaks of cryptosporidiosis have been documented in a variety of other recreational water settings in the United States since 1988, including a lake, community and hotel pools, a large recreational water park, a wave pool, and a water slide (1). As in several other outbreaks, there was no evidence in this outbreak that inadequate chlorination or filter malfunction contributed to transmission of Cryptosporidium. However, Cryptosporidium oocysts are resistant to disinfection by chlorine at levels generally used in recreational water, and recreational water filtration units that use sand filter media are not effective in removing the 4-6-micron oocysts (1). The zoo fountain in this outbreak was designed as a decorative display and not an interactive play area. However, the fountain was a popular attraction for children on hot summer days. Children would commonly stand directly over the jets and soak their entire bodies, a practice which could explain contamination of the fountain and subsequent transmission associated with ingestion of water. Consumption of foods while walking in the fountain plaza was also a common practice. Measures that might have reduced the risk for Cryptosporidium contamination of the fountain (e.g., showering before entering the fountain, excluding persons with diarrhea or incontinence, excluding children wearing diapers, and restricting food consumption in the fountain area) were not required or encouraged. Exclusion of persons from decorative water displays not designed for interactive use should be instituted and enforced. For recreational water facilities designed for human use, improved filtration may reduce risk. Waterborne cryptosporidiosis is probably underrecognized and underreported (1). Laboratory and physician surveys conducted in Minnesota indicate that most laboratories do not routinely test specifically for Cryptosporidium as part of ova and parasite examinations, even though many physicians assumed that they did. Even though cryptosporidiosis is reportable in Minnesota, this large outbreak probably would have remained undetected if not for the parent reporting the cases to the health department. Two of the original ill children had seen physicians, who ordered ova and parasite examinations; however, cryptosporidiosis remained undiagnosed until stool samples were examined specifically for Cryptosporidium at MDH. Because of their small size, Cryptosporidium oocysts can be difficult to detect by routine ova and parasite examination. The magnitude of this outbreak was probably determined only because of the public statement and the request that laboratories test all stools submitted for ova and parasite examination specifically for Cryptosporidium. To better understand the magnitude of cryptosporidiosis, health-care providers should specifically request testing for suspected cryptosporidiosis. Laboratories should consider routinely testing for Cryptosporidium as part of their ova and parasite examination protocol. Alternatively, when reporting test results back to health-care providers, laboratories should specifically indicate when Cryptosporidium is not tested for as part of a requested ova and parasite examination. Cryptosporidiosis is reportable in 41 states; interpretation of national data would be facilitated by mandatory reporting in all states. Reference
Figure_1 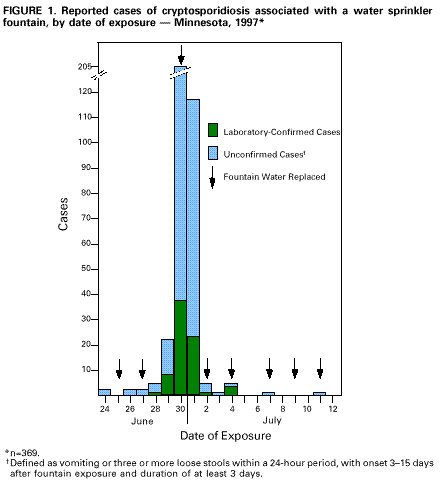 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 11/10/98 |
|||||||||
This page last reviewed 5/2/01
|