 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Outbreak of Vibrio parahaemolyticus Infections Associated with Eating Raw Oysters -- Pacific Northwest, 1997During July-August 1997, the largest reported outbreak in North America of culture-confirmed Vibrio parahaemolyticus infections occurred. Illness in 209 persons was associated with eating raw oysters harvested from California, Oregon, and Washington in the United States and from British Columbia (BC) in Canada; one person died. This report summarizes the investigations of the outbreak, which suggest that elevated water temperatures may have contributed to increased cases of illness and highlights the need for enhanced surveillance for human infections. British Columbia During July 1-19, the BC Provincial Laboratory received isolates of V. parahaemolyticus from nine patients, more than twice the expected number for July. Because of the high number of isolates identified, the BC Center for Disease Control (BCCDC) conducted interviews with the eight patients who could be contacted; seven had eaten raw oysters during the 24 hours before illness onset, and one had eaten crabs. On July 30, the BC Ministry of Health (BCMOH) issued a public health alert advising that molluscan shellfish (e.g., oysters, clams, mussels, and scallops) should not be eaten raw or undercooked. On July 31, the Vancouver/Richmond Health Board banned the sale of raw molluscan shellfish in restaurants in the cities of Vancouver and Richmond, BC. These actions were followed by a rapid decline in the number of new cases. On August 19, the Federal Department of Fisheries and Oceans (DFO) closed all BC coastal waters to the harvesting of oysters. The BCMOH continued to interview BC residents with culture-confirmed V. parahaemolyticus infections; information was obtained from 42 of the 51 persons with illness reported during July 1-September 26. Of the 42, a total of 39 (93%) had eaten molluscan shellfish and 35 (83%) had eaten raw or undercooked oysters during the 4 days before onset of illness; 28 had eaten oysters purchased at restaurants or other food establishments in BC; and seven had eaten oysters they had harvested. Oysters eaten by ill persons were traced by BCCDC, the Canadian Food Inspection Agency (CFIA), and BCMOH to harvesting areas along the BC coast. Samples of oysters harvested from these areas contained multiple V. parahaemolyticus serotypes at less than 200 colony-forming units (CFU) per gram of oyster tissue. No additional outbreak-related illnesses were reported in BC residents after DFO closed the coastal waters to the harvesting of oysters. The closure remained in effect until September 12, after which no additional cases were reported. Washington On July 18, on the basis of reports of illness received from local health departments and from ill persons, the Washington Department of Health (WDOH) issued an advisory that persons eat only thoroughly cooked oysters. On August 14, after additional cases had been reported, the WDOH advised commercial harvesters to refrigerate oysters within 4 hours after harvesting, and on August 20, advised the public to thoroughly cook molluscan shellfish from both commercial and noncommercial sources. On August 23, the U.S. Food and Drug Administration (FDA) also issued a statement regarding proper procedures for cooking oysters (1). WDOH interviewed 54 of the 56 persons who had culture-confirmed V. parahaemolyticus during May 26-September 9. Of the 54, a total of 48 (89%) had eaten molluscan shellfish before becoming ill; 42 (88%) reported eating oysters. Product traceback by the WDOH's Shellfish Program determined that 35 case-patients had eaten molluscan shellfish harvested in Washington. On August 20, members of the Pacific Coast Oyster Growers Association voluntarily halted shipments of shell oysters from Washington, and on August 28, WDOH closed oyster beds in major shellfish harvesting areas. The oyster beds were reopened on September 15, and no additional illnesses were reported. Oregon On August 21, the Oregon Health Division (OHD) requested that local county health departments and microbiology laboratories provide immediate notification of illnesses associated with or isolations of V. parahaemolyticus. The request was prompted by an increased number of V. parahaemolyticus cases detected by the Foodborne Disease Active Surveillance Network (FoodNet) (a collaboration between CDC, the U.S. Department of Agriculture, FDA, and seven states for surveillance of foodborne diseases and related epidemiologic studies) and simultaneous reports from BC and Washington of a V. parahaemolyticus outbreak associated with eating raw or undercooked shellfish. OHD interviewed the 13 persons reported with culture-confirmed V. parahaemolyticus infections with onsets during July 19-September 27. Twelve had eaten molluscan shellfish; 10 (77%) had eaten raw oysters. Traceback of the oysters that had been eaten indicated they had been harvested in waters near BC (four cases), Washington (four), Oregon (one), and California (one). On August 26, the implicated oyster harvest bed in Oregon was closed by the Oregon Department of Agriculture; only oysters to be cooked could be harvested. On August 28, OHD, in conjunction with the Food Safety Division of the Oregon Department of Agriculture, issued a press release warning persons not to eat raw molluscan shellfish harvested along the Pacific Northwest coast. After closure of the implicated oyster harvest bed in Oregon, no additional cases associated with eating raw oysters harvested from Oregon waters were reported. The sale of oysters to be eaten raw was reestablished on September 30. California During May-July, the City and County of San Francisco Department of Public Health reported 11 culture-confirmed V. parahaemolyticus infections to the California Department of Health Services (CDHS). On the basis of these cases, on August 18, San Francisco health officials issued a health advisory recommending that persons not eat raw shellfish and advising restaurants not to serve raw oysters, clams, or mussels. On August 19, CDHS issued a warning about eating raw oysters, clams, and mussels harvested off the coasts of BC and Washington. CDHS interviewed each of the 83 persons reported with culture-confirmed V. parahaemolyticus infections with onset during June 9-December 9. Of the 83, a total of 68 (82%) reported eating oysters during the week before onset of illness. Although 59 persons ate oysters identified through traceback as having been harvested off the coast of Washington and BC, nine persons with culture-confirmed illness ate oysters harvested from Tomales Bay, California (40 miles north of San Francisco). Summary Findings During July 20-August 24, culture-confirmed cases of V. parahaemolyticus infections associated with eating shellfish harvested from Washington or BC also were reported to the state health departments of Utah (three), Alaska (one), Maryland (one), and Hawaii (one). A total of 209 culture-confirmed V. parahaemolyticus infections were reported throughout North America during this outbreak. Dates of illness onset ranged from May 26 through December 9 (median: August 8) (Figure_1). V. parahaemolyticus isolates from ill persons included many different serotypes, some of which matched serotypes found in oysters. The median age of patients was 39 years (range: 12-85 years); 141 (67%) were male. Clinical histories were available for 196 persons with culture-confirmed infection: 194 (99%) reported diarrhea; 172 (88%), abdominal cramps; 101 (52%), nausea; 77 (39%), vomiting; 64 (33%), fever; and 24 (12%), bloody diarrhea. Of 137 persons providing information on underlying illnesses, 17 (12%) reported an underlying illness. Two patients were hospitalized; one with V. parahaemolyticus isolated from her bloodstream died. Mean Pacific coastal sea surface temperatures recorded by the U.S. Navy ranged from 54 F-66 F (12 C-19 C) during May 13-September 9, 1997 (B. McKenzie, U.S. Navy, personal communication, 1998). These temperatures were 2 F-9 F (1 C-5 C) above temperatures from the same period in 1996. Oysters from implicated harvest sites contained V. parahaemolyticus, but the number of organisms per gram was often less than 200 CFU. The highest levels were greater than 11,000 CFU in samples tested by CFIA. Reported by: M Fyfe, MD, Communicable Disease Epidemiology; MT Kelly, MD, Provincial Laboratory, British Columbia Center for Disease Control; ST Yeung, MBBS, Field Epidemiology Training Program, Health Canada; P Daly, MD, Vancouver/Richmond Health Board; K Schallie, Canadian Food Inspection Agency; S Buchanan, Food Protection Programs, British Columbia Ministry of Health. P Waller, MS; J Kobayashi, MD, Communicable Disease Epidemiologist; N Therien, MPH, M Guichard, MS, S Lankford, Public Health Laboratories; P Stehr-Green, DrPH, State Epidemiologist, Washington Dept of Health. R Harsch, MD, Oregon Health Sciences Univ, Portland; E DeBess, DVM, M Cassidy, T McGivern, S Mauvais, D Fleming, MD, State Epidemiologist, State Health Div, Oregon Dept of Human Resources. M Lippmann, Communicable Disease Control Unit; L Pong, Environmental Health Management Section, City and County of San Francisco Dept of Public Health. RW McKay, Food Safety Div, Dept of Agriculture; DE Cannon, Environmental Health, Shellfish Program; SB Werner, MD; S Abbott, Div of Communicable Disease Control; M Hernandez, C Wojee, J Waddell, Div of Food, Drug, and Radiation Safety, S Waterman, MD, State Epidemiologist, California Dept of Health Svcs. J Middaugh, MD, State Epidemiologist, State of Alaska Dept of Health and Social Svcs. D Sasaki, DVM, Epidemiology Br, P Effler, MD, State Epidemiologist, Hawaii Dept of Health. C Groves, MS, N Curtis, Maryland State Epidemiology and Disease Control, D Dwyer, MD, State Epidemiologist, Maryland State Dept of Health and Mental Hygiene. G Dowdle, MSPH, Communicable Disease Control, C Nichols, MPA, State Epidemiologist, Utah Dept of Health. Center for Food Safety and Applied Nutrition, US Food and Drug Administration. Foodborne and Diarrheal Diseases Br, Div of Bacterial and Mycotic Diseases, National Center for Infectious Diseases, CDC. Editorial NoteEditorial Note: The last large outbreak of V. parahaemolyticus infections reported in North America occurred in 1982 and resulted in 10 culture-confirmed cases. Although V. parahaemolyticus outbreaks are rare, sporadic cases are not infrequent. Most infections are associated with ingestion of raw or undercooked shellfish harvested from both the Gulf of Mexico and the Pacific Ocean. V. parahaemolyticus is a gram-negative bacterium that naturally inhabits U.S. and Canadian coastal waters and is found in higher concentrations during the summer (2,3). The outbreak described in this report may have been associated with elevated water temperatures. Because V. parahaemolyticus concentrations in oysters and shellfish increase with warmer temperatures, enhanced surveillance at the beginning of summer may lead to earlier recognition and appropriate public health action. Water temperature monitoring may help determine when oyster beds should be closed to harvesting to prevent further outbreaks (4). Epidemiologic and microbiologic studies conducted during this outbreak primarily implicated eating raw oysters. On the basis of studies suggesting that the infectious dose of V. parahaemolyticus might be greater than or equal to 100,000 CFU (5), the United States and Canada allow the sale of oysters if there are less than 10,000 CFU of V. parahaemolyticus per gram of oyster. However, adherence to these guidelines did not prevent this outbreak. Closure of implicated shellfish beds by health officials was useful; in Canada, additional human illness rapidly declined following a federally mandated suspension of harvesting of shellfish from BC waters in September. In the United States, shellfish-associated infections continued to occur into December. The mean incubation period for V. parahaemolyticus is 15 hours (range: 4-96 hours). In immunocompetent persons, V. parahaemolyticus causes a mild to moderate gastroenteritis with a mean duration of illness of 3 days. Infection can cause serious illness in persons with underlying disease (e.g., persons who use alcohol excessively or have diabetes, pre-existing liver disease, iron overload states, compromised immune systems, or gastrointestinal problems) (2,6). During this outbreak, most ill persons had no underlying illness. To reduce the risk for V. parahaemolyticus and other shellfish-associated infections, persons should avoid eating raw or undercooked shellfish. If persons who eat raw or undercooked shellfish develop gastroenteritis within 4 days of ingestion, they should consult a health-care provider and request a stool culture. Only three states (California, Florida, and Louisiana) require visible posting of alerts regarding the risks associated with eating raw oysters at point of retail sale (2,7,8). Although assessment of these regulatory educational strategies have indicated compliance is variable (7), other states might consider posting such alerts. V. parahaemolyticus is not a reportable disease in all states. During this outbreak, public health officials in Washington and California and in BC promptly became aware of the outbreak through routine reporting; in Oregon, although V. parahaemolyticus is not reportable, the outbreak was detected through an active surveillance program. All states should consider making V. parahaemolyticus and other vibrioses reportable; standard forms are available from CDC's Foodborne and Diarrheal Diseases Branch, Division of Bacterial and Mycotic Diseases, National Center for Infectious Diseases, telephone (404) 639-2206; fax (404) 639-2205. References
Figure_1 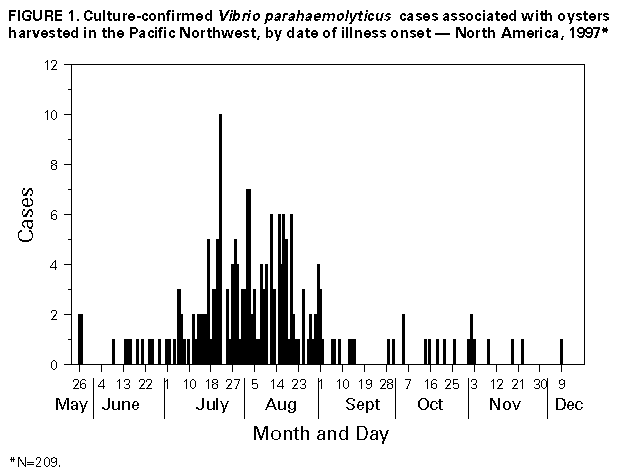 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 10/05/98 |
|||||||||
This page last reviewed 5/2/01
|