 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Heat-Related Deaths -- Dallas, Wichita, and Cooke Counties, Texas, and United States, 1996During July 2-8, 1996, high maximum daily temperatures in Dallas County, Texas, ranged from 101 F (38.3 C) to 106 F (41.1 C), and high maximum daily heat indexes (a measure of the effect of combined elements {e.g., heat and humidity} on the body) ranged from 105 F (40.6 C) to 112 F (44.4 C). Although guidelines for issuing heat advisories or warnings vary by geographic location and climate, the National Weather Service generally suggests issuing a heat advisory when a daytime heat index reaches greater than or equal to 105 F (greater than or equal to 40.6 C), and a night time minimum ambient temperature of 80 F (26.7 C) persists for at least 48 hours. In Dallas County, the criterion used by the medical examiner's (ME's) office to designate a heat wave is greater than or equal to 3 consecutive days of temperatures greater than or equal to 100 F (37.8 C). This report describes four cases of heat-related death in Dallas, Wichita, and Cooke counties, Texas, in 1996; summarizes risk factors for this problem; and reviews measures to prevent heat-related morbidity and mortality. The findings in this report indicate that, although a large proportion of heat-related deaths occur during the summer and during heat waves, such deaths occur year-round. For a death to be attributed to heat-related illness by the Dallas County ME's office (which serves as consultant for both Cooke and Wichita counties), a decedent must meet at least one of the following three criteria: 1) core body temperature is greater than or equal to 105 F (greater than or equal to 40.6 C) at the time of or immediately following death, 2) there is substantial environmental or circumstantial evidence of heat as a contributor to death (e.g., decedent is found in a room with a high ambient temperature, windows closed, and no air conditioning), or 3) decedent is found in a decomposed condition without evidence of other cause of death, and the decedent was last seen alive during the heat-wave period. Case 1. On February 21 (an exceptionally warm winter day {temperature approximately 90 F (32.2 C)}), a 10-month-old girl was left in a car in Dallas County at approximately 9:30 a.m.; she was discovered unresponsive at approximately 2:45 p.m. Despite the initiation of cardiopulmonary resuscitation, she could not be resuscitated. A core body temperature of 108 F (42.2 C) was recorded in the emergency department (ED), and the cause of death was listed as hyperthermia. Case 2. On July 9, a 61-year-old female resident of Cooke County was found dead in her bedroom in a residence with no air conditioning. Although fans were operating in the room, the room temperature was 107 F (41.7 C); air moved by the fan was 104 F (40.0 C). Family members reported having heard the woman moving about at approximately 8 a.m., but she was not checked by family members until approximately noon. The family reported a possible history of diabetes, although this diagnosis could not be confirmed. The primary cause of death was listed as hyperthermia, and the secondary cause was listed as dilated cardiomyopathy. Case 3. On July 10, a 52-year-old man walked from the lawn he was mowing in Dallas County to a nearby residence and knocked on the back door. When the homeowner opened the door, the man collapsed onto the porch. An ambulance transported him to a hospital ED, where he died. On arrival in the ED, his core temperature was 107.1 F (41.7 C), which, before his death, was reduced to 101 F (38.3 C) with ice baths. The outside temperature at the time he collapsed was 109 F (42.8 C). The primary cause of death was listed as hyperthermia, and the secondary cause was listed as hypertensive and arteriosclerotic cardiovascular disease. Case 4. On July 10, an 80-year-old female resident of Wichita County was discovered outdoors at 8 a.m. near shrubs she had been watering the previous day. Although her residence was air conditioned, the high temperature outside the day she died was 102 F (38.9 C). The primary cause of death was listed as hyperthermia. The secondary cause of death was listed as arteriosclerotic cardiovascular disease. Reported by: B Lene, MD, Southwestern Institute of Forensic Sciences at Dallas; Forecast Office, National Weather Svc, Fort Worth, Texas. J Grymes, Southern Regional Climate Center, Louisiana State Univ, Baton Rouge. Health Studies Br, and Surveillance and Programs Br, Div of Environmental Hazards and Health Effects, National Center for Environmental Health, CDC. Editorial NoteEditorial Note: During 1979-1994, the underlying cause of death for 5899 deaths in the United States was heat exposure *; of the 2383 persons for whom age data were available, persons aged greater than or equal to 55 years accounted for 1471 (62%) heat-related deaths "due to weather conditions" (Figure_1). Of the 221 heat-related deaths in 1994, a total of 101 were "due to weather conditions." During 1979-1994, the four highest age-adjusted rates for heat-related deaths "due to weather conditions" occurred in Arizona, Arkansas, Kansas, and Missouri (range: 2.7-3.7 per 1 million population). Because several other causes of death (e.g., cardiovascular and respiratory diseases) also increase during heat waves (1-3), deaths attributed to hyperthermia represent only a portion of heat-related excess mortality. The criteria to determine which deaths are attributable to hot weather and heat-related illness vary by state and among individual MEs and coroners (1,4,5). Consequently, the effects of hot weather on human mortality probably are underestimated, and standard definitions are needed to accurately classify these deaths (1,4,5). The cases described in this report illustrate the spectrum of factors and conditions associated with heat-related mortality, including age (the very young and the elderly), medical history (e.g., cardiovascular disease), social circumstance (e.g., living alone), and physical activity (e.g., exertion in exceptionally hot environments during either work or recreational activities) (2,6). Other factors associated with increased risk include alcohol consumption, chronic conditions (e.g., respiratory diseases), history of previous heatstroke, use of some medications (e.g., phenothiazines, butyrophenones, and thioxanthenes), and physical or mental impairment or bed confinement that interferes with ability to care for oneself (2,4,6). In addition to persons with risk factors, all persons may be at increased risk for fatal heatstroke if sufficiently exposed -- even on exceptionally hot winter days (4). Because young children, the elderly, and the immobile may be unable to obtain and drink adequate fluids or to avoid hot environments, they are at greater risk for heat exhaustion or heatstroke (2). The use of some drugs may increase the risk for heat-related illness by interfering with the body's physical heat regulatory system (2,4); examples of such drugs are neuroleptics (e.g., antipsychotics or major tranquilizers) and medications with anticholinergic effects (e.g., tricyclic antidepressants, antihistamines, some antiparkinsonian agents, and some over-the-counter sleeping pills). Alcohol consumption may cause dehydration, which increases the risk for heat-related illness (2). Adverse health conditions associated with high environmental temperatures include heatstroke, heat exhaustion, heat syncope, and heat cramps (4). Heatstroke is a medical emergency characterized by rapid onset and progression (within minutes) of the core body temperature to greater than or equal to 105 F (greater than or equal to 40.4 C) and lethargy, disorientation, delirium, and coma (4). Heatstroke is often fatal despite expert medical care directed at rapidly lowering the body temperature (e.g., ice baths) (4). Manifestations of heat exhaustion, which is clinically more benign than heatstroke, include dizziness, weakness, or fatigue often following several days of sustained exposure to hot temperatures (4); treatment for heat exhaustion is directed at replacing fluids and electrolytes and may require hospitalization (4). Heat syncope and heat cramps are usually related to physical exertion during hot weather (4). Treatment of persons who lose consciousness as a result of heat syncope should include placement in a recumbent position and electrolyte replacement (4). Persons working in high temperatures -- either indoors or outdoors -- should take special precautions, including allowing 10-14 days to acclimate to an environment of high ambient temperature. Although adequate salt intake is important, salt tablets are not recommended and may even be hazardous for many persons (4). Even though the use of fans may increase comfort at temperatures less than 90 F (less than 32.2 C), fans are not protective against heatstroke in the presence of high temperatures (greater than or equal to 90 F {greater than or equal to 32.2 C}) and humidity (greater than 35%) (2,7). Measures for preventing heat-related illness and death include increasing time in air-conditioned environments, increasing nonalcoholic fluid intake, exercising only during cooler parts of the day, and taking cool-water baths (2). Persons whose fluid consumption is restricted for medical reasons should alter their fluid intake patterns only if advised by their physicians (4). The elderly should be encouraged and assisted in taking advantage of air-conditioned environments (e.g., shopping malls, public libraries, and heat-wave shelters), even if for only part of the day (2,4,6). Parents should be educated about the increased heat sensitivity of children aged less than 5 years (4). Prevention messages about how to avoid heat-related illness should be disseminated to the public as early as possible when exceptionally high temperatures are forecast. These messages can assist in reducing the risk for heat-related deaths, even though such deaths usually do not occur until the second or third day of a heat wave (1,5). References
* International Classification of Diseases, Ninth Revision (ICD-9), code E900.0, "due to weather conditions" (deaths); code E900.1, "of man-made origin" (deaths); or code E900.9, "of unspecified origin" (deaths). These data were obtained from the Compressed Mortality File (CMF) of CDC's National Center for Health Statistics, which contains information from death certificates filed in the 50 states and the District of Columbia that have been prepared in accordance with external cause codes. CDC's Wide-ranging ONline Data for Epidemiologic Research computerized information system was used to access CMF data. All rates were standardized to the 1980 U.S. population. Figure_1 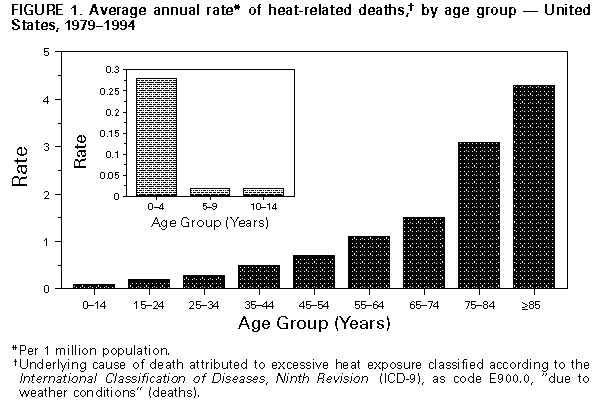 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 09/19/98 |
|||||||||
This page last reviewed 5/2/01
|