 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Progress Toward Elimination of Haemophilus influenzae Type b Disease Among Infants and Children -- United States, 1987-1995Before effective vaccines were available, Haemophilus influenzae type b (Hib) was the most common cause of bacterial meningitis among children in the United States, and an estimated one of 200 children aged less than 5 years developed invasive Hib disease (1-4). From December 1987 -- when Hib conjugate vaccines were introduced -- through 1994, the incidence of invasive Hib disease declined 95% among children aged less than 5 years (4,5). Eliminating invasive Hib disease among children aged less than 5 years by 1996 is a goal of the Childhood Immunization Initiative (CII) (6). This report summarizes data about trends in invasive H. influenzae (Hi) disease during 1987-1995 from three separate surveillance systems (CDC's National Notifiable Diseases Surveillance System [NNDSS]; the National Bacterial Meningitis and Bacteremia Reporting System [NBMBRS]; and an active, multistate, laboratory-based surveillance system). The findings underscore the need for age-appropriate vaccination of infants and for complete investigation and reporting of cases of invasive Hi disease (2). National Surveillance State health agencies report weekly provisional notifiable diseases data to NNDSS through the National Electronic Telecommunications System for Surveillance (NETSS) (7,8). Because the primary purpose of NNDSS is timely national surveillance, the information transmitted includes only basic demographic data about persons with invasive Hi disease. NETSS permits electronic transmission of critical supplemental information (e.g., the type of clinical illness, serotype causing disease, Hib vaccination status, and clinical outcome) for cases of Hi disease; these data were reported consistently by approximately 25 states. NBMBRS collects information about invasive bacterial diseases in the United States and includes detailed information about each case identical to the supplemental information transmitted through NETSS. Approximately 11 states participated consistently in reporting through NBMBRS. During June-July 1996, all states were contacted to obtain additional supplemental information about Hi disease among children aged less than 5 years who had onset of disease in 1995. Three states confirmed that no Hi cases had been reported in children aged less than 5 years while the remaining 47 states, the District of Columbia, and New York City submitted additional supplemental data. During 1987-1995, the incidence of invasive Hi disease among children aged less than 5 years declined 96% (from 41 cases per 100,000 children to 1.6) (Figure_1) (5). However, the incidence of Hi disease among persons aged greater than or equal to 5 years remained stable during this period. Of the 317 cases of invasive Hi disease among children aged less than 5 years reported in 1995, serotype data were available for 201 (63%) cases. In 1995, Hib accounted for 86 (43%) isolates for which serotype was known; of these, 47 (55%) cases occurred among non-Hispanic whites, 13 (15%) among non-Hispanic blacks, five (6%) among American Indians/Alaskan Natives, two (2%) among Asians/Pacific Islanders, and 12 (14%) among Hispanics; race/ethnicity data were missing for seven (8%). Of the 74 (86%) Hib case-patients identified in 1995 for whom information about age and vaccination status were available, 33 (45%) were unvaccinated and 41 (55%) had received at least one Hib-containing vaccine; all but three children had their first vaccination at age less than 7 months (Table_1). Twenty-two children were age-appropriately vaccinated before disease onset, including three children who began the series late. Among 18 children who had completed a primary series before onset of Hib disease, each had completed the two- or three-dose series with one of the three licensed vaccines (i.e., vaccines had not been used interchangeably). Vaccine manufacturer lot numbers were available for 12 of the 18 children; among these children, no single lot was used to complete the series. Laboratory-Based Surveillance The active laboratory-based system coordinated by CDC includes surveillance projects which, during 1989-1994, maintained continuous surveillance of 10.5 million persons in four areas (three counties in the San Francisco Bay area, eight counties in metropolitan Atlanta, four counties in Tennessee, and the state of Oklahoma) (5). During 1995, the population under surveillance was 12.8 million persons in four areas (three counties in the San Francisco Bay area, eight counties in metropolitan Atlanta, five counties in Tennessee, and the state of Maryland). Information routinely obtained about all cases of invasive Hi disease included serotype, clinical syndrome and outcome, vaccination status, and demographic information. Because blacks were overrepresented in the surveillance population, rates were race-adjusted to the 1990 U.S. population. During 1989-1995, the race-adjusted incidence of invasive Hib disease among children aged less than 5 years decreased substantially compared with the decrease in incidence of non-type b Hi disease among children (Figure_2). Among children aged less than 5 years, during 1989-1995 the incidence of invasive Hib cases declined 99% (from 34 cases per 100,000 in 1989 to 0.4 cases in 1995). During 1995, Hib accounted for 18% of all the Hi isolates serotyped from children aged less than 5 years. Information about vaccination status was available for one of the four children aged less than 5 years with invasive Hib disease. This infant had received one dose of vaccine, although he was aged 4.5 months at disease onset and was eligible to have received two doses. One child was too young to be vaccinated, and the other two children for whom vaccination information was not available were aged 6 and 9 months. Reported by: G Rothrock, MPH, Bur of Disease Control, Oakland, California. L Billmann, MPH, L Harrison, MD, Johns Hopkins Univ, Baltimore; D Dwyer, MD, Maryland Dept of Health and Mental Hygiene. B Barnes, MS, Dept of Preventive Medicine, Vanderbilt Medical Center, Nashville, Tennessee. W Baughman, MSPH, Veterans Administration Medical Svcs, Atlanta. Child Vaccine Preventable Disease Br, Epidemiology and Surveillance Div, National Immunization Program; Childhood and Respiratory Diseases Br, Div of Bacterial and Mycotic Diseases, National Center for Infectious Diseases, CDC. Editorial NoteEditorial Note: The findings in this report document the continued decline in the incidence of invasive Hib disease among children aged less than 5 years in the United States -- a trend associated with the increased use of Hib conjugate vaccines. These findings also affirm two of the primary barriers to eliminating invasive Hib disease among children: disease among undervaccinated children and among children too young to complete the primary series of Hib vaccination. Identification of the serotype of cases of invasive Hi disease is essential for evaluating changes in the epidemiology of Hib disease. In the United States, the percentage of invasive Hi disease cases among children with serotype information has increased substantially, from 41% of 340 cases in 1994 to 63% of 317 cases in 1995 (5). These data suggest that the proportion of Hi cases caused by Hib has been decreasing. Invasive Hib disease now occurs primarily among undervaccinated children and among infants too young to have completed the primary series of vaccinations. However, among children aged 19-35 months, Hib vaccination coverage with three or more doses of Hib vaccine increased substantially from the second quarter of 1994 (76%) to the second quarter of 1995 (92%) (9). Although widespread vaccination with conjugate vaccine has reduced Hib colonization rates among young children, circulation of the organism continues (1,4). Population groups with low levels of vaccination probably contribute to the ongoing occurrence of disease and regional differences in disease incidence. Consequently, all health-care providers who counsel parents about childhood vaccination should emphasize the importance of protecting infants against Hib disease and ensure that the vaccine is administered in a timely manner, especially to children of low socioeconomic status who may be more likely to be under-vaccinated or unvaccinated (2,10). The small proportion of Hib cases reported through national surveillance among children who had completed a primary Hib vaccine series with vaccines from different manufacturers and with different lot numbers suggests that vaccine failure occurs infrequently. The findings in this report indicate that the incidence of invasive Hib disease among preschool-aged children has continued to decline, consistent with the goal to eliminate invasive Hib disease among children aged less than 5 years. However, to attain this goal, timely and complete vaccination coverage is needed among all preschool-aged children (2). Because conjugate vaccines reduce Hib carriage and interrupt transmission of the organism, complete coverage among preschool-aged children will help to eliminate disease among infants who are too young to be completely vaccinated (1,2,4). To monitor progress toward meeting the goal of elimination of invasive Hib disease among children aged less than 5 years and to evaluate changes in the epidemiology of invasive Hi disease, national surveillance for Hi should be strengthened. To optimize surveillance efforts, case reporting should include four elements. First, because Hib vaccines protect against Hi serotype b organisms only, serotyping should be performed for all cases of invasive Hi disease -- state health departments are encouraged to identify laboratories in which serotyping is conducted for all Hi isolates or to send Hi isolates to CDC for serotyping. In addition, assessments of children in older age groups (5-14 years) will be needed to document persistence of protection by Hib conjugate vaccines. Second, to improve characterization of groups at risk for under-vaccination and Hib disease, vaccination status of all children with invasive Hib disease should be assessed. Third, to ensure continued high levels of vaccine effectiveness and to enable systematic evaluation of factors associated with vaccine failure in persons with Hib disease, the date, vaccine manufacturer, and vaccine lot number should be included in the case report. Fourth, important indicators of the severity of Hi infections should be reported, including the type of clinical syndrome, specimen source (e.g., cerebrospinal fluid, blood, or joint fluid), and clinical outcome. References
Figure_1 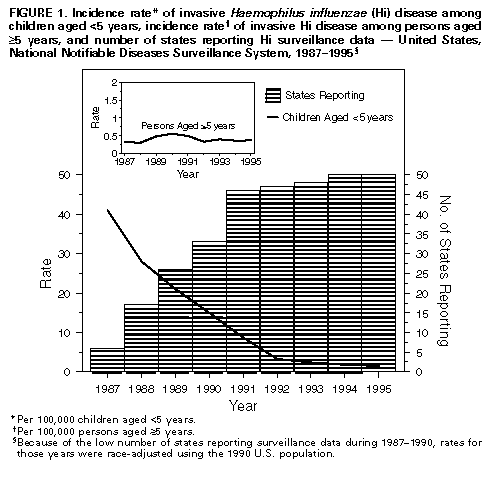 Return to top. Table_1 Note: To print large tables and graphs users may have to change their printer settings to landscape and use a small font size. TABLE 1. Number of children aged <5 years with invasive Haemophilus influenzae type b (Hib) disease, by age group and number of Hib vaccine doses received United States, 1995 *="======================================================================" No. vaccine doses Age group Vaccination (mos.) 0 1 2 3 4 status unknown Total 0- 1 7 2 9 2- 3 9 5 3 17 4- 5 6 9 2 2 19 6-11 8 3 3 4 3 21 12-60 3 2 1 7 5 2 20 Total 33 19 6 11 5 12 86 * Reported through the National Notifiable Diseases Surveillance System, the National Bacterial Meningitis and Bacteremia Reporting System, and states reporting additional supplementary information.="======================================================================" Return to top. Figure_2 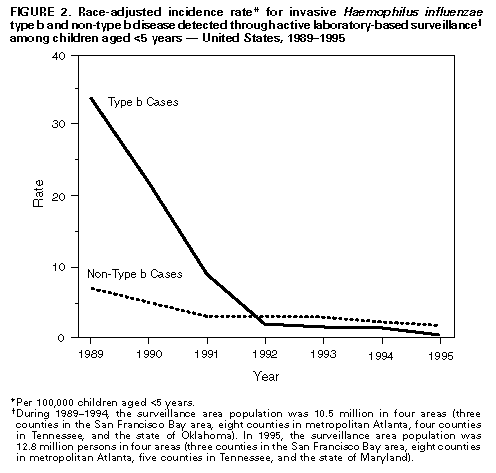 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 09/19/98 |
|||||||||
This page last reviewed 5/2/01
|