 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Pneumococcal and Influenza Vaccination Levels Among Adults Aged Greater Than or Equal to 65 Years -- United States, 1993In 1993, pneumonia and influenza ranked sixth among the 10 leading causes of death in the United States, and approximately 90% of the deaths caused by these illnesses occurred among adults aged greater than or equal to 65 years. A national health objective for the year 2000 is to increase pneumococcal and influenza vaccination levels to greater than or equal to 60% for persons at high risk for complications from pneumococcal disease and influenza, including those aged greater than or equal to 65 years (objective 20.11) (1). To estimate state-specific influenza and pneumococcal vaccination levels for persons aged greater than or equal to 65 years, CDC analyzed data from the 1993 Behavioral Risk Factor Surveillance System (BRFSS). This report summarizes the BRFSS findings, which indicate substantial increases in coverage levels for influenza and pneumococcal vaccines among persons aged greater than or equal to 65 years, and assesses progress toward the year 2000 objective. BRFSS is a population-based, random-digit-dialed telephone survey of the noninstitutionalized U.S. population aged greater than or equal to 18 years and can be used to determine the prevalence of behaviors and practices related to the leading causes of death (2). To assess state-specific vaccination levels, two questions about influenza and pneumococcal vaccination were added to the 1993 BRFSS; 49 states and the District of Columbia participated. Race/ethnicity-specific data are presented only for blacks, whites, and Hispanics because numbers for other racial/ethnic groups were too small for meaningful analysis. Data were weighted by age and sex to reflect each state's most recent adult population estimate and by the probability of the respondent's selection. SUDAAN was used to calculate 95% confidence intervals (CIs). In 1993, weighted responses were available from 19,761 adults aged greater than or equal to 65 years (12,862 {65.1%} and 6899 {34.9%} men) who were interviewed throughout the year as part of state BRFSS surveys. Respondents were asked, "During the past 12 months, have you had a flu shot?" and "Have you ever had a pneumonia vaccination?" A total of 50.4% of respondents reported receiving influenza vaccine during the preceding 12 months, and 28.7% reported ever having received pneumococcal vaccine (Table_1). Self-reported vaccination levels varied by race/ethnicity and state for both influenza and pneumococcal vaccines. Reported vaccination levels were low but similar among men and women (Table_1). Coverage levels varied by race/ethnicity. Non-Hispanic white respondents were significantly more likely to report receiving influenza vaccine during the preceding 12 months (52.2%) than were non-Hispanic black respondents (33.1%) and respondents of other racial/ethnic groups (39.7%). Non-Hispanic whites also were more likely to report ever receiving pneumococcal vaccine (29.8%) than either Hispanics (21.0%) or persons of other racial/ethnic groups (18.7%) (Table_1). State-specific rates for self-reported influenza vaccination ranged from 28.7% (District of Columbia) to 66.2% (Arizona) (median: 49.9%); rates for pneumococcal vaccination ranged from 18.5% (Louisiana) to 40.0% (Colorado) (median: 27.4%) (Table_2). For reported influenza vaccination, coverage levels were greater than or equal to 60% in five states and greater than or equal to 50% in 24 states. Reported by the following BRFSS coordinators: J Durham, MPA, Alabama; P Owen, Alaska; B Bender, Arizona; J Senner, PhD, Arkansas; B Davis, PhD, California; M Leff, MSPH, Colorado; M Adams, MPH, Connecticut; F Breukelman, Delaware; C Mitchell, District of Columbia; D McTague, MS, Florida; E Pledger, MPA, Georgia; J Cooper, MA, Hawaii; C Johnson, MPH, Idaho; B Steiner, MS, Illinois; N Costello, MPA, Indiana; P Busick, Iowa; M Perry, Kansas; K Asher, Kentucky; R Meriwether, MD, Louisiana; D Maines, Maine; A Weinstein, MA, Maryland; D Brooks, MPH, Massachusetts; H McGee, MPH, Michigan; N Salem, PhD, Minnesota; S Loyd, Mississippi; J Jackson-Thompson, PhD, Missouri; P Smith, Montana; S Huffman, Nebraska; E DeJan, MPH, Nevada; K Zaso, MPH, New Hampshire; G Boeselager, MS, New Jersey; W Honey, New Mexico; T Melnik, DrPH, New York; G Lengerich, VMD, North Carolina; J Kaske, MPH, North Dakota; R Indian, MS, Ohio; N Hann, MPH, Oklahoma; J Grant-Worley, MS, Oregon; L Mann, Pennsylvania; J Hesser, PhD, Rhode Island; J Ferguson, DrPh, South Carolina; M Gildemaster, South Dakota; D Ridings, Tennessee; R Diamond, MPH, Texas; R Giles, Utah; R McIntyre, PhD, Vermont; J Stones, Virginia; K Wynkoop-Simmons, PhD, Washington; F King, West Virginia; E Cautley, MS, Wisconsin. Adult Vaccine Preventable Diseases Br, Epidemiology and Surveillance Div, and Assessment Br, Data Management Div, National Immunization Program; Behavioral Surveillance Br, Div of Adult and Community Health, National Center for Chronic Disease Prevention and Health Promotion, CDC. Editorial NoteEditorial Note: During 1972-1991, influenza caused an estimated 20,000 excess deaths during each of 10 U.S. epidemics (3). Pneumococcal infections are the most common cause of bacterial pneumonia requiring hospitalization and cause an estimated 40,000 deaths annually in the United States (4). Despite the continuing morbidity and mortality caused by influenza and pneumococcal disease among adults, coverage levels remained low during 1973-1993 for influenza vaccine and during 1984-1993 for pneumococcal vaccine (5) (Figure_1). However, the findings in this report indicate that, in 1993, state-specific self-reported coverage levels for both influenza and pneumococcal vaccines were at the highest levels ever reported for persons aged greater than or equal to 65 years. Previous estimates indicate that self-reported influenza and pneumococcal vaccination levels among persons aged greater than or equal to 65 years increased steadily during 1987-1993 (3,6) (Figure_1). In addition, preliminary estimates from the 1994 National Health Interview Survey indicate overall influenza and pneumococcal vaccination levels for persons aged greater than or equal to 65 years were 55% and 30%, respectively (CDC, unpublished data, 1996). Possible reasons for the increase in self-reported influenza vaccination levels include 1) greater acceptance of preventive medical services by practitioners, 2) increased delivery and administration of vaccine by health-care providers and sources other than physicians (e.g., visiting nurse and home-health agencies), and 3) the initiation of Medicare reimbursement for influenza vaccination in 1993 (5). In conjunction with the increase in coverage levels for influenza vaccine, net doses of influenza vaccine distributed nationwide also increased, from 24 million doses of vaccine distributed in 1989 to 40.9 million doses in 1993 (Figure_2). Although pneumococcal vaccination levels increased during 1989-1993, self-reported coverage levels in 1993 were substantially lower than those for influenza vaccine. Distribution of pneumococcal vaccine increased from 1.2 million doses in 1989 to 3.6 million doses in 1993, consistent with increasing self-reported vaccination levels (Figure_2). Coverage may be lower because many providers and patients are not routinely reminded about the need for pneumococcal vaccination among persons aged greater than or equal to 65 years; in comparison, influenza vaccination campaigns are conducted annually before each influenza season. Intensified efforts are needed to improve knowledge among health-care providers and the public about the benefits of pneumococcal vaccination and current recommendations for this vaccine (e.g., simultaneous administration of influenza and pneumococcal vaccines for those who require both vaccines). Lower levels for influenza vaccination coverage among non-Hispanic blacks and pneumococcal vaccination coverage among Hispanics have been previously reported (5). Compared with vaccination levels for non-Hispanic whites, these racial/ethnic variations may reflect differences in multiple factors, including education, income, insurance coverage, culture and behavior, and the prevalence of specific risk factors (7,8), and emphasize the need for programs aimed at increasing vaccination levels among these groups. The 1993 BRFSS documents substantial state-specific variation in influenza and pneumococcal vaccination levels. Some of these differences probably are related to racial/ethnic variations in population density and vaccination levels. In addition, medical practice patterns vary regionally because of differences in health-reimbursement plans, physician practice patterns, and patient attitudes toward different aspects of medical care (9). These variations probably are determinants for administration of influenza and pneumococcal vaccines. The findings in this report are subject to at least two limitations. First, because BRFSS data were self-reported without validation of vaccination status, these findings may underestimate vaccination levels; however, a validation study among a different sample indicated 91% of persons who had reported receiving influenza vaccine actually received the vaccine (10). Second, some medical conditions increase the risk for complications or death from influenza and pneumococcal disease, and providers may be more likely to administer vaccine to patients with these conditions; however, BRFSS did not collect data about medical conditions of respondents. To achieve the year 2000 objective for influenza and pneumococcal vaccination levels, additional efforts should be directed toward high-risk populations, including all persons aged greater than or equal to 65 years. Measures for increasing coverage require 1) continuing collaboration between public and private organizations to improve awareness about the need for these vaccines; 2) changes in clinical practice to improve vaccine delivery; 3) vaccine delivery mechanisms that limit cost and remove accessibility constraints; and 4) timely surveillance data, such as those collected by BRFSS, to assess the progress of current and future programs. States can expand influenza and pneumococcal vaccination services for the elderly by building coalitions with private, medical, and community groups; collaborating with Health Care Financing Administration Peer Review Organizations to increase vaccination levels among Medicare beneficiaries; and encouraging local health departments to enroll as Medicare providers and to file claims for influenza and pneumococcal vaccination services, which are covered benefits under Medicare. BRFSS and other state-specific data can assist states in targeting expanded vaccination programs for the elderly. References
Table_1 Note: To print large tables and graphs users may have to change their printer settings to landscape and use a small font size.
TABLE 1. Percentage of persons aged >= 65 years who reported receiving influenza * or
pneumococcal + vaccine, by sex and race/ethnicity & -- United States, Behavioral Risk
Factor Surveillance System (BRFSS), 1993
=============================================================================================
Influenza Pneumococcal
-------------------- --------------------
Characteristic % (95% CI **) % (95% CI)
-------------------------------------------------------------------
Sex
Men 48.8 (47.1%-50.5%) 28.2 (26.7%-29.7%)
Women 51.5 (50.2%-52.8%) 29.1 (27.9%-30.3%)
Race/Ethnicity
White, non-Hispanic 52.2 (51.1%-53.3%) 29.8 (28.8%-30.8%)
Black, non-Hispanic 33.1 (29.5%-36.7%) 25.0 (19.3%-30.7%)
Hispanic 47.6 (40.9%-54.3%) 21.0 (14.5%-27.5%)
Other 39.7 (30.8%-48.5%) 18.7 (15.6%-21.8%)
Total 50.4 (49.3%-51.5%) 28.7 (27.7%-29.7%)
-------------------------------------------------------------------
* During the preceding 12 months.
+ Ever during their lifetimes.
& Numbers for racial/ethnic groups other than blacks, whites, and Hispanics were too small
for meaningful analysis.
@ Forty-nine states and the District of Columbia participated in the 1993 BRFSS. Weighted
sample size=19,761: 12,862 (65.1%) women and 6899 (34.9%) men.
** Confidence interval.
=============================================================================================
Return to top. Table_2 Note: To print large tables and graphs users may have to change their printer settings to landscape and use a small font size.
TABLE 2. Number of persons aged >= 65 years who reported receiving influenza * or
pneumococcal + vaccine and percentage vaccination coverage, by state -- United
States, Behavioral Risk Factor Surveillance System (BRFSS), 1993&
==================================================================================================
Influenza Pneumococcal
No. -------------------- --------------------
State persons % (95% CI @) % (95% CI)
------------------------------------------------------------------------------
Alabama 490 40.0 (35.4%-44.7%) 25.1 (20.9%-29.2%)
Alaska 141 53.3 (42.2%-64.5%) 31.2 (21.2%-41.2%)
Arizona 384 66.2 (59.8%-72.7%) 30.7 (24.7%-36.7%)
Arkansas 427 51.8 (46.3%-57.3%) 27.2 (22.6%-31.7%)
California 630 54.4 (50.0%-58.8%) 35.6 (31.4%-39.9%)
Colorado 268 64.0 (57.5%-70.4%) 40.0 (33.4%-46.6%)
Connecticut 345 53.4 (47.6%-59.1%) 18.8 (14.5%-23.1%)
Delaware 395 55.0 (49.6%-60.3%) 35.6 (30.6%-40.7%)
District of Columbia 225 28.7 (21.8%-35.7%) 22.2 (14.9%-29.4%)
Florida 788 46.3 (42.6%-50.1%) 25.2 (21.9%-28.5%)
Georgia 391 44.4 (38.8%-50.0%) 27.8 (23.0%-32.6%)
Hawaii 299 56.6 (49.2%-64.0%) 37.8 (31.1%-44.6%)
Idaho 355 64.4 (58.5%-70.3%) 33.1 (27.3%-38.9%)
Illinois 470 45.2 (40.0%-50.4%) 23.1 (18.8%-27.4%)
Indiana 438 47.0 (41.9%-52.2%) 26.7 (22.2%-31.2%)
Iowa 430 49.7 (44.6%-54.8%) 32.3 (27.6%-37.0%)
Kansas 258 52.4 (45.9%-59.0%) 23.1 (17.8%-28.5%)
Kentucky 581 44.5 (40.1%-48.9%) 24.2 (20.3%-28.1%)
Louisiana 318 36.2 (30.3%-42.1%) 18.5 (13.8%-23.2%)
Maine 287 49.2 (42.9%-55.6%) 20.3 (15.2%-25.4%)
Maryland 749 48.6 (44.6%-52.7%) 33.8 (30.0%-37.5%)
Massachusetts 289 49.7 (43.5%-56.0%) 21.5 (16.4%-26.6%)
Michigan 401 47.8 (42.4%-53.2%) 24.7 (20.2%-29.1%)
Minnesota 660 50.9 (46.9%-54.9%) 26.1 (22.6%-29.7%)
Mississippi 302 42.4 (35.9%-48.9%) 27.6 (22.0%-33.2%)
Missouri 337 54.8 (48.9%-60.6%) 30.6 (25.0%-36.2%)
Montana 244 62.4 (55.8%-69.0%) 33.8 (27.1%-40.4%)
Nebraska 426 53.2 (48.1%-58.3%) 27.4 (22.9%-31.9%)
Nevada 278 43.6 (37.0%-50.1%) 31.4 (24.9%-37.8%)
New Hampshire 256 49.6 (42.8%-56.3%) 19.1 (13.9%-24.4%)
New Jersey 265 53.2 (46.6%-59.9%) 21.9 (16.5%-27.3%)
New Mexico 226 60.9 (54.0%-67.8%) 31.8 (25.6%-38.0%)
New York 438 45.3 (40.1%-50.5%) 22.1 (18.0%-26.2%)
North Carolina 443 50.9 (45.9%-55.9%) 26.3 (21.7%-30.9%)
North Dakota 423 48.9 (43.9%-53.9%) 19.8 (15.8%-23.8%)
Ohio 324 50.1 (44.0%-56.2%) 27.9 (22.4%-33.4%)
Oklahoma 355 58.4 (52.7%-64.1%) 29.1 (24.4%-33.8%)
Oregon 593 55.8 (51.4%-60.2%) 34.7 (30.3%-39.1%)
Pennsylvania 544 48.7 (44.1%-53.2%) 25.0 (21.2%-28.8%)
Rhode Island 356 51.2 (45.4%-57.0%) 20.1 (15.8%-24.5%)
South Carolina 400 47.3 (41.6%-53.0%) 19.4 (14.9%-23.9%)
South Dakota 401 47.7 (42.6%-52.8%) 26.6 (22.1%-31.1%)
Tennessee 578 46.0 (41.6%-50.4%) 25.5 (21.6%-29.3%)
Texas 376 56.8 (50.9%-62.6%) 36.9 (31.4%-42.4%)
Utah 284 54.3 (47.7%-60.9%) 35.3 (28.7%-41.9%)
Vermont 318 57.0 (51.2%-62.9%) 28.7 (23.4%-34.0%)
Virginia 287 45.8 (39.2%-52.3%) 34.2 (28.0%-40.4%)
Washington 394 53.4 (48.1%-58.6%) 32.1 (27.2%-37.0%)
West Virginia 592 49.8 (45.3%-54.2%) 28.5 (24.5%-32.5%)
Wisconsin 302 49.1 (42.8%-55.3%) 27.4 (21.7%-33.1%)
Range 141-788 28.7-66.2 18.5-40.0
Median 49.9 27.4
------------------------------------------------------------------------------
* During the preceding 12 months.
+ Ever during their lifetimes.
& Forty-nine states and the District of Columbia participated in the 1993 BRFSS. Weighted sample
size=19,761:12,862 (65.1%) women and 6899 (34.9%) men.
@ Confidence interval.
==================================================================================================
Return to top. Figure_1  Return to top. Figure_2 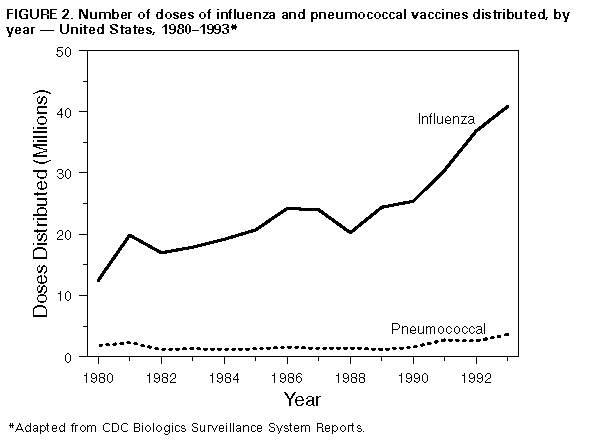 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 09/19/98 |
|||||||||
This page last reviewed 5/2/01
|