 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Appendix Instructions for Completing the Sudden Unexplained Infant Death Investigation Report Form (SUIDIRF)Use SUIDIRF may be used to assess the death of any infant for whom the cause of death is not apparent before autopsy. Applicable parts of the form may also be used to collect data about the death of any infant for whom the cause of death is known. The medical examiner or coroner (ME/C) or the death investigator acting on behalf of the former should complete the SUIDIRF. Police officers who report to the ME/C may also find the form useful. Completion The form may be completed by using blue or black ink or a #2 soft-lead pencil to facilitate electronic scanning, photocopying, and fax transmission. To ensure legibility of the forms, writing on the blank side (back) of the forms is discouraged. One blank page is provided for notes. If necessary, additional sheets of blank paper may be attached. Design The SUIDIRF pages are designed for use on a clipboard. The pages may be separated to allow other persons to complete, scan, photocopy, or fax the pages. Each page is printed on one side for legibility. Compatibility with Other Forms CDC's Medical Examiner and Coroner Information Sharing Program has published two generic death investigation report forms (DIRFs) -- one for the investigator conducting the initial phases of the investigation (IDIRF) and another for the person who certifies the death or "closes" the investigation (CDIRF) (1,2). The SUIDIRF is compatible with the DIRFs and has many data items in common. The CDIRF may be used in conjunction with the SUIDIRF. Although the generic IDIRF can be used for all death investigations irrespective of the age of the decedent, the SUIDIRF was designed specifically for infant deaths. On the SUIDIRF, the one-letter abbreviations in parentheses match the codes on the other DIRFs developed by CDC. General Instructions Glossay Table_G1 Use military time. Military time (midnight = 0000, noon = 1200) facilitates computer applications. Midnight (0000) corresponds to the same day as 0001 (one minute after midnight). The investigator may indicate a.m. and p.m. as long as the data entry personnel converts standard time to military time. Month and day are sufficient for many fields. Birth date, death date, and the date the case was reported to the ME/C should each contain the month, day, and year, in that order, in numeric format (e.g., 01/05/97). For other events that occur in the same year as the report, indicating the month and day only is sufficient. Indicate answers by an X. Multiple possible answers to an item are preceded by a line or followed by a box. Indicate the correct answer by writing an X on the appropriate line or in the appropriate box. Use NA to indicate that a specific item is not applicable. If a given item is not applicable, write NA. If the respondent refuses to answer a question, write refused. Do not leave an item blank; the reviewer needs to know that an item has not been overlooked. Correct errors by erasing or scratching through an incorrect response. If it is not possible to erase an answer, scratch out the incorrect response and indicate the correct one by using an X or by writing text as needed. Page-by-Page Instructions Many of the information items on SUIDIRF are self-explanatory. Instructions are provided here for items that require clarification. Page 1 Use page 1 to document the date and time of critical events as well as to describe briefly circumstances of the infant's death. If the space on the blank page provided is not sufficient, additional pages for narrative descriptions may be attached. Home address. The primary residence of the infant at the time of his or her death. Age. The infant's age at death. Use MI for minutes (if less than 1 hour old), HR for hours (if less than 1 day old), DA for days (if less than 1 month old), and MO for months (until 23 months). Age at death can readily be calculated from the date of birth and date of death. Race. The infant's race (based on the race of the birth mother). Use W for white, B for black, I for American Indian or Alaskan Native, A for Asian or Pacific Islander, and O for other. Ethnicity. Whether the infant is of Hispanic descent. Additional information about the infant's national descent may be included here (e.g., Japan, China, Philippines, South Africa, Poland, or Germany). Receipt by. The name of the ME/C or receptionist who first received notification of the infant's death. NOK notified. The date and time the NOK not at the scene was notified of the infant's death, who was notified, and by whom. If the family was present at the scene and already knew of the infant's death at the time of its report, write NA in the date field. Scene visit. The date and time the ME/C or the death investigator acting on behalf of the former visited the site where the injury or illness began or the death occurred. If ME/C staff visited the site, put an X by "ME/C staff" and name the person who went to the scene. If another agency and not ME/C staff went to the site, put an X by "Other agency" and name the agency or person. If no scene visit took place, place an X by "Not done"; however, use this form to collect information from telephone or in-person interviews of witnesses and from emergency medical service logs and reports. Scene address. The address of the place where the injury or death occurred. Indicate if the scene address is the same as the home address. If the scene was not visited, give the presumed address. Condition of infant when found. The condition of the infant at the time of his or her discovery. A dead infant is believed to be dead even after resuscitation is attempted. An unresponsive infant is unconscious but shows signs of life (e.g., has a pulse and is breathing). An infant in distress is in obvious trouble but retains some degree of responsiveness. Sequence of events before death. A summary of the reported sequence of events leading to the infant's death. For example, "Infant found dead in crib at 3:00 a.m. No significant history." Use supplementary pages to detail the reported circumstances and sequence of events. Injury. The date, time, and address of a known or suspected injury relevant to the infant's death. Discovery. The date, time, and address of where the infant was found dead, unresponsive, or in distress. Arrival. The date and time the infant arrived at a hospital (if such is the case). Transport by. The mode of transport (e.g., ambulance or private motor vehicle) and the agency or person who transported the infant to the hospital. Actual death. The specific date, time, and place where the death is believed or known to have occurred, not necessarily when or where death was pronounced. Options include where the infant was found (on scene), en route to a hospital, in a hospital emergency room, during surgery, and after being admitted to a hospital as an inpatient. Infant placed. The date, time, and type of place where the infant was last placed as well as who placed the infant before he or she was found dead, unresponsive, or in distress. For example, a place might be listed as crib in bedroom, adult bed, sofa in living room, mattress on floor, or infant seat in vehicle. Known alive. The date, time, and type of place where the infant was last seen or otherwise known (or assumed) to be alive as well as who believed the infant was alive. First response. The date, time, and type of response (e.g., mouth-to- mouth resuscitation, chest compression, slapping, or shaking) rendered by the first person who attempted to aid or revive the infant as well as who rendered such aid. EMS called. The date and time EMS was called, who called EMS, and the site from where the EMS caller called. EMS response. The date and time EMS personnel arrived at the scene as well as the name of the EMS agency. Police response. The date and time police arrived at the scene as well as the name of the police department. Place of fatal event. For each choice, only one condition can apply. Indicate the correct choice with an X on the appropriate line. Describe type of place. A concise but thorough description of the place where the events leading to death occurred. Examples include infant's bedroom at home, privately owned day care center, child restraint in back seat of moving car, and infant seat in booth at a restaurant. The name and relationship to the infant of all involved persons referenced on page 1 should be listed in the table at the top of page 4. On page 1 of the form, generic terms (e.g., mother, sister, uncle, or neighbor) can be used to indicate "By whom." Page 2 Use page 2 to document the infant's usual health-care provider, prenatal and birth history, medical history (e.g., recent symptoms, signs, and behavioral changes), and medication history as well as resuscitation attempts (including medical techniques and procedures) used in attempts to revive the infant. The letter codes can be used to identify the fields on supplementary pages and to facilitate data coding. Medical source. The sources used to obtain medical information about the infant and the mother. Use the section on specific infant medical history to describe relevant medical history. If further description or clarification is needed, use the space provided on the right of the form, use the blank supplement page, or attach additional pages. Problems during labor or delivery. Includes problems with the placenta, membranes, or cord; breech or malpresentation; cephalopelvic disproportion; prolonged labor; and fetal distress. Maternal illness or complications during pregnancy. Includes eclampsia; incompetent cervix; maternal anemia; and pregnancy-induced hypertension, diabetes, cardiac conditions, and renal diseases. Major birth defects. Includes central nervous system defects (e.g., spina bifida or meningocele, hydrocephalus, and microcephalus), cardiac malformations, gastrointestinal defects (e.g., rectal atresia or stenosis), Down's syndrome, and cleft lip or cleft palate. Hospitalization of infant after initial discharge. Any overnight stay of the infant at a hospital after having been discharged from the hospital of delivery. Specify the date, reason, and outcome of each hospitalization. Emergency room visits in past 2 weeks. The date, reason, and outcome of each visit. Known allergies. Any allergies (e.g., to cow's milk, food, medication, or vaccine). Growth and weight gain considered normal. If not normal, clarify. Exposure to contagious diseases in past 2 weeks. Any contact with a person who had a communicable infectious disease (e.g., a cold, hepatitis, measles, pertussis, tuberculosis, or viral or diarrheal disease). Illness in past 2 weeks. Any observed illness the infant experienced in the past 2 weeks. Specify the condition and its outcome. Infant has ever stopped breathing or turned blue. Any episode of apnea before the infant died. Infant was ever breast-fed. Breast-feeding was successfully initiated irrespective of whether the infant was still breast-feeding at the time of death. Vaccinations in past 72 hours. Vaccinations against preventable childhood diseases. Specify which vaccinations were administered. Deceased siblings. The cause and circumstances of death of the infant's deceased siblings. Medication history. The type of medications given to the infant in the past. Place an X where it applies. List the name of the medicines and doses taken. Indicate any home remedies given to infant, such as white clay or balms. Emergency medical treatment. The types of medical treatment rendered to revive the infant. Explain further, if necessary, in the spaces provided below. Page 3 When completing the questions on page 3, draw on personal observations. Use the section on household environment to indicate whether the household was visited and to document the presence or absence of selected environmental and social risk factors in the primary home of the infant (even if the events leading to death occurred somewhere else). Items for which the response is yes can be clarified in the space provided on the right. The letter codes can be used to identify the fields on supplementary pages and to facilitate data coding. Also use this section to document maternal sociodemographic information. Type of dwelling. Concise description of the type of household (e.g., single family home, apartment, or trailer). Water source. Source of drinking water (e.g., city water, well water, bottled water, or spring water). Number of bedrooms. The number of rooms used as nighttime sleeping rooms, excluding living and dining rooms. Estimated annual income. The estimated yearly income from all sources except public assistance. On public assistance. Whether the householder receives public assistance (e.g., Aid for Families with Dependent Children {AFDC}). Number of smokers in household. Includes both regular and occasional smokers in the household. Use the section on infant and environment to document the immediate environment in which the events leading to death occurred. The immediate environment may or may not be the infant's primary home. If the infant was found in a crib or bed, put an X in the space provided. Indicate if the infant was sleeping alone or was sharing the crib or bed with others. Temperature of area. A measured temperature where the infant was discovered. If a thermometer is not available, use subjective terms such as cold, cool, comfortable, warm, and hot. The next items are included to help evaluate the possibility of asphyxia and external conditions as a cause of death. The questions evaluate the possibility of interference with breathing (e.g., covering of the nose and mouth) or hazards related to aspiration, choking, electrocution, excessive heat or cold, and other external factors. When possible, the manufacturer, brand, and lot or product number of relevant consumer products should be documented. Sleeping or supporting surface. The characteristics of the crib, bed, floor, or other object that directly supported the infant when he or she was found dead, unresponsive, or in distress. Examples include sheepskin on cement floor, mesh seat of baby swing, sheeted mattress in crib, uncovered mattress on wood floor, and plastic-covered foam cushion on sofa. If the surface is easily compressed or deformed, that fact should be noted and the item should be obtained as evidence. Clothing. A list and description of all articles of clothing worn by the infant, including diapers. Other items in contact with infant. Any objects, other than the sleeping surface and articles of clothing, that were in contact with the infant (e.g., pacifier, dangling puppet on mobile, or plastic- covered, foam-filled bumper guard). These items should be secured as evidence. Items in crib or immediate environment. Any other items in the immediate area to which the infant reasonably may have had access. Examples are pill on floor 16 inches from body, pacifier at opposite end of crib, and electric cord draping through crib. These items should be secured as evidence. Devices operating in room. All electrical and mechanical devices in use in the room where the infant was found dead, unresponsive, or in distress. These devices include vaporizers, space heaters, fans, and infant electronic monitors (e.g., apnea monitor or heart rate monitor). Cooling source in room and Heat source in room. The type of cooling and heat sources in the room where the infant was found. Examples of space devices include portable heaters, window air conditioners, and ceiling fans. Central devices include gas- or electricity-powered systems that heat or cool multiple rooms or an entire house. Use the section on items collected to document material secured as evidence for presentation to the ME/C, crime laboratory, or other expert for further observation or analysis. Page 4 Use page 4 to document interviews and procedures related to the investigation (e.g., review of medical records and referral of the case to a SIDS services agency), provide notes to the pathologist, indicate an overall assessment of whether findings suggest SIDS or another diagnosis or injury, indicate the family's interest in organ or tissue donation, and document disposition of the body. Use the section on interview and procedural tracking to record the names of informants, their relationship to the infant, phone number, and the date and time of interview. Relationship to infant. Specific relationship to the infant (e.g., natural {or birth} mother, adoptive mother, foster mother, stepmother, maternal aunt, or neighbor). Alternate contact person. If the mother cannot be located, the person who would be able to provide information about her. Doll reenactment performed. Whether a doll was used to assist the witnesses in describing the body and face position of the infant when he or she was found dead, unresponsive, or in distress. Detailed protocol completed. Whether the jurisdiction's detailed death investigation protocol was completed. Enter an X by "NA" if no such protocol exists for the jurisdiction. Use the overall preliminary summary to provide notes to the pathologist (e.g., note and evaluate subtle mark on neck), indicate whether environmental hazards or consumer products may have contributed to the infant's death, and indicate whether the family is interested in organ or tissue donation. The last line is for the investigator to indicate whether, in his or her opinion, the investigation suggests SIDS, other causes of death, or trauma or injury. In the section on case disposition, indicate whether the ME/C declined or accepted the reported case for investigation. A case can be declined because the cause and circumstances of death do not place the case within the ME/C's jurisdiction because of the topic (subject matter) or the location of death. A case is generally accepted so that an autopsy can be performed, an external examination can be conducted, and the cause and manner of death can be certified. Diagnosis of SIDS requires a complete autopsy, including histology, toxicology, and other tests as needed. Transport agent. The person or transport service who brings the body to the morgue from its location at the time of the death report. Enter NA if the body is not brought to a morgue. Funeral home. The funeral home authorized to handle the disposition of the body (regardless of whether the body has been brought to a morgue). Page 5 Use page 5 to diagram the immediate area surrounding the infant when he or she was discovered dead, unresponsive, or in distress and to record selected observations about the area. Page 6 Page 6 is an illustration of an infant's body that may be used to note marks, bruises, discolorations, drainage from orifices, and other observations. References
SUDDEN UNEXPLAINED INFANT DEATH INVESTIGATION REPORT FORM (SUIDIRF) 3.96 Figure_P1 Page 1 Figure_P2 Page 2 Figure_P3 Page 3 Figure_P4 Page 4 Figure_P5 Page 5 Figure_P6 Page 6 Figure_P7 Page 7 Table_G1 Note: To print large tables and graphs users may have to change their printer settings to landscape and use a small font size.
Glossary
======================================================================================
Abbreviations used in the SUIDIRF
CPR Cardiopulmonary resuscitation NA Not applicable
DC Death certificate NOK Next of kin
DOA Dead on arrival OTC Over-the-counter medication
DOB Date of birth Rx Prescription medication
EMS Emergency medical services SIDS Sudden infant death syndrome
IV Intravenous SS# Social security number
ME/C Medical examiner or coroner Unk Unknown
Terminology
EMS caller. The person who first called Last caregiver. The person who was
for emergency medical services, last responsible for the care of the
including an ambulance service, the infant when he or she was discovered
police, or the fire department rescue dead, unresponsive, or in distress
team. (e.g., a baby-sitter, a child care custo-
dian, or the mother).
EMS responder. The person who first
responded on behalf of the emergency Last witness. The person who last
medical service agency. observed the infant alive or presum-
ably alive in or near the area where he
Father. The person serving as the or she was discovered dead,
father at the time of the incident. The unresponsive, or in distress.
relationship as natural (birth) father,
stepfather, or other should be indi- Mother. The person serving as mother
cated. of the infant at the time of the incident.
The relationship as natural (birth)
Finder. The person who discovered mother, stepmother, or other should
the infant dead, unresponsive, or in be indicated.
distress.
Placer. The person who last placed the
First responder. The first person who infant in or near the area where he or
attempted to render aid when the she was found dead, unresponsive, or
infant was found dead, unresponsive, in distress.
or in distress.
Police. The law enforcement officer
Health-care provider. The physician, responsible for completing the police
nurse, clinician, or other medical report on the death scene investi-
service provider who usually gave the gation.
infant medical care or well-baby
checkups. Usual caregiver. The person
responsible for providing the usual,
ongoing care for the infant (e.g.,
changing diapers and feeding).
======================================================================================
Return to top. Figure_P1 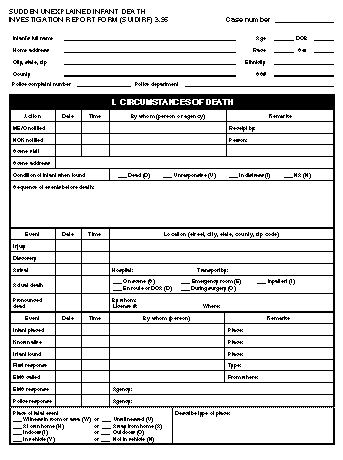 Return to top. Figure_P2 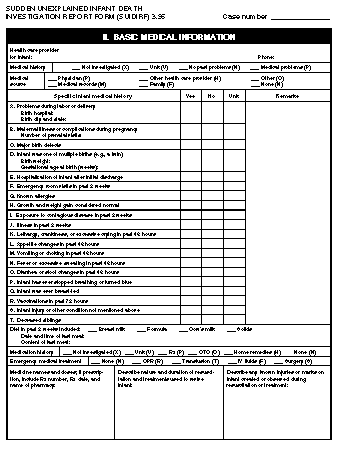 Return to top. Figure_P3  Return to top. Figure_P4  Return to top. Figure_P5 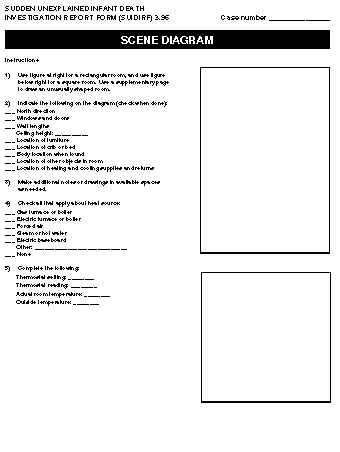 Return to top. Figure_P6 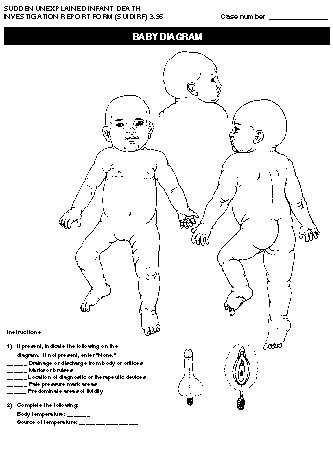 Return to top. Figure_P7  Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 09/19/98 |
|||||||||
This page last reviewed 5/2/01
|