 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Outbreak of Salmonella Serotype Typhimurium Infection Associated with Eating Raw Ground Beef -- Wisconsin, 1994Despite previously publicized outbreaks of illness associated with and recommendations to avoid eating undercooked meat, some persons continue to eat under-cooked or raw meat. This report summarizes the investigation of an outbreak of Salmonella serotype Typhimurium gastrointestinal illness in Wisconsin associated with eating contaminated raw ground beef during the 1994 winter holiday season. On December 29, 1994, physicians in a group medical practice in Dodge County (1994 estimated population: 79,360), Wisconsin, reported to the Public Health Unit of the Dodge County Human Services and Health Department (DCHSHD) that during December 27-29 they had treated 17 patients with acute gastrointestinal illness characterized by diarrhea and abdominal cramps. At least 14 patients reported having eaten raw ground beef that was either plain or seasoned with onions and an herb mix during the 72 hours before illness onset. Stool samples for culture were obtained from 11 patients; Salmonella serotype Typhimurium that did not ferment tartrate was isolated from seven specimens. Based on these reports and findings, the DCHSHD issued a physician alert and press release that encouraged affected residents to report their illnesses and physicians to obtain stool cultures from case-patients. In addition, DCHSHD and the Bureau of Public Health, Wisconsin Division of Health (WDOH), initiated an investigation of this outbreak. A probable case of Salmonella infection was defined as diarrhea or abdominal cramps with onset during December 22, 1994-January 4, 1995, in a resident of or a visitor to Dodge County or any of the four contiguous counties. A confirmed case was defined as a stool culture positive for tartrate-negative Salmonella Typhimurium. DCHSHD and WDOH identified 107 confirmed and 51 probable case-patients (Figure_1); of these, 17 (16%) were hospitalized. Predominant manifestations of illness included diarrhea (98%), abdominal cramps (88%), chills (77%), body aches (71%), fever (65%), nausea (60%), and bloody stools (43%). The ages of ill persons ranged from 2 years to 90 years; 62% were male. To assess potential risk factors for illness, DCHSHD and WDOH conducted a case-control study including 40 case-patients who were randomly selected from the persons with a stool specimen culture positive for tartrate-negative Salmonella Typhimurium and 40 controls who were identified by random telephone digit dialing. The mean ages of cases and controls were similar (43 years for cases; 47 years for controls). Of 40 case-patients, 35 (88%) reported having eaten raw ground beef during December 22-January 4, compared with eight (20%) of 40 controls (odds ratio {OR}=28; 95% confidence interval {CI}=7-117). Among the 35 who ate raw ground beef, 34 (97%) had purchased the beef from one butcher shop, compared with three (37%) of the eight controls (OR=56; 95% CI=4-1881). Knowledge of previous reports of outbreaks related to eating raw or undercooked beef was less among ill persons than among controls (26 {65%} of 40 case-patients compared with 30 {75%} of 40 controls {OR=0.6; 95% CI=0.2-1.8}). However, 22 (85%) of the 26 case-patients who reported being aware of previous outbreaks associated with consumption of raw ground beef continued this behavior compared with seven (23%) of the 30 controls with knowledge of previous outbreaks (OR=18.1; 95% CI=4.0-92.0). DCHSHD and WDOH obtained from case-patients six leftover samples of raw ground beef that had been purchased at the butcher shop on five dates during December 21-29 and served in different homes. These samples were cultured for Salmonella sp.; all grew tartrate-negative Salmonella Typhimurium. On December 30, 1994, staff of the Meat Safety and Inspection Bureau (MSIB), Wisconsin Department of Agriculture, Trade, and Consumer Protection (WDATCP), informed the proprietor of the butcher shop of a potential problem with consumption of raw ground beef from the shop and the need to properly label meat products. During the winter holiday season, the butcher shop sold both seasoned and unseasoned raw ground beef that had a warning label regarding safe handling of poultry. On January 2, 1995, inspectors from MSIB examined sanitary conditions in the butcher shop, obtained invoices indicating the origin and the quantity of the meat used to prepare the ground beef, and inspected the raw ground beef production method and selling practice in the butcher shop. Meat from approximately 35 carcasses obtained from three different suppliers had been ground in the shop from December 21 through January 4. Leftover product was reported to have been discarded each day and not carried over for sale the next day. All parts of the meat grinder except for the auger housing were disassembled and individually cleaned and sanitized at the end of each day. This type of grinder allowed easy disassembly of the auger and other smaller parts; the auger housing was attached to the grinder with nuts and bolts and required a wrench for removal. However, the cleaning staff had not received instructions regarding removal of the auger housing and had cleaned only surfaces of the tunnel-like space for the auger with a brush. Meat remnants were present in the auger housing when the grinder was disassembled. Twenty environmental swabs of the equipment and the areas related to the production of the ground beef were obtained for bacterial culture; all were negative for Salmonella sp. Stool specimens obtained from all five butchers at the shop were cultured; one was positive for tartrate-negative Salmonella Typhimurium. Although this butcher denied illness, he had eaten raw ground beef at the shop during the outbreak interval. Reported by: PA Frazak, MPH, Public Health Unit, Dodge County Human Svcs and Health Dept; JJ Kazmierczak, DVM, ME Proctor, PhD, JP Davis, MD, State Epidemiologist for Communicable Diseases, Bur of Public Health, Wisconsin Div of Health; J Larson, R Loerke, Meat Safety and Inspection Bur, Wisconsin Dept of Agriculture, Trade, and Consumer Protection. Div of Bacterial and Mycotic Diseases, National Center for Infectious Diseases; Div of Field Epidemiology, Epidemiology Program Office, CDC. Editorial NoteEditorial Note: The investigation of this outbreak implicated consumption of contaminated raw ground beef as the source of Salmonella infection. Inadequate cleaning and sanitization of the meat grinder probably resulted in ongoing contamination of ground beef over many production days. The outbreak occurred during the winter holiday season, and some patients reported that consumption of raw ground beef during these holidays was a practice brought from Europe by their ancestors. The decline of cases after the holidays may have occurred because ground beef from the implicated butcher shop was no longer consumed raw or because the grinder was cleaned more thoroughly after WDATCP personnel spoke with the proprietor of the butcher shop on December 30. The five persons who became ill but did not report eating raw ground beef may not have remembered eating the raw ground beef, may have eaten undercooked ground beef or food that was contaminated from the raw ground beef, or may have become ill through person-to-person transmission. Raw ground beef previously has been implicated as a vehicle for transmission of Salmonella (1,2), and undercooked ground beef is the most frequently recognized vehicle for Escherichia coli O157:H7 infection (3). The prevalence of Salmonella in beef ranges from 1% for raw beef carcasses (4) to 5%-7% for ground beef (U.S. Department of Agriculture, Food Safety and Inspection Service, unpublished data, 1994). Prevention measures include warning consumers of the health risks associated with eating raw ground beef and encouraging them to thoroughly cook ground beef and to adhere to safe foodhandling guidelines. Safe cooking and handling labels on raw or partially cooked meat and poultry are now required by the U.S. Department of Agriculture (USDA). However, the presence of safe foodhandling labels does not ensure adherence to safe practices. For example, an investigation of risk factors for sporadic E. coli O157:H7 infection indicated that of 43 food preparers who reported reading the safe foodhandling label on meat packages, 33 (77%) admitted to practices specifically discouraged on the label (5). The investigation in Dodge County underscores that knowledge of health risks is not consistently associated with desirable changes in behavior. Despite public health warnings and publicity about related outbreaks, some consumers in Dodge County and elsewhere have continued to eat raw or undercooked foods of animal origin. For example, a telephone survey of a national sample of adults conducted by the Center for Food Safety and Applied Nutrition, Food and Drug Administration (FDA), during December 1992-February 1993 indicated that 53% consumed raw eggs; 23%, undercooked hamburgers; 17%, raw clams or oysters; 8%, raw sushi or ceviche; and 5%, steak tartare (raw hamburger meat) (6). Consumer advisories can be more effective if targeted to specific cultural or ethnic groups with such high-risk dietary practices, and WDATCP is planning two press releases this winter holiday period to warn consumers of the risks associated with eating raw ground beef. In addition to consumer advisories, interventions to reduce the risks associated with the consumption of ground beef include the needs for 1) producers of ground beef to emphasize employee education and training on the recommended methods of cleaning and sanitizing meat-grinding equipment; 2) manufacturers to design meat-grinding equipment that is easily accessible for cleaning and sanitization; and 3) state regulatory and inspection authorities to adopt and enforce FDA's Food Code model requirements, which offer specific recommendations for handling, cooking, and storing raw meat; cleaning and sanitizing equipment and utensils; designing and constructing equipment; and advising consumers about the risks associated with consumption of raw or undercooked food of animal origin (7). The USDA's Food Safety and Inspection Service also has proposed changes in the meat and poultry inspection system to improve assessment and control of microbial pathogens in raw meat and poultry (8). Consumers can obtain more information on safe meat handling from the USDA's Meat and Poultry Hotline (telephone {800} 535-4555). References
Figure_1 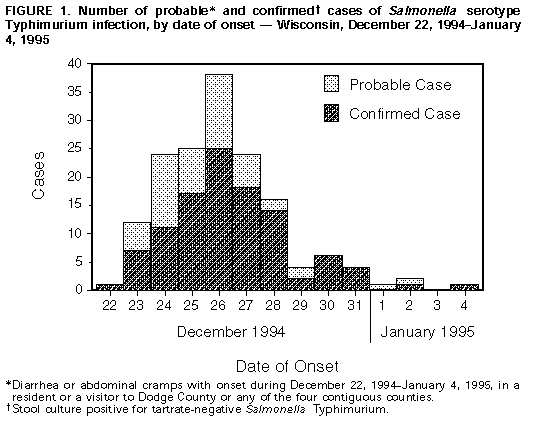 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 09/19/98 |
|||||||||
This page last reviewed 5/2/01
|