 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Differences in Maternal Mortality Among Black and White Women -- United States, 1990The risk for maternal mortality has consistently been higher among black women than white women. The 1990 national health objective of reducing maternal mortality to no more than five deaths per 100,000 live births for any racial/ethnic group was nearly achieved for white women, for whom the maternal mortality ratio * was 5.7 in 1990 (1); for black women, however, the ratio was 18.6. The year 2000 national health objectives include reducing the overall maternal mortality ratio to no more than 3.3 deaths per 100,000 live births and to no more than five for blacks (objective 14.3) (2). This report summarizes race-specific differences in maternal mortality among black and white women for 1990 and compares these with trends in mortality from 1940-1990. Maternal mortality ratios were calculated at 10-year intervals from 1940 to 1990 using data contained on death certificates filed in state vital statistics offices and compiled by CDC in a national database (3,4). Maternal deaths were defined as those for which a maternal condition was designated as the underlying cause of death, as recorded on the death certificate by the attending physician, medical examiner, or coroner. ** This report compares maternal mortality only for black and white women because data for other racial/ethnic groups were not available for all years; data for Hispanic women are included in the totals for both blacks and whites. In 1990, the overall maternal mortality ratio was 8.0 deaths per 100,000 live births, a 98% decline from 363.9 in 1940. From 1940 to 1990, race-specific ratios declined substantially, from 319.8 to 5.7 for white women and from 781.7 to 18.6 for black women. Although the percentage decline was similar for black women and white women (97.6% and 98.2%, respectively), the ratios for black women were consistently two to four times higher than those for white women. For example, compared with that for white women, the maternal mortality ratio for black women was 2.4 times greater in 1940, 3.6 times greater in 1950, 4.1 times greater in 1960, 3.9 times greater in 1970, 3.4 times greater in 1980, and 3.3 times greater in 1990 (Figure_1, page 13). From 1960 through 1990 (years for which more detailed data were available), the maternal mortality ratio was higher for black women in all age groups and for each of the major causes of death. The black-white differential was greatest for pregnancies that did not end in a live birth, such as ectopic pregnancy, spontaneous abortion, induced abortion, and gestational trophoblastic disease. *** Reported by: Div of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion; Div of Vital Statistics, National Center for Health Statistics, CDC. Editorial NoteEditorial Note: Despite overall improved maternal survival during 1940-1990, black women were more than three times more likely than white women to die from complications of pregnancy, childbirth, and the puerperium. Although the reasons for this disparity are unclear, possible explanations include differences in pregnancy-related morbidity, access to and use of health-care services, and content and quality of care. Maternal hospitalization, except when associated with delivery, can serve as a marker for severe maternal morbidity. For example, during 1987-1988, a study of pregnancy-related hospitalizations indicated the ratio for black women was 1.4 times that for white women (6); during the same period, the black-white maternal mortality ratio was 3.1. However, in a study of women in the military -- who have unrestricted access to prenatal care -- there was virtually no difference between black and white women in the overall prevalence of antenatal hospitalization and in the indications for hospitalization (7). Early entry into prenatal care (i.e., during the first trimester) -- one indicator of access to and use of pregnancy-related health care -- has been assessed for women whose pregnancies ended in a live birth. During 1980-1990, although 76% of all mothers received early prenatal care, the percentage of black women who did not receive early prenatal care was nearly twice that for white women (8). In 1990, 39.4% of black mothers did not receive early prenatal care, compared with 20.8% of white mothers. Once women enter prenatal care, studies indicate differences between black and white women in the advice given to them and use of technology (9,10). Data describing access to pregnancy-related health care other than prenatal care (e.g., gynecologic services) or the content and quality of health care once women obtain these services are limited. Narrowing discrepancies in maternal mortality between black and white women will require evaluating and addressing race-specific differences in morbidity and in access to and use and content of pregnancy-related care. Addressing discrepancies in maternal mortality also may improve maternal morbidity and infant survival. References
* The maternal mortality ratio is the number of maternal deaths per 100,000 live births. CDC's National Center for Health Statistics (NCHS) uses the term maternal mortality rate as required by the World Health Organization. In this report, the term "ratio" is used because the numerator includes some maternal deaths that were not related to live births, and thus were not included in the denominator. For this analysis, 3 years of data were combined to calculate maternal mortality ratios to promote statistical reliability and stability in the estimates. For example, 1990 ratios are based on data from 1989 through 1991. In addition, beginning with the 1989 data year, NCHS began using race of mother instead of race of child to tabulate live birth and fetal death data by race. In this analysis, race for live births is tabulated by the race of the child for maternal mortality to maintain comparability of ratios. ** An underlying cause of death is defined by the International Classification of Diseases, Ninth Revision (ICD-9), as "a) the disease or injury which initiated the train of morbid events leading directly to death, or b) the circumstances of the accident or violence which produced the fatal injury. provided the first formal definition of maternal mortality, defining maternal death as the death of a woman while pregnant or within 42 days of termination of pregnancy. This definition differed from that used previously by NCHS, which included deaths up to 1 year after termination of pregnancy. However, the change from the 1-year limit used in the eighth revision to the 42-day limit used in the ninth revision did not greatly affect the comparability of maternal mortality statistics (4). *** The ICD code is revised approximately every 10 years. In the ninth revision, ectopic pregnancy (ICDA code 631) was transferred from complications of pregnancy (ICDA codes 630 -- 634) to pregnancy with abortive outcomes (ICD codes 630 -- 638) (5). In this report, maternal deaths from ectopic pregnancy are included with abortive outcomes for all time periods. Figure_1 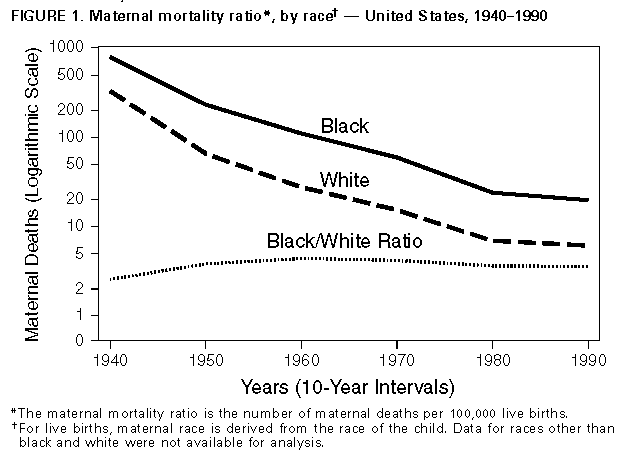 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 09/19/98 |
|||||||||
This page last reviewed 5/2/01
|