 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Addressing Emerging Infectious Disease Threats: A Prevention Strategy for the United States Executive SummaryIngenuity, knowledge, and organization alter but cannot cancel humanity's vulnerability to invasion by parasitic forms of life. Infectious disease which antedated the emergence of humankind will last as long as humanity itself, and will surely remain, as it has been hitherto, one of the fundamental parameters and determinants of human history.
Summary The spectrum of infectious disease is changing rapidly in conjunction with dramatic societal and environmental changes. World- wide, explosive population growth with expanding poverty and urban migration is occurring; international travel and commerce are increasing; and technology is rapidly changing -- all of which affect the risk of exposure to infectious agents. Recent examples of important emerging infectious diseases include prolonged diarrheal illness due to waterborne Cryptosporidium, hemorrhagic colitis and renal failure from foodborne Escherichia coli O157:H7, pneumonia and middle-ear infections caused by drug-resistant pneumococci, and rodentborne hantavirus pulmonary syndrome. These diseases as well as resurgent diseases (e.g., tuberculosis and cholera) illustrate human vulnerability to microorganisms in the environment. Three recent reports by the Institute of Medicine document the need to address emerging infectious disease threats. In partnership with representatives from health departments, other federal agencies, medical and public health professional associ- ations, and international organizations, CDC has developed a strategic plan to address emerging infectious disease threats. The plan contains four goals that emphasize surveillance, applied research, prevention and control, and public health infrastructure. To ensure sustain- ability, plan implementation will be approached in stages, as a long- term endeavor with emphasis on extramural programs. As health-care reform proceeds, priority should be given to strengthening partner- ships between health-care providers, microbiologists, and public health professionals to detect and control emerging infectious diseases. INTRODUCTION Once expected to be eliminated as a public health problem, infectious diseases remain the leading cause of death and disability- adjusted life years (DALYs) worldwide (1) and are among the leading causes of death in the United States (2). Dramatic changes in society, technology, and the environment, together with the diminished effectiveness of certain approaches to disease control, usher in an era wherein the spectrum of infectious diseases is expanding, and many infectious diseases once thought to be controlled are increasing (Box 1 Table_B1). The term "emerging infectious diseases" refers to diseases of infectious origin whose incidence in humans has either increased within the past two decades or threatens to increase in the near future (3). To effectively address emerging infectious diseases, CDC has developed a strategic plan emphasizing surveillance, research, and prevention activities necessary to maintain a strong defense against infectious diseases that affect, or threaten to affect, the public's health. The goals of this plan address priorities for surveillance, applied research, prevention and control, and public health infra- structure, respectively: Goal I. Detect, promptly investigate, and monitor emerging patho- gens, the diseases they cause, and the factors influencing their emergence. Goal II. Integrate laboratory science and epidemiology to optimize public health practice. Goal III. Enhance communication of public health information about emerging diseases and ensure prompt implementation of prevention strategies. Goal IV. Strengthen local, state, and federal public health infra- structures to support surveillance and implement prevention and control programs. BACKGROUND The Concept of Emergence Many factors or combinations of factors can contribute to disease emergence. Newly emergent infectious diseases may result from changes in or evolution of existing organisms; known diseases may spread to new geographic areas or human populations; or previously unrecognized infections may appear in persons living or working in areas undergoing ecologic changes (e.g., deforestation or reforestation) that increase human exposure to insects, animals, or environmental sources that may harbor new or unusual infectious agents (Table_1) (4-7). Infectious diseases may reemerge because of either the develop- ment of antimicrobial resistance in existing agents (e.g., gonorrhea, malaria, pneumococci) or breakdowns in public health measures for previously controlled infections (e.g., cholera, tuberculosis, and pertussis) (3). The Burden of Infectious Diseases In the United States and elsewhere, infectious diseases increas- ingly threaten public health and contribute substantially to the esca- lating costs of health care. For example, childhood ear infections are the leading cause of patient visits to pediatricians, and the incidence of visits for these infections increased 150% during 1975- 1990 (8). In addition, infectious agents may be causing diseases previously considered noninfectious: Helicobacter pylori has a well- established association with peptic ulcer disease and gastritis (9); sexually transmitted human papillomavirus is associated with cervical cancer (10); and infection with hepatitis C virus -- now recognized as a leading cause of chronic liver disease and cirrhosis in the United States -- occurs in an estimated 150,000 persons annually (11). Chlamydia infections have long been implicated in infertility and, more recently, have been tentatively associated with coronary artery disease (12), and rodentborne hantaviruses may play a role in hyper- tensive renal disease (13). Infectious diseases account for 25% of all visits to physicians each year, and antimicrobial agents are the second most frequently prescribed class of drugs in the United States. (14,15). Direct and indirect costs of infectious diseases (e.g., economic losses and days of disability) may exceed an estimated $120 billion. Such approxi- mations, however, most likely underestimate the burden of infectious diseases. For example, the International Classification of Diseases (ICD-9) distributes infectious diseases across several categories, obscuring their public health impact (e.g., the classification of endocarditis among cardiovascular diseases and the classification of meningitis and middle-ear infections among diseases of the nervous system and sense organs, respectively). The Threat of Emerging Infections As a consequence of changes in society, technology, and the environment, pathogens evolve or spread, and the spectrum of infectious diseases expands. Emerging infections, such as human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS), illustrate that no nation can be complacent regarding human vulnerability to microorganisms in the environment. Since the early 1970s, the U.S. public health system has been challenged by other newly identified pathogens and syndromes, such as Legionnaires' disease, Lyme disease, toxic shock syndrome, hepatitis C virus, and, most recently, hantavirus pulmonary syndrome (16-23). Moreover, the incidence of many diseases widely presumed to be under control -- such as cholera (24), dengue (25), yellow fever (26), and tuberculosis (TB) (27,28) -- has increased in many areas or spread to new regions or populations throughout the world. Because of widespread use and misuse of antimicrobial drugs, their effectiveness in treating common bacterial infections is diminishing, resulting in prolonged illnesses, higher mortality rates, and higher health-care costs (Figure_1) (29-35). Emerging infections are particularly serious in persons with lowered immunity, such as those infected with HIV and those receiving immunosuppressive therapy for cancer or organ transplantation -- populations whose numbers are increasing (Figure_2). Other groups that may be disproportionately affected by emerging infections include the elderly; persons being cared for in institutional settings, such as hospitals and nursing homes; and persons with inadequate access to health care, such as the homeless, migrant farm workers, and others of low socioeconomic status. The number of children attending day care facilities has increased in the past decade as more mothers of young children have entered the work force. These children, now numbering more than 11 million, are at a substantially increased risk for enteric infections, such as hepatitis A, giardiasis, and cryptosporidiosis; acute respir- atory illnesses; and middle-ear infections. Also, children who become infected can infect other members of a household (36). Emerging infections transmitted by contaminated public water supplies place entire communities at risk. In the spring of 1993, contamination of a municipal water supply with the intestinal parasite Cryptosporidium caused the largest recognized outbreak of waterborne illness in the history of the United States; an estimated 403,000 persons in Milwaukee, Wisconsin, had prolonged diarrhea, and approxi- mately 4,400 persons required hospitalization (personal communication, Jeffrey P. Davis, communicable disease epidemiologist, Wisconsin). Large segments of populations may also be exposed to emerging infections through contaminated food products. For example, in 1993, hamburgers contaminated with the bacterial pathogen Escherichia coli O157:H7 and served at a fast-food restaurant chain caused a multistate outbreak of hemorrhagic colitis (bloody diarrhea) and serious kidney disease, resulting in the deaths of at least four children (37,38). Limitations in both surveillance and the availability of appro- priate diagnostic tests constrain public health efforts to prevent and control outbreaks. Both E. coli O157:H7 and Cryptosporidium were first recognized as important human pathogens in the early 1980s, but neither has received adequate public health attention (Figure_3). Exposure to certain animals also poses a risk for emerging infectious diseases. Hantavirus pulmonary syndrome, first recognized in the southwestern United States in 1993, has been linked to exposure to infected rodents in more than a dozen states. More than 60 cases have been detected; of those, more than half have died (Figure_4) (20-23). Once considered "exotic," tropical infectious diseases are having an increasing effect on the U.S. public. Recent examples include severe illness and at least one death due to cholera among interna- tional airline passengers arriving in California (39); malaria among residents of southern California and immigrants in North Carolina (40,41); fever and heart failure in New York and Canada among patients who received blood transfusions contaminated with the bloodborne parasite (Trypanosoma cruzi) that causes Chagas' disease in Latin America (42,43); and a newly described form of leishmaniasis among troops returning from the Persian Gulf conflict (44,45). From a historical perspective, cholera, smallpox, and plague are examples of infectious diseases that spread globally with devastating impact, often during periods of rapid economic change or population growth (7). Today, travel and commerce have fostered the worldwide spread of pathogens such as HIV/AIDS and influenza, as well as the reemergence of cholera as a global health threat -- consistent with a perspective that "the microbe that felled one child in a distant continent yesterday can reach yours today and seed a global pandemic tomorrow" (46). These examples underscore the fact that emerging infections can affect persons in geographically widespread areas, regardless of factors such as lifestyle, cultural or ethnic back- ground, or socioeconomic status. Preparing to Confront Emerging Infections The public health infrastructure is insufficiently prepared to confront today's emerging disease problems. Domestic surveillance systems for most infectious diseases are inadequate and global surveillance is fragmentary at best. For example, foodborne and waterborne disease outbreaks may be either unrecognized or detected late, and the magnitude of the problem of antimicrobial drug resistance is unknown. Surveillance of infectious diseases in the United States depends on voluntary collaboration between CDC and state and local health departments, which depend on reporting by health-care professionals of a limited number of specific, recognized infectious diseases. Reporting is generally incomplete. Results of a recent survey conducted by the Council of State and Territorial Epidemiologists underscore the inadequacy of existing infectious disease surveillance by documenting the limited number of professional positions dedicated to infectious disease surveillance in most states. For example, in 12 of the 50 states surveyed, no professional position is dedicated to surveillance of foodborne and waterborne diseases. Funding for infectious disease surveillance is restricted primarily to diseases for which public health crises have already developed. In 1992, more than 95% of federal funds allocated to states for infectious disease surveillance were targeted to four disease categories (i.e., TB, HIV/AIDS, sexually transmitted diseases {STDs}, and selected vaccine-preventable diseases) (personal communication, M. Osterholm, Council of State and Territorial Epidemiologists survey on surveil- lance). However, no federal resources are provided to state and local health departments to support the national notifiable disease system. In addition, the ability of state public health laboratories to support the surveillance and control of infectious diseases has diminished (47). Timely recognition of emerging infections requires early warning systems to detect such problems so they may be promptly investigated and controlled before they evolve into public health crises. Prompt detection of these new threats depends on careful monitoring by effective surveillance systems; on a thorough understanding of trends in incidence and distribution of known infectious agents; and on effective communication among clinicians, clinical laboratory personnel, and public health professionals. The ability to detect what is new or reemerging depends on the capacity to identify and track both the routine and the unusual. Like radar or "early warning" systems that detect threats to national security, surveillance with appropriate laboratory support is a critical element in the effective defense against these diseases. Surveillance systems are the most important tools for determining which infectious diseases are emerging or receding. Effective surveillance also provides a basis for evaluating the outcome of both public health and personal medical-care programs. Surveillance information is essential to ensure the use of the most efficacious and cost-effective approaches to preventive, as well as curative, health care. Regardless of the direction of health-care reform, surveillance will be critical to the meaningful evaluation of new prevention programs. In addition to comprehensive and innovative surveillance systems, effective preparation for detecting, preventing, and controlling emerging infectious diseases requires sound foundations in profes- sional expertise, laboratory support, and research capability to strengthen the infrastructure needed to address the ongoing, but often changing, threats from emerging infections. Despite the continued emergence of such threats, support for applied research and control efforts has declined over the past decade. Three recent reports by expert committees convened by the National Academy of Science's Institute of Medicine (IOM) have indi- cated that the ability of the U.S. public health system and health professionals to address emerging infectious disease problems is in jeopardy (3,48,49). The earliest of these reports, "The U.S. Capacity to Address Tropical Infectious Disease Problems" (48), documented the inadequate state of readiness to recognize, treat, or control infectious disease threats emanating from the tropics -- regions that have yielded microbial threats such as Lassa fever and Ebola viruses, chloroquine-resistant malaria, and penicillin-resistant gonorrhea. The second report, "The Future of Public Health," concluded that the U.S. public health system is in disarray. This report emphasized that the U.S. approach to public health has too often been crisis driven, an approach that is costly because it constrains the institution of cost-saving preventive strategies (49). The third IOM report, "Emerging Infections, Microbial Threats to Health in the United States," emphasized the ongoing threat to domestic and global health from emerging infectious diseases (3). The report provided specific recommendations for CDC, the National Institutes of Health, the Food and Drug Administration, the Department of Defense, and other federal and state agencies for addressing microbial threats to health in the United States and elsewhere. This report emphasized a critical leadership role for CDC in a national and global effort to detect and control emerging infectious disease threats. THE CDC PREVENTION STRATEGY To effectively detect and prevent emerging infections, improve- ments are needed in public health systems, program design, and infra- structure. To accomplish these improvements and to achieve the objectives of Healthy People 2000, CDC has developed a strategy to address these microbial threats. Because meeting the broad challenge of emerging infections requires interaction, cooperation, and coordination among a wide range of public and private organizations, the development of this strategy has taken place in partnership with state and local health departments, other federal agencies, academic institutions, health-care providers, medical laboratory personnel, and international organizations. The prevention strategy outlined in this document contains four critical goals that address, in a broader context, specific IOM recom- mendations for revitalizing the ability to identify, contain, and, most importantly, prevent illness from emerging infectious diseases (Box 2 Table_B2). Goal I (Surveillance) emphasizes the improvement and expansion of surveillance capabilities for infectious diseases in the United States and internationally. This goal includes plans for strengthening local and state public health programs for infectious disease surveillance, establishing provider-based sentinel surveillance networks, and creating population-based Emerging Infections Epidemiology and Prevention Centers at different sites throughout the United States (Table_2). Also included are plans for a global consortium of closely linked epidemiology/biomedical research centers to promote the detection, monitoring, and investigation of emerging infections (Box 3 Table_B3). Other objectives emphasize improved detection and monitoring of trends in antimicrobial resistance in both institutional and community settings; expansion of field investigations and epidemic response capabilities; prevention of foodborne and waterborne infectious diseases and improved knowledge of the distribution of animal reservoirs and vectors associated with human infectious diseases. Goal II (Applied Research) focuses on applied research and the integration of laboratory science and epidemiology with public health practice. Emphasis is placed on determining how behavioral factors influence exposure to new infections; better characterizing the health burden of both well-established and emerging infections; and evalu- ating the effectiveness and economic benefit of strategies to prevent emerging infectious diseases. An additional focus is the development and application of improved laboratory techniques for the identifi- cation of new pathogens and the expanded use of molecular epidemio- logic techniques in investigating emerging diseases. Supporting the national Childhood Immunization Initiative by conducting vaccine efficacy studies and improving rapid response capabilities for vaccine development and delivery is also a priority. A final focus is the reestablishment of CDC extramural programs to promote effective partnerships with public agencies, universities, and private industry and to support applied research in surveillance, epidemiology, and prevention of emerging infections. Goal III (Prevention and Control) addresses enhanced communi- cation of public health information and the implementation of prevention strategies for emerging infections. Highlighted under this goal are proposals for expanded dissemination of the MMWR, as well as other important public health information sources. Another priority is the creation of an accessible and comprehensive infectious disease database for the United States that increases awareness of infectious diseases and promotes public health action. The database will contain current information on topics such as antimicrobial resistance, foodborne and waterborne disease outbreaks, travelers' health, antimicrobial drug availability, vaccine-preventable diseases, and vaccine guidelines. This goal also addresses the development and implementation of guidelines for preventing emerging infectious diseases and the provision of critical prevention materials. Goal IV (Infrastructure) deals with issues relating to local, state, and federal infrastructure, particularly personnel and physical resources. Points of emphasis include maintaining expertise in rare or unusual infectious diseases and establishing training programs that emphasize the diagnosis of infectious diseases. A public health laboratory fellowship in infectious diseases is proposed. Also emphasized is the need for state-of-the-art physical resources such as laboratory space, training facilities, and equipment. Laboratory capabilities must be maintained in a manner that optimizes flexibility and "surge capacity" so that unanticipated public health threats can be adequately, efficiently, and safely addressed. Plans for expanding facilities for maintaining specimen banks of etiologic agents and clinical specimens are also a priority. IMPLEMENTATION This plan reflects CDC's commitment to meet the urgent public health challenge of important emerging infectious diseases. The need to proceed rapidly is made more urgent for many reasons. Many diseases pose an immediate danger. For example, methicillin-resistant Staphylococcus aureus, a common cause of hospital infections, may potentially develop resistance to vancomycin (29,50); penicillin resistance is spreading in Streptococcus pneumoniae (29,31,51); the potential exists for extension of the current cholera epidemic in Latin America to the Caribbean Islands (24); and Vibrio cholerae O139, a new strain for which existing cholera vaccines are ineffective and prior infection with V. cholerae O1 affords no protection, is spreading throughout southern Asia (Figure_5) (52,53). Changing food-industry practices, dietary choices, and globalization of food supplies will bring new challenges to provide a diet safe from pathogens such as Salmonella sp. and E. coli O157:H7 (37,38,54-57). Ongoing investigations of hantavirus pulmonary syndrome document that the geographic distribution of this infection goes beyond the desert Southwest (23). These infectious disease problems emphasize the necessity of expeditiously implementing this plan through a balanced intramural and extramural effort. The implementation of the goals and objectives in this plan is relevant to health-care reform. Examples of relevant issues include prolonged hospitalizations caused by hospital-acquired infections; increased morbidity and treatment costs resulting from antimicrobial drug resistance; and excessive burdens placed on public and private health-care delivery facilities because of community-wide outbreaks of foodborne and waterborne infections. Some of the activities listed in this document are already in the planning stages and will be implemented soon. Many of the proposed activities need further development in full cooperation with other federal agencies, state and local health authorities, academic insti- tutions, professional societies, private industry, and others. With this document serving as both a guide and a first step, implementation will be based on public health priorities and resource availability. This process will be approached in stages, as a long-term endeavor with sustainable impact and emphasis on extramural programs (Box 4 Table_B4). The strategy of this plan is based on repeated experience demon- strating that it is less costly to anticipate and prevent infectious disease threats than to react with expensive treatment or containment measures to public health crises. Public health policy and practice that combine investments in surveillance, laboratory research and training, and epidemiologic investigations with prevention and control efforts will reduce the impact of emerging infectious disease threats, in terms of both human suffering and economic losses. Acknowledgments Development of this plan began in December 1992 with consultation from the Board of Scientific Counselors of CDC's National Center for Infectious Diseases. Further guidance was provided at a meeting of infectious disease and public health experts in Atlanta in March 1993 and at a meeting of state and territorial public health epidemio- logists, laboratory directors, and veterinarians in Minneapolis in June 1993. Drafts of this plan have also been reviewed by leaders of numerous medical, scientific, and public health organizations. We thank the following individuals for their comments and suggestions: James R. Allen, Henry Anderson, Larry J. Anderson, Douglas L. Archer, Thomas Arrowsmith-Lowe, William H. Bancroft, C.L.R. Bartlett, Nancy H. Bean, David M. Bell, Abram S. Benenson, John E. Bennett, John V. Bennett, Bobbie A. Berkowitz, Guthrie S. Birkhead, Paul A. Blake, Coleen A. Boyle, Philip S. Brachman, Windell R. Bradford, A.D. Brandling-Bennett, Joel G. Breman, Don J. Brenner, Claire V. Broome, George T. Bryan, James W. Buehler, Michael J. Burkhart, Jay C. Butler, Ronald L. Cada, Carlos C. Campbell, Grant R. Campbell, Roger H. Carlson, Gail H. Cassell, Kenneth G. Castro, Willard Cates, Jr., Mary Ann Chiasson, Gary G. Clark, Barnett L. Cline, Mitchell L. Cohen, Daniel G. Colley, Mary-Paxton D. Colley, E. Mary Cooke, Jose F. Cordero, Jon M. Counts, Nancy J. Cox, Donald E. Craven, James W. Curran, Mary Ann Danello, Jeffrey P. Davis, Barbara
References
======================================================== BOX 1. Examples of emerging infectious diseases, 1993 Diseases in the United States -- Coccidioidomycosis -- Cryptosporidiosis -- Drug-resistant pneumococcal disease -- Escherichia coli O157:H7 disease -- Hantavirus pulmonary syndrome -- Influenza A/Beijing/32/92 -- Vancomycin-resistant enterococcal infections Diseases outside the United States -- Cholera, Latin America -- Dengue, Costa Rica -- Diphtheria, Russia -- E. coli O157:H7, South Africa and Swaziland -- Multidrug-resistant Shigella dysenteriae, Burundi -- Rift Valley fever, Egypt -- Vibrio cholerae O139, Asia -- Yellow fever, Kenya ======================================================== Return to top. Table_1 Note: To print large tables and graphs users may have to change their printer settings to landscape and use a small font size.
TABLE 1. Factors contributing to emergence of infectious diseases *
===============================================================================================
Categories Specific examples
---------------------------------------------------------------------------------------------
Societal events Economic impoverishment; war or civil conflict; population
growth and migration; urban decay
Health care New medical devices; organ or tissue transplantation; drugs
causing immunosuppression; widespread use of antibiotics
Food production Globalization of food supplies; changes in food processing,
packaging, and preparation
Human behavior Sexual behavior; drug use; travel; diet; outdoor recreation;
use of day care facilities
Environmental changes Deforestation/reforestation; changes in water ecosystems;
flood/drought; famine; global warming
Public health infrastructure Curtailment or reduction of prevention programs; inadequate
communicable disease surveillance; lack of trained
personnel (e.g., epidemiologists, laboratory scientists, and
vector and rodent control specialists)
Microbial adaptation Changes in virulence and toxin production; development of
and change drug resistance; microbes as cofactors in chronic diseases
---------------------------------------------------------------------------------------------
* Adapted from reference 3.
===============================================================================================
Return to top. Figure_1 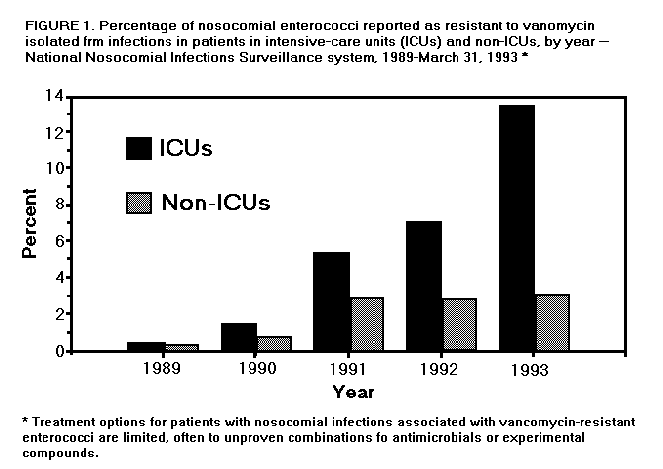 Return to top. Figure_2 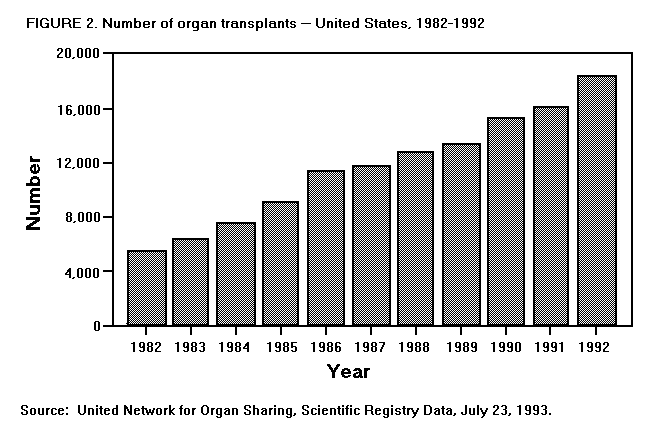 Return to top. Figure_3 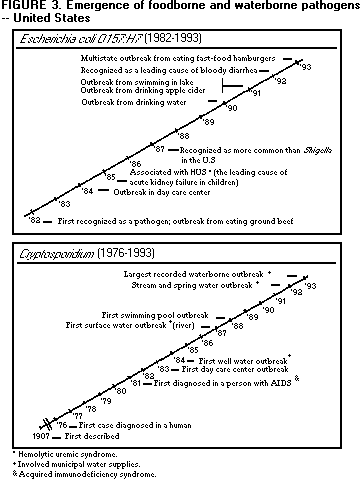 Return to top. Figure_4 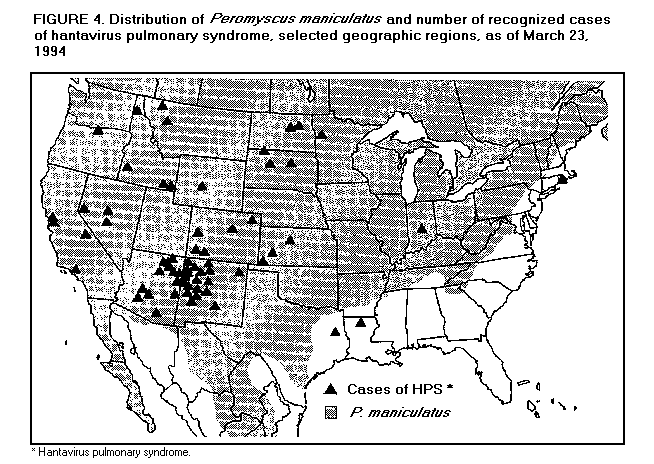 Return to top. Table_B2 Note: To print large tables and graphs users may have to change their printer settings to landscape and use a small font size.
=============================================================================
BOX 2. Summary of goals and objectives for preventing illness from emerging
infectious diseases
Goal I: Surveillance
Detect, promptly investigate, and monitor emerging pathogens, the diseases
they cause, and the factors influencing their emergence.
Objectives:
-- Expand and coordinate surveillance systems for the early detection,
tracking, and evaluation of emerging infections in the United States.
-- Develop more effective international surveillance networks for the
anticipation, recognition, control, and prevention of emerging
infectious diseases.
-- Improve surveillance and rapid laboratory identification to ensure
early detection of antimicrobial resistance.
-- Strengthen and integrate programs to monitor and prevent emerging
infections associated with food/water, new technology, and environ-
mental sources.
-- Strengthen and integrate programs to monitor, control, and prevent
emerging vector-borne and zoonotic diseases.
Goal II: Applied Research
Integrate laboratory science and epidemiology to optimize public health
practice.
Objectives:
-- Expand epidemiologic and prevention effectiveness research.
-- Improve laboratory and epidemiologic techniques for the rapid
identification of new pathogens and syndromes.
-- Ensure timely development, appropriate use, and availability of
diagnostic tests and reagents.
-- Augment rapid response capabilities for vaccine production and
delivery and expand evaluation of vaccine efficacy and the cost
effectiveness of vaccination programs.
Goal III: Prevention and Control
Enhance communication of public health information about emerging diseases
and ensure prompt implementation of prevention strategies.
Objectives:
-- Use diverse communication methods for wider and more effective
delivery of critical public health messages.
-- Establish the mechanisms and partnerships needed to ensure the rapid
and effective development and implementation of prevention measures.
Goal IV: Infrastructure
Strengthen local, state, and federal public health infrastructures to
support surveillance and implement prevention and control programs.
Objectives:
-- Ensure the ready availability of the professional expertise and
support personnel needed to better understand, monitor, and control
emerging infections.
-- Make available state-of-the-art physical resources (e.g., laboratory
space, training facilities, and equipment) needed to safely and
effectively support the preceding goals and objectives.
=============================================================================
Return to top. Table_2 Note: To print large tables and graphs users may have to change their printer settings to landscape and use a small font size.
TABLE 2. Potential projects for Emerging Infections Epidemiology and Prevention
Centers, United States
===========================================================================================
Center Projects
-----------------------------------------------------------------------------------------
Prevention
Unexplained of oppor-
deaths of tunistic Drug Febrile and
possible Foodborne infections resistance diarrheal Etiologic
infectious disease in HIV- * in nursing illness in agents of
Potential etiology in surveillance infected homes and migrant community-
center young and inner-city day care farm acquired
locations adults prevention populations facilities workers pneumonia
-----------------------------------------------------------------------------------------
Northeast X X X
Mid-Atlantic X X X X X
Southeast X X X X
South X X X X X
Midwest X X X X
Southwest X X X X
West X X X X X
Northwest X X X X X
U.S. Pacific
Islands X X X
U.S. Carib-
bean
Islands X X X
-----------------------------------------------------------------------------------------
* Human immunodeficiency virus.
===========================================================================================
Return to top. Table_B3 Note: To print large tables and graphs users may have to change their printer settings to landscape and use a small font size.
=============================================================================
BOX 3. Examples of potential members of a global consortium of
epidemiology/biomedical research programs/centers
Existing networks
-- CDC Field Epidemiology Training Programs
-- International Clinical Epidemiology Network
-- International Office of Epizootics Worldwide Information System
-- Pan American Health Organization-CDC Dengue Surveillance Laboratory
Network
-- Pan American Health Organization Polio Eradication Laboratory
Surveillance Network
-- World Health Organization Arbovirus and Hemorrhagic Fever
Collaborating Centers
-- World Health Organization Global Influenza Surveillance Network
Existing research facilities
-- Caribbean Epidemiology Centre, Trinidad
-- CDC: National Center for Infectious Diseases Field Stations (Cote
d'Ivoire, Guatemala, Puerto Rico, Kenya, Sierra Leone, and Thailand)
-- Department of Defense: U.S. Army Research Facilities (Brazil, Kenya,
Thailand) and U.S. Naval Research Facilities (Egypt, Indonesia, Peru,
Philippines)
-- Food and Agriculture Organization Reference Centers (Argentina,
Brazil, Colombia, Czech Republic, France, Germany, Hungary, Kenya,
Panama, Senegal, Spain, Sri Lanka, Thailand, United Kingdom, Uruguay,
and the United States)
-- French Scientific Research Institute (e.g., Senegal, Congo, Cote
d'Ivoire)
-- Instituto de Nutricion para Centroamerica y Panama, Guatemala
-- International Center for Diarrhoeal Disease Research, Bangladesh
-- National Institutes of Health, National Institute of Allergy and
Infectious Diseases-supported facilities (Brazil, Colombia, Israel,
Mali, Mexico, Philippines, Sudan, Uganda, Venezuela, and Zimbabwe)
-- Pasteur Institutes (e.g., Algeria, Central African Republic, French
Guiana, Iran, Madagascar, Morocco, New Caledonia, Senegal, and
Vietnam)
=============================================================================
Return to top. Table_B4 Note: To print large tables and graphs users may have to change their printer settings to landscape and use a small font size.
=============================================================================
BOX 4. Implementation: high priorities for 1994-1996
Goal I: Surveillance
-- Strengthen notifiable disease surveillance at state and local levels.
-- Establish two physician-based Sentinel Surveillance Networks to detect
and monitor emerging diseases, such as unexplained adult respiratory
distress syndrome, drug-resistant pneumococcal disease, and childhood
illnesses characterized by fever and rash.
-- Establish four population-based Emerging Infections Epidemiology and
Prevention Centers to conduct focused epidemiology/prevention projects
emphasizing foodborne and waterborne infectious diseases and
potentially vaccine-preventable diseases.
-- Strengthen and link four existing research facilities/networks for a
global consortium to promote the detection, monitoring, and
investigation of infections emerging internationally that could affect
the health of U.S. residents.
Goal II: Applied Research
-- Reestablish an extramural program to support emerging infectious
disease prevention and control activities, such as evaluating the role
of prescribing practices in the development of antimicrobial
drug-resistant pathogens.
-- Initiate prevention effectiveness studies to assess the impact of food
preparation guidelines on the incidence of foodborne infections such
as E. coli O157:H7 and Salmonella enteritidis.
Goal III: Prevention and Control
-- Develop additional means to deliver laboratory and public health
information informing health professionals about emerging infections
and antimicrobial drug resistance.
-- Develop and implement guidelines for the prevention of opportunistic
infections in immunosuppressed persons.
Goal IV: Infrastructure
-- Provide state-of-the-art training in diagnostic evaluation and testing
for medical laboratory personnel to ensure the diagnosis and surveil-
lance of emerging infections.
-- Establish a public health laboratory fellowship in infectious diseases
that will train medical microbiologists in public health approaches to
diagnosis and molecular epidemiology.
=============================================================================
Return to top. Figure_5 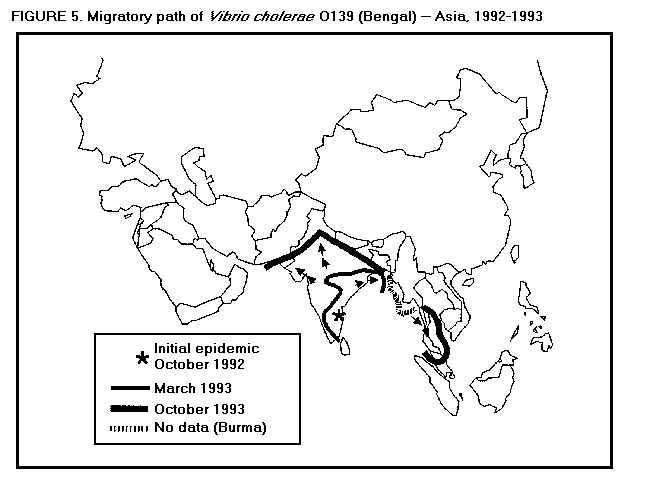 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 09/19/98 |
|||||||||
This page last reviewed 5/2/01
|