 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Increases in HIV Diagnoses --- 29 States, 1999--2002Since the advent of highly active antiretroviral therapy (HAART) in 1996, progression from receiving diagnosis of human immunodeficiency virus (HIV) infection to having acquired immunodeficiency syndrome (AIDS) has slowed substantially, making HIV-transmission patterns less predictable through AIDS surveillance alone. Consequently, CDC has recommended that states report diagnoses of HIV infections in addition to cases of AIDS (1). Recent estimates of HIV diagnoses suggested a leveling of the downward trend in HIV infections nationally and increases in HIV infections among certain populations (2). Reports of syphilis outbreaks and increased unprotected sex raised concerns regarding increases in HIV transmission among men who have sex with men (MSM) (3--5). In response to these developments, CDC analyzed trends in HIV diagnoses in 29 states* that conducted name-based HIV/AIDS surveillance during 1999--2002. This report summarizes the results of that study, which indicated that HIV diagnoses increased among men, particularly MSM, and also among non-Hispanic whites and Hispanics. The findings emphasize the need for new prevention strategies to reverse potential increases in HIV transmission among these populations. In 1994, CDC began supporting a uniform system for national, integrated HIV and AIDS surveillance. At that time, 25 states required confidential reporting of persons with HIV infection whether or not their infection had progressed to AIDS. Four additional states included in this analysis have had confidential HIV reporting since at least 1999, the year the lowest number of HIV diagnoses was reported among the original 25 states. In this analysis, persons with HIV were defined as those who received a diagnosis of HIV with or without a diagnosis of AIDS. Annual numbers of HIV diagnoses during 1999--2002 were based on the earliest reported dates of diagnosis. All analyses were adjusted for delays in reporting. Reports with no identified mode of HIV exposure were later reclassified to an exposure category (e.g., MSM, injection-drug use, MSM who inject drugs, and heterosexual contact) (6). Variance estimates and standard deviations for the annual number of HIV diagnoses were calculated, taking into account adjustments for reporting delay and reclassification to exposure categories. Variance estimates were derived from variances based on monthly data submissions to CDC (7). Year-to-year differences in the numbers of new diagnoses were considered statistically significant when 95% confidence intervals (CIs) based on calculated standard deviations did not overlap for those years. During 1999--2002, HIV infection was diagnosed in 102,590 persons in the 29 HIV-reporting states. Of these persons, 72,323 (70.5%) were male, and 30,264 (29.5%) were female (Table). Among racial/ethnic populations, the majority (56,872 [55.4%]) of HIV diagnoses were among non-Hispanic blacks, accounting for 71.8% of all diagnoses in female and 48.6% of all diagnoses in males. The remainder of the HIV diagnoses occurred primarily among non-Hispanic whites (32,077 [31.3%]), followed by Hispanics (11,829 [11.5%]). Among males, the most prevalent mode of exposure was MSM (59.7%), followed by heterosexual contact (17.8%), and injection-drug use (15.8%). Among females, the most prevalent exposure category was heterosexual contact (76.7%), followed by injection-drug use (20.3%). During 1999--2002, the number of males with new HIV diagnoses increased 7.3%, from 17,556 (95% CI = 17,412--17,701) to 18,843 (95% CI = 18,360--19,326) (Table). Among MSM, the number with new HIV diagnoses increased 17.0%, from 9,988 (95% CI = 9,733--10,243) to 11,686 (95% CI = 11,239--12,132) (Figure 1). The number of new HIV diagnoses did not change significantly during 1999--2002 among females (Table), persons exposed through heterosexual contact, injection-drug users, or MSM who inject drugs (Figure 1). Trends varied among racial/ethnic populations. During 1999--2002, the number of HIV diagnoses increased 26.2% among Hispanics, from 2,622 (95% CI = 2,566--2,678) to 3,308 (95% CI = 3,106--3,510) and 8.1% among non-Hispanic whites, from 7,716 (95% CI = 7,618--7,814) to 8,341 (95% CI = 8,016--8,665). No significant changes were observed for non-Hispanic blacks or Asians/Pacific Islanders. During 1999--2002, the number of persons in whom AIDS was diagnosed along with HIV did not change significantly (Figure 2); however, the number of persons with HIV diagnosis and no AIDS diagnosis during the same calendar month increased by 9.3%, from 18,712 (95% CI = 18,554--18,870) to 20,443 (95% CI = 19,925--20,961). Reported by: HI Hall, PhD, R Song, PhD, MT McKenna, MD, Div of HIV/AIDS Prevention, National Center for HIV, STD, and TB Prevention, CDC. Editorial Note:The increase in total HIV diagnoses during 1999--2002 reflects increases primarily among males, particularly MSM, and among non-Hispanic whites and Hispanics. The 29 states participating in these analyses did not include certain states (e.g., California, Illinois, New York, and Washington) that have reported increases among MSM in other sexually transmitted diseases (3,4). In addition, among states not participating, certain states (e.g., New York and Texas) have recently implemented confidential HIV reporting that will enable monitoring of HIV diagnoses; other states (e.g., California, Illinois, and Maryland) are implementing alternative forms of surveillance such as coded patient identifiers. Standard protocols are being developed to evaluate the performance of these alternative surveillance procedures. Nationwide reporting of HIV diagnoses would improve estimates of the size of the HIV-infected population. The findings in this report are subject to at least three limitations. First, delays in reporting were assumed to be <5 years, and reporting delays were assumed consistent within the preceding 5 years. When implemented fully, electronic laboratory reporting should decrease the time between HIV diagnosis and reporting to the surveillance system. Second, classification of cases with no identified mode of exposure into exposure categories was based on follow-up investigations. Cases with follow-up information were assumed to constitute a representative sample of all cases initially reported with no identified exposure, and the distribution among exposure categories was assumed consistent during the preceding 10 years. The validity of these estimates is being evaluated by sampling and intensive follow-up. Finally, completeness of reporting and potential duplicate reporting by different states is being evaluated in accordance with CDC's performance standards for HIV/AIDS surveillance (1). Changes in the annual number of HIV diagnoses might be affected by changes in testing patterns for HIV infection. Additional data on testing patterns are needed; new testing technologies that distinguish between recent and long-term infections will allow for better characterization of recent HIV-transmission patterns and more rapid and targeted preventive measures (8). However, population surveys suggest stable trends in testing in recent years, with approximately 45% of U.S. adults reporting they ever had an HIV test (9). In addition, because the number of simultaneous diagnoses of HIV and AIDS did not increase, the increase in HIV diagnoses more likely reflects an increase in newly infected persons rather than more intensive testing efforts. Hispanic and non-Hispanic black populations, with historically less access to treatment and prevention services, are affected disproportionately by HIV. New strategies are needed to remove access barriers to those populations and address the HIV epidemic among MSM. Advances in treatment for HIV infection can lower concern regarding AIDS and perhaps lead to an increase in high-risk sexual behaviors (5). To address these concerns, CDC's new initiative, Advancing HIV Prevention: New Strategies for a Changing Epidemic, promotes access to testing, medical care, and prevention services for all persons with HIV infection (10). CDC also is funding a series of projects regarding the prevention needs of MSM, both HIV positive and negative, and MSM who belong to racial/ethnic minority populations. References
* Alabama, Arizona, Arkansas, Colorado, Florida, Idaho, Indiana, Iowa, Louisiana, Michigan, Minnesota, Mississippi, Missouri, Nebraska, Nevada, New Jersey, New Mexico, North Carolina, North Dakota, Ohio, Oklahoma, South Carolina, South Dakota, Tennessee, Utah, Virginia, West Virginia, Wisconsin, and Wyoming.
Figure 1 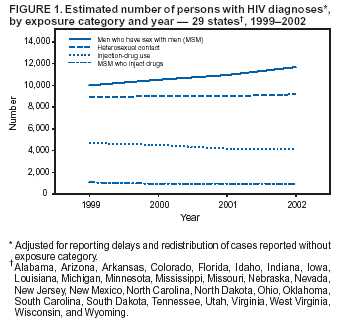 Return to top. Figure 2 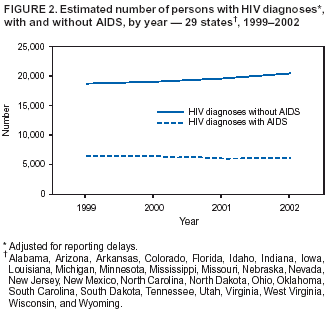 Return to top. Table 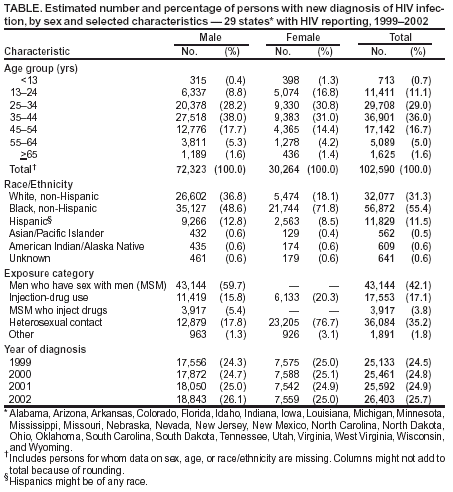 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 11/26/2003 |
|||||||||
This page last reviewed 11/26/2003
|